Iliosacral screw fixation is used for treatments of sacral fractures, spino-pelvic dissociation, and unstable posterior pelvic ring injuries. The percutaneous approach is gaining popularity12). Most complications of percutaneous iliosacral screw fixation are related to improper insertion of iliosacral screws. They are commonly characterized by fifth lumbar and first sacral nerve root damages as well as injury to iliac vessels anterior to the sacral wing234). Other iatrogenic complications are frequently reported along with an increased popularity of this fixation method. We report a case of superior gluteal artery injury during percutaneous bilateral iliosacral screw fixation for treatment of sacral fracture of spino-pelvic dissociation. This complication was managed using angiographic arterial embolization. Here, we discuss the cause, prevention and treatment of superior gluteal artery injury along with a review of literature.
CASE REPORT
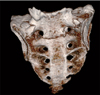
A 68-year-old man was brought to the emergency room with pelvic pain after an accident with a motorcycle. No open wound was observed on pelvic examination and the patients had no tenderness on the anterior pelvis. However, the patient complained from severe tenderness on the lumbosacral junction with limited mobility due to extreme pain. Motor and sensory functions and circulation of the lower extremity were normal without any neurological symptoms. In the plain radiographs, bilateral vertical fractures were observed on the upper aspect of the first sacral foramen (Fig. 1). In three-dimension reconstruction computed tomography (CT), bilateral vertical fractures on Zone II of the first sacrum with communition of the anterior cortex was observed. This U-shaped fracture passed through the first sacral foramen to connect through the first and second sacral vertebrae (Fig. 2). This sacral fracture of spino-pelvic dissociation was relatively stable because the comminuted fragment was small and not displaced. To achieve early ambulation, we scheduled percutaneous iliosacral screw fixation.
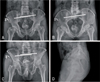
Under general anesthesia, the patient was placed on a radiolucent table in the supine position with pelvic support using multiple layers of operation drapes on the sacral region to relax the gluteal muscles. A true lateral image of the pelvis was obtained with an overlap of both greater sciatic notches using a C-arm image intensifier. After localizing the safe area, a 1-cm incision was made on the left gluteal area on the central upper part of the first sacrum and posterior to the ilio-cortical line in the lateral image. Muscular areas were widened with a straight hemostatic forceps to reach the outer cortex of the iliac bone. Then, a guide pin sleeve was introduced to reach the outer cortex of the iliac bone to subsequently place a horizontal 3.2-mm-sized guide pin on the safe area of the first sacrum (Fig. 3A). It was then passed through the opposite side of the first sacral body under monitoring of the pelvic inlet and outlet views with a C-arm image intensifier. In sequence, a 1-cm skin incision was made on the corresponding right gluteal area and a guide pin sleeve was inserted using the same method. A guide pin was placed 7 mm posterior and inferior to the left guide pin (Fig. 3B). It was completed with insertion of the pin into the opposite side of the first sacral body under C-arm guide (Fig. 3C). In the next step, reaming was performed along the right postero-inferior guide pin with a 5 mm cannulated reamer (Fig. 3D), bright red arterial bleeding was noted when the reamer was retrieved. The bleeding site was packed with gauze but the bleeding could not be controlled. Since the vital signs of the patients were stable, a full threaded 120-mm-long, 7.0-mm-diameter cannulated screw (Zimmer®, Warsaw, IN, USA) was inserted and gauze packing was applied. A same size cannulated screw was inserted towards the center of the first sacral body through the guide pin that was introduced from the opposite side. After reaming, no arterial bleeding was observed on the left side (Fig. 3F). The left incision was closed but arterial bleeding continued on the right side after removal of gauze. We tried to find the bleeding site by gentle exploration, which turned to be unsuccessful. Therefore, the incision was temporarily closed after gauze packing and the patient was immediately transferred to the angiography room.
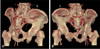
Through the left femoral artery, a guide catheter was introduced along the right internal iliac artery to perform right superior gluteal artery angiography. Arterial bleeding was localized to the upper branch of the deep branch of the right superior gluteal artery (Fig. 4A), which was adjacent to the insertion site and the extension line of the right iliosacral screw. Arterial embolization and bleeding control was achieved by coiling of the deep branch of the right superior gluteal artery (Fig. 4B). The patient had well-controlled vital signs throughout the whole procedure. Post-operative AP, inlet/outlet and lateral pelvic radiographs confirmed proper-positioned iliosacral screws on both sides. No fracture displacement was seen (Fig. 5A-D). In CT imaging, both iliosacral screws were not invading the first sacral foramen and were positioned in the safe area. Screws had passed the opposite side of the sacral fracture but had not crossed the opposite sacral wing. The left antero-superior iliosacral screw was positioned from the postero-superior aspect of the left iliac cortex along an antero-inferior direction towards the opposite sacrum. The right postero-inferior iliosacral screw was laid from the antero-inferior aspect of the right iliac cortex along a postero-superior direction towards the opposite first sacral body. Three-dimension reconstructed CT angiography showed that the head of the right side screw is in close proximity to the deep branch of the superior gluteal artery (Fig. 6A); however, there was comparatively more space between the screw head and the deep branch of the superior gluteal artery on the left (Fig. 6B).
