Abstract
Purpose
The purpose of this study was to evaluate the clinical outcomes and radiologic findings of primary total hip arthroplasty (THA) using cemented polished femoral stems.
Materials and Methods
We retrospectively reviewed 91 hips (91 patients) that had undergone primary THA with cemented polished femoral stems who were followed for at least 10 years. The mean age at surgery was 57 years (47-75 years). Mean follow up period was 12.8 years (10.1-14.0 years). Harris Hip Score (HHS) was used for clinical evaluation. Radiologic evaluation was focused on cementing technique including subsidence within the cement mantle, radiolucent lines at the cement-bone or cement-stem interface, cortical hypertrophy, and calcar resorption.
Results
The average HHS was 55.2 points before the surgery that improved to an average of 93.2 points at the final follow-up. According to Barrack classification, there were 50, 32, and 9 cases in A, B, and C grades, respectively. Subsidence of femoral stem was less than 2 mm except in one patient. There were no progressing radiolucent line or loosening of the femoral stem.
Early in the history of cemented stems in primary total hip arthroplasty (THA), unfavorable clinical outcomes were often observed due to poor cementing techniques, materials (e.g., pre-coated stems) and design (collared) of artificial joints. It is reported that failure in surgeries might be caused by incomplete filling of bone cement in the femoral canal, surface treatment of cemented femoral stems that may result in osteolysis, and femoral stem designs that put excessive stress on the cement mantle123). Subsequently, multiple studies demonstrated improved outcomes via enhancement of mechanical strength and reduction of stress on the cement mantle by using cement guns, vacuum mixing methods, and proximal/distal centralizers as well as improvement in design of femoral stems (e.g., polished, collarless, and double-tapered femoral stems)456). However, there is little information available on the long-term follow-up outcome of primary THA using cemented femoral stems in South Korea. In this study, we investigated the long-term outcome of primary THA using a femoral stems that are polished, collarless, and double-tapered.
We retrospectively reviewed 91 hips (91 patients) out of 125 hips (113 patients) who underwent primary THA with Exeter® (Howmedica International Ltd., London, UK) femoral stems (Fig. 1) in our hospital between January 1993 and December 2003. Our patients constituted of 52 men and 39 women with an average age of 57 years (45-75 years). The shortest and longest follow-up durations were 10 years and 1 month, and 14 years, respectively. The mean follow-up duration was 12.8 years. Preoperative diagnoses included avascular necrosis (38 patients), Legg-Calve-Perthes disease (13 patients), developmental hip dysplasia (10 patients), primary osteoarthritis (5 patients), and femoral neck fracture (25 patients) (Table 1).
The anterolateral approach (modified Hardinge) was used for operation. For the cementing technique, we used rasp to shape and fit the femoral marrow space and the loose cancellous bone in the proximal femur followed by pulsatile irrigation. A thin polyethylene suction pipe was inserted into the femoral marrow space and gauze soaked in hydrogen peroxide were packed to keep the area dry and prevent bleeding during the suction. After confirming the viscosity of cement, the gauze and the suction pipe were removed and the distal marrow space was blocked with an intramedullary plug. Retro-perfusion of the low-viscosity Simplex® cement (Howmedica Osteonics Co., Rutherford, NJ, USA) was performed using a cement gun. After filling the proximal part with cement, the distal part of the cement gun was removed. An inverted triangle-shaped silicon was inserted and the proximal femoral part was sealed. Pressure was applied to get an even dispersion of the cement in the femoral marrow space. The Exeter® femoral stem with a distal centralizer was inserted as depicted in Fig. 1. We did not use the vacuum mixing method in our patients. A cementless acetabular cup was used. CLS Expansion® (Sulzer Orthopaedic, Barr, Switzerland), Osteolock® (Howmedical Osteonics Co.), HGII® (Zimmer, Warsaw, IN, USA), and Spherical® (Osteonics, Allendale, NJ, USA) were used in 34, 23, 18, and 16 patients, respectively. Metal-polyethylene and zirconia- polyethylene were used for the articular surface in 76 and 15 patients, respectively. After surgery, patients completed femoral quadriceps and knee flexion exercises for 3-5 days followed by 5-7 days of wheelchair assisted walking. Up to the 6th week, partial weight bearing was allowed and full weight bearing was achieved with gradual increment of the weight load.
