Abstract
Purpose
In comminuted intertrochanteric fractures, various operative options have been introduced. The purpose of this study was to determine whether there were differences in clinical and radiologic outcomes among bipolar hemiarthroplasty (BH), compression hip screw (CHS) and proximal femur nail antirotation (PFNA) in treating comminuted intertrochanteric fractures (AO/OTA classification, A2 [22, 23])
Materials and Methods
We retrospectively evaluated total 150 patients (BH, 50; CHS, 50; PFNA, 50) who were operated due to intertrochanteric fractures from March 2010 to December 2012 and were older than 65 years at the time of surgery. We compared these three groups for radiologic and clinical outcomes at 12 months postoperatively, including Harris Hip Score, mobility (Koval stage), visual analogue scale and radiologic limb length discrepancy (shortening).
Results
There was no statistical significance among three groups in clinical outcomes including Harris Hip Score, mobility (Koval stage), visual analogue scale. However, there was significant differences in radiologic limb discrepancy in plain radiographs at 12 months postoperatively (radiologic shortening: BH, 2.3 mm; CHS, 5.1 mm; PFNA, 3.0 mm; P=0.000).
In comminuted intertrochanteric fractures, various operative options have been introduced12345678). However, the optimal treatment for unstable intertrochanteric fractures in elderly patients remains controversial. Traditionally, intertrochanteric fractures were operated with a sliding hip screw with a side plate. In the early 1990s, a new method of an intramedullary nail in the proximal femur with an interlocking screw in the femoral head was introduced29). In cases of unstable intertrochanteric fracture in the elderly, osteoporosis and comminution often result in delayed full weight-bearing and a high rate of complications that are treated with internal flxation including compression hip screw (CHS) and proximal femur nail antirotation (PFNA)210). Recently, many reports in the literature consider that prosthetic replacement is the preferred treatment for selected unstable comminuted intertrochanteric fractures in the elderly1112). However, unlike a femoral neck fracture, an intertrochanteric fracture has a good blood supply, ensuring bone healing in the case of proper flxation. Also, arthroplasty has a number of disadvantages, including greater blood loss, increased operation time and greater soft tissue injury, which are especially important issues in elderly patients8). The purpose of this study was to determine whether there were differences in clinical and radiologic outcomes among bipolar hemiarthroplasty (BH), CHS and PFNA in treating comminuted intertrochanteric fractures (AO/OTA classification, A2 [22, 23]) at postoperative 1 year.
The Institutional Review Board of Soonchunhyang University Cheonan Hospital approved the design and protocol of this study. From March 2010 to December 2012, total of 150 restrospective consecutive patients were enrolled to perform this study in three groups-BH, 50 cases; CHS, 50 cases; PFNA, 50 cases. All patients were older than 65 years at the time of surgery. The inclusion criteria were: unstable intertrochanteric fractures (AO/OTA classification, A2 [22, 23]), no contraindication to anesthesia, and pre-injury independent walking with or without aids. The exclusion criteria were: reoperation, expire and follow up loss within postoperative 1 year, suspected pathological fracture, significant senile dementia, and osteoarthritis or rheumatoid arthritis in the fractured hip.
The demographic characteristics of the 150 patients are summarized in Table 1. The BH group included 20 males and 30 females with a mean age of 81.8 years old (standard deviation [SD], 6.9; range, 71-101 years old), the CHS group included 21 males and 29 females with a mean age of 77.3 years (SD, 8.8; range, 65-93 years old), and the PFNA group included 21 males and 29 females with a mean age of 73.8 years (SD, 9.5; range, 65-94 years old). There was significant differences in the mean age among these three groups, but there were no significances in the body mass index and dual energy absorptiometry (Table 1).
All operation was performed by two senior surgeons. BH and CHS were performed by YSS and PFNA were performed by JSP, because of surgeon's preference for unstable intertrochanteric fractures in same center. The prosthesis for BH was the Bencox stem and the Corenbipolar cup (Corentec, Seoul, Korea). Osteosynthesis was performed using CHS (Dynamic hip screw system; Tradimedics, Seongnam, Korea) and PFNA (Synthes, Solothurn, Switzerland).
At postoperative 1 year, the functional outcome was evaluated using Harris Hip Score (HHS)13) and the degree of pain was measured by visual analogue scale (VAS)13). Pain while walking was assessed on a VAS (0 to 100) and scores exceeding thirty were regarded as substantial pain. Mobility were evaluated by use of the Koval classiflcation1415), which grades ambulatory ability as independent community ambulatory (grade 1), community ambulatory with cane (grade 2), community ambulatory with walker or crutches (grade 3), independent household ambulatory (grade 4), household ambulatory with cane (grade 5), household ambulatory with walker or crutches (grade 6), and nonfunctional ambulatory (grade 7). Anteroposterior radiographs of the hip were taken at each follow-up for the evidence of union, subsidence of the stem, migration of internal fixation, and heterotopic ossification, ipsilateral limb length discrepancy (LLD) for radiologic shortening was checked at each group. All radiographs were taken in the same department using a standardized protocol. Anteroposterior radiographs of the hip were obtained in the supine position at a source-to-film distance of 110 cm with the x-ray beam centered on the superior aspect of the pubic symphysis and perpendicular to the patient16).