On the following day, right-sided packed gauzes were removed under local anesthesia and no bleeding was noted. The skin incision was closed and the patient recovered without any noticeable complication.
DISCUSSION
Percutaneous iliosacral screw fixation for sacral fractures or sacroiliac joint injuries is gaining increased popularity in treatment of unstable posterior pelvic ring injuries. This is primarily due to advantages that include reduced time of operation and anesthesia, and lower rates of bleeding, infection, and wound problem, while a strong fixation and lower rate of fracture non-union is ensured. However, other complications are being reported which include spinal nerve root damage and vascular injury due to improper positioning of the screws12345).
Superior gluteal artery injury is not a common complication and is limited to a few case reports on superior gluteal artery injury during the procedure67), and post-operative development of pseudoaneurysms of the superior gluteal artery89). Like the described complication in our case, the upper branch of the deep branch of the superior gluteal artery is more likely to be injured by iliosacral screw fixation, as it is located along the posterior ilium in the upper part of greater sciatic notch5). Although the incidence of procedural superior gluteal artery injury is very low, ranging 0.6-1.2%37), Collinge et al.5) reported a relatively high incidence of superior gluteal artery injury in a study on cadaver. They found injuries in 10 out of 58 cases of percutaneous iliosacral screw fixation (18%). The injuries were either direct neurovascular damages due to screw insertion or partial entrapment of the neurovascular structure between the screw head and the iliac bone despite use of cannulated sleeves to protect the soft tissue and appropriately inserted the screw. The limitations of this study are its cadaveric nature with hard and less mobile tissues and inclusion of the whole bundle of the superior gluteal vessels and nerves, which can lead to a reportedly higher incidence of injury in comparison to the living human body.
Predisposing factors of superior gluteal arterial damage include calcification of intrapelvic arteries6), and aberrant anatomical structures of deep branches of superior gluteal arteries7), yet it is primarily attributed to traction injuries or direct injury with screws, drill sleeve, and drill678). Stephen8) pointed that the use of large sized guide pin could be one of the reasons of superior gluteal artery injuries. Other factors that may have contributed to an increased likelihood of superior gluteal artery injuries are attempted insertion of a guide pin into the distal part further from the insertion position of final screw and multiple attempts to insert the guide pin to achieve the ideal position for the screws. In our patient, we used a 3.2-mm guide pin without any bleeding as we used a guide pin sleeve, yet bleeding happened right after removal of the reaming drill. The reaming drill was used without a reaming drill sleeve, as it was not ready on the day of operation. This narrows the primary reason of bleeding in our patient to the injury of superior gluteal artery branches by the reaming drill. Since we introduced bilateral 7-mm-diameter iliosacral screws reaching the opposite side of the first sacral body, the second guide pin was located postero-inferior to the first guide pin in a 7-mm-distance into the safe area without an overlap. The direction of insertion of the second iliosacral screw ran from the antero-inferior of the iliac cortex towards the postero-superior aspect of the sacral body, which makes the guide pin more antero-inferior in the muscular layer of outer pelvis compared to the opposite guide pin. This placed the guide pin closer to the deep branch of the superior gluteal artery and possibly led to vascular injury during the reaming (Fig. 6).
It is reported that tamponade with gauzes had not been effective to stop bleeding associated with superior gluteal artery injury during percutaneous iliosacral screw fixation6). Although Rysavý et al.3) reported the treatment of this injury with extension of the incision and ligation of the bleeding arteries, exploration of the exact bleeding site through extended incision is difficult7). It is preferred to use arterial embolization to stop bleeding after confirming the bleeding sites by angiography6789). In our patient, similarly, gauze packing was ineffective to control bleeding thus arterial coil embolization was used after confirmation of the bleeding site by angiography.
Routt et al.2) recommended soft tissue protective tools or sleeves for guide pin, drill, tap and screw insertion during percutaneous iliosacral screw fixation to minimize superior gluteal artery damage. Stephen8) recommended that the insertion site of the iliosacral screws should be determined with guide pins less than 2 mm to be later replaced by larger guide pins. Additionally, 6.5- or 7.0-mm cannulated screws are suggested as they allow introduction of smaller guide wires. On the other hand, Collinge et al.5) suggested slightly wider skin incision, use of trocar-tipped drill sleeve systems to protect soft tissues, and gentle retraction of the deep soft tissues on the outer side of periosteum before introduction of the drill.
We presented a patient who had superior gluteal artery injury during bilateral percutaneous iliosacral screw fixation of sacral fracture of spino-pelvic dissociation who was treated with arterial embolization. Orthopedic surgeons are strongly recommended to use sleeves for a guide pin as well as drill to minimize the potential damage of the superior gluteal blood vessels. We should also highlight the importance of accurate iliosacral screw insertion based on anatomical parameters using a shading scanner. Immediate angiography and arterial embolization is necessary to locate the bleeding site and control the unexpected bleeding. Higher risk of superior gluteal artery injury is expected when a guide pin is placed in the antero-inferior aspect of the outer pelvis as it is positioned adjacent to the deep branch of the superior gluteal artery. More anatomical investigation of the safe area is warranted to avoid superior gluteal neuro-vascular damage during percutaneous iliosacral screw fixation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download