Harris Hip Score (HHS)7) was used for clinical evaluation. Patients were grouped as excellent, good, normal, and poor in >90, 80-89, 70-79, and <69 HHSs, respectively. We used anteroposterior and lateral images for radiologic evaluation of hips at the time of operation and throughout the final follow-up. Barrack classification1) was used for postoperative cementing technique evaluation that categorizes the patients into four grades. We measured the vertical distance of the radiolucent line of the outer shoulder of stem in zone 1 to assess subsidence of the femoral stem8). When we could not measure this distance, the change in the distance between the end of the femoral stem and the lower part of the distal centralizer was assessed (Fig. 2). As described by Gruen et al.9), the femoral stem is divided into 7 zones for monitoring and the radiolucent line is identified if the demarcation line of bone cement and femoral stem is thicker than 2 mm. Loosening of the femoral stem is classified as 'Definite Loosening', 'Probable Loosening', or 'Possible Loosening' according to the classification of Harris et al.10). We also monitored the reduction in height of the medial femoral neck (calcar) and the changes in erosion and cyst thereof. Localized endosteal bone lysis and femoral cortical hypertrophy were also analyzed. As described previously by DeLee and Charnley11), an acetabular cup is divided into 3 zones and the radiolucency between bone and the acetabluar cup is monitored along with osteolysis. We evaluated the stability of the acetabular cup according to the method of Massin et al.12) where the loosening of the acetabular cup is defined as 1) more than 5 mm displacement in radiologic images or 2) appearance of radiolucent lines including the acetabular screws. We used Spearman correlation coefficient to find out the association between postoperative complication and Barrack's classification against HHS. Clinical failure was defined as reoperation due to 1) loosening of acetabular cup, 2) loosening of femoral stem, and 3) any other clinical reasons (periprosthetic fracture, recurrent dislocation) by the end of the follow-up. The Kaplan-Meier survival analysis was performed using the SPSS program ver 12.0 (SPSS Inc., Chicago, IL, USA)13).
The average HHS was 55.2 (19-82) before the surgery that improved to an average of 93.2 (78-100) at the final follow-up. Excellent and good outcomes were found in 75 (82.4%) and 12 (13.2%) patients, respectively with only 4 (4.4%) patients in the normal group (Table 2). In postoperative imaging, 50 (54.9%) and 32 (35.2%) patients were classified as grade A and grade B, respectively, according to the Barrack classification. We identified nine patients as grade C and no one as grade D (Table 3). The average subsidence of femoral stem was 1.9 mm (0.5-4.9 mm) at the final follow-up with no subsidence of bone cement in any case. Only one patient possibly had loosening of femoral stem on the final follow-up imaging who was categorized as grade C.
Four patients had less than 2-mm reduction in height of medial femoral neck at the final follow-up. Three patients had femoral cortical hypertrophy. Loosening of the acetabular cup was found in 13 patients. Revision of the acetabular cup was performed in 9 patients (9.9%). Others were monitored without revision.
We did not find osteolysis and loosening of the femoral stem in any patient (Fig. 3). Postoperative complications included fracture of the proximal part of the femoral stem due to falling (3 patients, Vancouver type C), fracture of the femoral stem due to an unknown reason (1 patient), and recurrent dislocation due to improper positioning of the acetabular cup (2 patients). Proximal femoral stem fractures were managed with inner fixation using a metal plate with replacing a same size stem while maintaining the cement. The two patients with recurrent dislocation underwent revision of acetabular cup.
Barack classification did not significantly influence the HHS yet it was shown to be significantly lower in patients with either loosening of the acetabular cup or postoperative complications (Table 4). The Kaplan-Meier survival analysis revealed 84.6% survival rate for a total of 124 hips over 12.8 years of follow-up including 34 hips lost to follow-up (Fig. 4).
In this study, we investigated long-term clinical outcome of polished femoral stems in primary THA and found favorable outcomes from both clinical and radiologic aspects. Unlike other cement stems, the polished femoral stem (0.1µm Ra) is debonded from the bone cement and shifts toward the axis creating subsidence in the bone cement. Subsidence is mechanically critical and potentially results in favorable clinical outcomes as it contributes to improved femoral stem stability in bone cement through hoop stress.
In early bone cementing surgeries, however, 30-40% failure rate was demonstrated for primary THA in long-term follow-ups (10 years) with the failure rate being 15% in 20-year follow-ups. Such failures might be due to poor cementing technique(s), surface treatments for the femoral stems, and their designs141516). The early cementing technique is known to have poor clinical outcomes and failure as it inserts the femoral stem despite incomplete marrow filling with bone cement. This happens due to either non-sufficient bone cement filling or presence of debris and excessive removal of cancellous bone from the proximal femoral canal, followed by bleeding in the marrow space that gives rise to an inconsistent thickness in cement mantle, which should be at least 2 mm4). Barrack et al.1) claimed no loosening of the femoral stem in their 