Radiologic outcome was evaluated by ipsilateral LLD between immediate postoperative length and length of postoperative 1 year after adjusting difference of magnification. Each LLD was checked from hip center to wiring area of lesser trochanter (or distal tip of lesser trochanter, if there was no wiring) in BH (Fig. 1), from hip center to first proximal screw in CHS (Fig. 2), and from hip center to distal locking screw in PFNA (A, postoperative length; A', length of postoperative 1 year) (Fig. 3). Magnification adjustment were performed using the ratio of stem length between postoperative length and length of postoperative 1 year (B, postoperative stem length; B', the length of stem at postoperative 1 year) in BH. In CHS, the length of plate was used to adjust difference of magnification (B, postoperative plate length; B', the length of plate at postoperative 1 year). In PFNA, the length of nail was used to adjust difference of magnification (B, postoperative nail length; B', the length of nail at postoperative 1 year). Shortening of limb length was adjusted considering difference of magnification. All measurements on radiographs were subsequently made on a 19 inch LCD monitor.
*Radiologic LLD (shortening)= [A×(B'/B)]-A'
Baseline patient characteristics and perioperative clinical data were analyzed for all patients, and by gender and operation type with descriptive statistics. Bi-variable tests of association were based on either Pearson's chi-square or Fisher's exact tests for categorical variables. A robust analysis of variance (ANOVA) was used for continuous variables and the Kruskal-Wallis test was used for for ordinal variables. All tests were two-sided, and statistical significance was accepted for a P-value of <0.05, and statistical analysis was performed using SPSS statistical software (version 16; SPSS Inc., Chicago, IL, USA).
In clinical outcomes, the mean HHS of BH was 73±17, the mean HHS of CHS was 71±19, and the mean HHS of PFNA 74±15. The mean Koval score of BH was 2.8±1.7, the mean Koval score of CHS was 3.0±2.3, and the the mean Koval score of PFNA was 2.5±2.2. The mean VAS score was 2.8±3.8 in BH group, 2.8±3.6 in CHS group, and 3.0±4.1 in PFNA group. There were no significances in clinical outcome including HHS, the Koval score, and the VAS score among these three groups (Table 2).
In radiologic outcomes, there was significant differences in radiologic limb discrepancy in plain radiographs at 12 months postoperatively (radiologic shortening: BH group, 2.3±3.7 mm; CHS group, 5.1±6.3 mm; PFNA group, 3.0 ±4.1 mm; P=0.000) (Table 2).
All of the 150 patients achieved fracture union without fixation loss or stem loosening, and there were no cases of infection, heterotrophic ossification.
Intertrochanteric hip fractures account for approximately half of all hip fractures in the elderly population17). Among these fractures, 50-60% are classifled as unstable618192021). Several methods of operation have been proposed for the management of intertrochanteric fractures67192021). However, the choice of surgical options for intertrochanteric fractures is controversial6). In this study, we evaluated clinical outcomes and radiological outcomes for intertrochanteric fracture by operation type. There are various reports comparing clinical outcome, but few reports published for radiological outcome after 1 year postoperatively24891022).
It is very obvious advantages and disadvantages for each method. The BH with full coated stem, initial stability and long-term biologic fixation can be obtained even in osteoporotic proximal femur with large bone defect1123). The BH had a significantly shorter time to beginning weight-bearing. However, BH was associated with significantly longer operation time, intraoperative blood loss, intraoperative blood salvage, and total volume of blood transfused than internal fixation23). CHS can provide satisfactory flxation, but failure rates of 4-20% have been reported in the treatment of intertrochanteric fractures112224). Intramedullary flxation using PFNA has the theoretical advantages of closed insertion through a small incision and a shorter lever arm, which reduces the risk of fatigue failure of the implant25). However, its main drawback is the possibility of femoral shaft fracture, especially at the site of the distal locking screw hole826). Because internal fixation of unstable intertrochanteric fractures in osteoporotic patients necessitates a prolonged period of protected weight bearing and is frequently associated with problems such as loss of fixation, nonunion, and cut-out of the lag screw in CHS and PFNA. Varus collapse and shortening are mechanical complications of unstable or severely osteoporotic intertrochanteric fractures19). However, in spite of these problems, it is very important advantage to preserve normal joint and bone viability in CHS and PFNA.
Several limitations of the present study should be considered. First, other important factors for clinical and radiological outcomes were not evaluated, such as demographic characteristics about preinjury ambulatory state and instability risk and, radiographic findings about the defect of posteromedial cortex, extension to subtrochanteric area, presence of osteoporosis. Second, preoperative true limb length could not investigated, and radiologic landmarks to adjust magnification could be checked ambiguously by the patient position. Thrid, we could not evaluate the clinical and radiological outcomes such as complications after operation.
Although there was no significant differences in clinical outcomes among three groups at postoperative 1 year, notable differences were observed in LLD according to selection of operative methods (BH<PFNA<CHS). Meaningful shortening could be originated during fracture healing in osteosynthesis, compared to arthroplasty, and that could induce limping.
Figures and Tables
Fig. 1
Radiologic outcome was evaluated by limb length discrepancy after adjusting difference of magnification. Shortening was checked from hip center to wiring area of lesser trochanter (or distal tip of lesser trochanter, if there was no wiring) in bipolar hemiarthroplasty. A: postoperative length, A': length of postoperative 1 year, B: postoperative stem length, B': the length of stem at postoperative 1 year.