12-year radiographic review on second generation cementing techniques (e.g., use of a methylmethacrylate femoral medullary plug, delivery of a doughy mix of cement using a gun, and pulsatile irrigation). Kim et al.5) also reported excellent clinical outcomes in their 2-year follow-up of fourth generation cementing techniques (vacuum mixing method and use of proximal and distal centralizers). We implemented the second generation cementing techniques along with the use of distal centralizers in all patients. In addition, in order to achieve excellent filling of bone cement in the distal femoral part, silicon plugs were used to seal the proximal femoral part, and pressurized bone cement was filled using a cement gun16). This resulted in the absence of a radiographic postoperative boundary line between the bone cement and the femoral cortex (aka "white out"). In our nine patients who were categorized as grade C in Barrack classification, we did not find a failure in the femoral stem, which shows that the cementing technique did not attribute to this outcome. Rather, these patients were osteoporotic who are characterized by a wide marrow space and non-sufficient cancellous bone, which might have resulted in the distal dislocation of the femoral medullary plug under pressure.
Surface treatment of the femoral stem is controversial. In earlier national and international studies, favorable outcomes were shown with precoated or rough surface femoral stems. Most failures were shown in bone cement thickness of below 1 mm (C2), which is a result of poor cementing technique17181920). However, in a few investigations, higher risks of loosening of stem and osteolysis were reported with rough or precoated femoral stems, hence, polished femoral stems were recommended212223). This could be due to short life of binding between the femoral stem and the bone cement that could not last over the follow-up. In addition, debonding is unavoidable with rough and precoated stems, which eventually exacerbates the stress over the bone cement and increases the likelihood of debris formation that can facilitate osteolysis via abrasion of the bone cement. There are a few studies on polished femoral stems in South Korea. Shon et al.24) and Yim et al.25) followed up patients receiving polished femoral stems for over 5 years and did not find any aseptic loosening of femoral stem. Similarly, in the present study, we did not find aseptic loosening of the femoral stem while the subsidence of the femoral stem was approximately 1.9 mm (0.5-4.9 mm) in our 10-year follow-up. Polished femoral stems are present in a separate form from the bone cement, which allows subsidence of the femoral stem in the cement. This may result in stress relaxation that relieves the stress on the bone cement.
Carrington et al.26) showed reduction in the height of the medial femoral neck after implementation of bone cement in primary THA. The authors claimed that the reduction might be due to incomplete transfer of stem weight to the distal femur yet no association might exist with aseptic loosening. In our study, we had four patients with reduction in the height of the medial femoral neck but no loosening of stem was observed.
Cortical hypertrophy develops due to the weight load on the femoral stem on the proximal part of the femur. Particularly, it happens with large-sized femoral stems. However, subsidence of stem may be unrelated to cortical hypertrophy26). We had three patients with cortical hypertrophy who had the stem size of No 3 yet, subsidence was found to be less than 1 mm in these patients. Subsidence of the femoral stem transfers the hoop stress to bone and minimizes the stress shield. In our patients, cortical hypertrophy might be caused by imbalanced transfer of stress.
In patients undergoing revision of acetabular cup (9 patients), two had CLS expansion® and three had Osteolock®. HGII® was used in three patients and one had received Spherical®. Metal-polyethylene was the material of the articular surface in all nine patients. It appears that the position, direction of cup, and combination of the articular surface may elicit a more pronounced effect on the clinical and radiologic outcomes rather than the various type of the acetabular cup.
There are a number of limitations in our study. We retrospectively reviewed clinical and radiologic outcomes without having a matching control group. In addition, we did not include other potential factors that might have influenced the outcome including the position of the acetabular cup, size of the femoral head, degree of abrasion of the articular surface, patients' age, and physical activities.
In our study, we found favorable outcomes with polished femoral stems for primary THA in a 10-year follow-up. This might be due to debonding between the stem and the bone cement. This creates the hoop stress in bone and contributes to improved stability of the femoral stem. Therefore, THA using cemented polished femoral stems was found to have favorable outcomes in long term follow-up.
Figures and Tables
Fig. 2
Radiologic parameters about subcidence of femoral stem (red arrows at the proximal femoral shoulder and red lines in the distal centralizer).

Fig. 3
(A) This anteroposterior radiography shows Legg-Calve-Perthes disease sequalae of femoral head in a 58-year-old male. (B) The postoperative radiography shows good cement mantle (Barrck grade A). (C) After 12.4 years, the radiography shows subsidence less than 1 mm of femoral stem and no osteolysis around acetabular and femoral component.

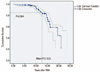
Fig. 4
At the mean follow-up (F/U) 12.8 years, the survival rate was 84.6% by Kaplan-Meier. THA, total hip arthroplasty.
References
1. Barrack RL, Mulroy RD Jr, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg Br. 1992; 74:385–389.

2. Sherfey JJ, McCalden RW. Mid-term results of Exeter vs Endurance cemented stems. J Arthroplasty. 2006; 21:1118–1123.

3. Mohler CG, Callaghan JJ, Collis DK, Johnston RC. Early loosening of the femoral component at the cement-prosthesis interface after total hip replacement. J Bone Joint Surg Am. 1995; 77:1315–1322.

4. Mulroy WF, Estok DM, Harris WH. Total hip arthroplasty with use of so-called second-generation cementing techniques. A fifteen-year-average follow-up study. J Bone Joint Surg Am. 1995; 77:1845–1852.

5. Kim SY, Baek SH, Park IH, et al. Early results of hybrid total hip arthroplasty using a fourth generation cementing technique. J Korean Hip Soc. 2003; 15:209–216.
6. Williams HD, Browne G, Gie GA, Ling RS, Timperley AJ, Wendover NA. The Exeter universal cemented femoral component at 8 to 12 years. A study of the first 325 hips. J Bone Joint Surg Br. 2002; 84:324–334.
8. Fowler JL, Gie GA, Lee AJ, Ling RS. Experience with the Exeter total hip replacement since 1970. Orthop Clin North Am. 1988; 19:477–489.
9. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; 141:17–27.
10. Harris WH, McCarthy JC Jr, O'Neill DA. Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Joint Surg Am. 1982; 64:1063–1067.

11. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; 121:20–32.

12. Massin P, Schmidt L, Engh CA. Evaluation of cementless acetabular component migration. An experimental study. J Arthroplasty. 1989; 4:245–251.
13. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958; 53:457–481.

15. Stauffer RN. Ten-year follow-up study of total hip replacement. J Bone Joint Surg Am. 1982; 64:983–990.

16. Sutherland CJ, Wilde AH, Borden LS, Marks KE. A tenyear follow-up of one hundred consecutive Müller curved-stem total hip-replacement arthroplasties. J Bone Joint Surg Am. 1982; 64:970–982.

17. Schulte KR, Callaghan JJ, Kelley SS, Johnston RC. The outcome of Charnley total hip arthroplasty with cement after a minimum twenty-year follow-up. The results of one surgeon. J Bone Joint Surg Am. 1993; 75:961–975.

18. Oh I, Bourne RB, Harris WH. The femoral cement compactor. An improvement in cementing technique in total hip replacement. J Bone Joint Surg Am. 1983; 65:1335–1338.

19. Shon WY, Hur CY, Moon JG, Nam HW, Lee YK, Choi JH. 3-5 years results of cemented Versys-TM® femoral stem. J Korean Hip Soc. 2004; 16:317–323.
20. Suh DH, Yun HH, Chun SK, Shon WY. Fifteen-year results of precoated femoral stem in primary hybrid total hip arthroplasty. Clin Orthop Surg. 2013; 5:110–117.

21. Harris WH. Long-term results of cemented femoral stems with roughened precoated surfaces. Clin Orthop Relat Res. 1998; 355:137–143.

22. Sporer SM, Callaghan JJ, Olejniczak JP, Goetz DD, Johnston RC. The effects of surface roughness and polymethylmethacrylate precoating on the radiographic and clinical results of the Iowa hip prosthesis. A study of patients less than fifty years old. J Bone Joint Surg Am. 1999; 81:481–492.

23. Collis DK, Mohler CG. Comparison of clinical outcomes in total hip arthroplasty using rough and polished cemented stems with essentially the same geometry. J Bone Joint Surg Am. 2002; 84-A:586–592.

24. Shon WY, Hur CY, Moon JG, Han SW, Yang JH, Jang KM. 2-5 year results of the cemented polished Versys Heritage® femoral stem. J Korean Orthop Assoc. 2008; 43:9–16.

25. Yim SJ, Woo SH, Kim MY, et al. Total hip arthroplasty using Exeter stem. J Korean Hip Soc. 2005; 17:195–200.
26. Carrington NC, Sierra RJ, Gie GA, Hubble MJ, Timperley AJ, Howell JR. The Exeter Universal cemented femoral component at 15 to 17 years: an update on the first 325 hips. J Bone Joint Surg Br. 2009; 91:730–737.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download