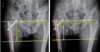
Fig. 2
Radiologic shortening was checked from hip center to first proximal screw in compression hip screw. A: postoperative length, A': length of postoperative 1 year, B: postoperative plate length, B': the length of plate at postoperative 1 year.

Fig. 3
Radiologic shortening was checked from hip center to distal locking screw in proximal femur nail antirotation. A: postoperative length, A': length of postoperative 1 year, B: postoperative nail length, B': the length of nail at postoperative 1 year.
References
1. Carpentier K, Govaers K. Internal fixation of an intertrochanteric femoral fracture after Birmingham hip resurfacing arthroplasty. Acta Orthop Belg. 2012; 78:275–278.
2. Anglen JO, Weinstein JN. American Board of Orthopaedic Surgery Research Committee. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008; 90:700–707.

3. Kreder HJ. Principles and evidence: The optimal treatment of pertrochanteric hip fractures: Commentary on an article by Kjell Matre, MD, et al.: "TRIGEN INTERTAN intramedullary nail versus sliding hip screw. A prospective, randomized multicenter study on pain, function, and complications in 684 patients with an intertrochanteric or subtrochanteric fracture and one year of follow-up". J Bone Joint Surg Am. 2013; 95:e16(1-2).
4. Matre K, Vinje T, Havelin LI, et al. TRIGEN INTERTAN intramedullary nail versus sliding hip screw: a prospective, randomized multicenter study on pain, function, and complications in 684 patients with an intertrochanteric or subtrochanteric fracture and one year of follow-up. J Bone Joint Surg Am. 2013; 95:200–208.
5. Swart E, Makhni EC, Macaulay W, Rosenwasser MP, Bozic KJ. Cost-effectiveness analysis of fixation options for intertrochanteric hip fractures. J Bone Joint Surg Am. 2014; 96:1612–1620.

6. Lee YK, Yoon BH, Nho JH, Kim KC, Ha YC, Koo KH. National trends of surgical treatment for intertrochanteric fractures in Korea. J Korean Med Sci. 2013; 28:1407–1408.

7. Guo Q, Shen Y, Zong Z, et al. Percutaneous compression plate versus proximal femoral nail anti-rotation in treating elderly patients with intertrochanteric fractures: a prospective randomized study. J Orthop Sci. 2013; 18:977–986.

8. Shen J, Wang DL, Chen GX, et al. Bipolar hemiarthroplasty compared with internal fixation for unstable intertrochanteric fractures in elderly patients. J Orthop Sci. 2012; 17:722–729.

9. Parker MJ, Bowers TR, Pryor GA. Sliding hip screw versus the Targon PF nail in the treatment of trochanteric fractures of the hip: a randomised trial of 600 fractures. J Bone Joint Surg Br. 2012; 94:391–397.
10. Chen YT, Chen WM, Lee KS, Huang CK, Chiang CC, Chen TH. Diaphyseal locking hip arthroplasty for treatment of failed fixation of intertrochanteric hip fractures. J Arthroplasty. 2008; 23:241–246.

11. Lee YK, Ha YC, Chang BK, Kim KC, Kim TY, Koo KH. Cementless bipolar hemiarthroplasty using a hydroxyapatite -coated long stem for osteoporotic unstable intertrochanteric fractures. J Arthroplasty. 2011; 26:626–632.

12. Choy WS, Ahn JH, Ko JH, Kam BS, Lee DH. Cementless bipolar hemiarthroplasty for unstable intertrochanteric fractures in elderly patients. Clin Orthop Surg. 2010; 2:221–226.

13. Maxwell C. Sensitivity and accuracy of the visual analogue scale: a psycho-physical classroom experiment. Br J Clin Pharmacol. 1978; 6:15–24.

14. Koval KJ, Zuckerman JD. Functional recovery after fracture of the hip. J Bone Joint Surg Am. 1994; 76:751–758.

15. Koval KJ, Aharonoff GB, Rosenberg AD, Bernstein RL, Zuckerman JD. Functional outcome after hip fracture. Effect of general versus regional anesthesia. Clin Orthop Relat Res. 1998; 348:37–41.
16. Nho JH, Lee YK, Kim HJ, Ha YC, Suh YS, Koo KH. Reliability and validity of measuring version of the acetabular component. J Bone Joint Surg Br. 2012; 94:32–36.

17. Egol KA, Marcano AI, Lewis L, Tejwani NC, McLaurin TM, Davidovitch RI. Can the use of an evidence-based algorithm for the treatment of intertrochanteric fractures of the hip maintain quality at a reduced cost? Bone Joint J. 2014; 96:1192–1197.

18. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995; 77:1058–1064.

19. Kazemian GH, Manafi AR, Najafi F, Najafi MA. Treatment of intertrochanteric fractures in elderly highrisk patients: dynamic hip screw vs. external fixation. Injury. 2014; 45:568–572.

20. Lee YK, Chung CY, Park MS, Lee KM, Koo KH. Intramedullary nail versus extramedullary plate fixation for unstable intertrochanteric fractures: decision analysis. Arch Orthop Trauma Surg. 2013; 133:961–968.

21. Cole PA, Bhandari M. What's new in orthopaedic trauma. J Bone Joint Surg Am. 2006; 88:2545–2561.

22. Shen L, Zhang Y, Shen Y, Cui Z. Antirotation proximal femoral nail versus dynamic hip screw for intertrochanteric fractures: a meta-analysis of randomized controlled studies. Orthop Traumatol Surg Res. 2013; 99:377–383.

23. Chang Q, Liu S, Guan C, Yu F, Wu S, Jiang C. Bipolar hip arthroplasty. J Arthroplasty. 2011; 26:1455–1459.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download