Bone marrow edema syndrome (BMES) is a rare condition characterized by pain that mainly affects the hip and which can be aggravated by ambulation. BMES was first described by Curtiss and Kincaid in 19591), but the etiology and natural history of BMES still remain unclear because epidemiological studies have not been sufficiently undertaken2). BMES typically occurs in women during late pregnancy or middle-aged men between 40-60 years old, and often disappears spontaneously after pain persists for several weeks to months2). Although magnetic resonance imaging (MRI) usually reveals low to intermediate signal intensity on T1-weighted images and high signal intensity on T2-weighted images in the femoral head, neck, and greater and lesser trochanteric area, MRI findings in patients with BMES are often non-specific. Thus, differential diagnosis of this condition can be a challenge3). Previous studies have reported several cases with unilateral BMES, but there are few case reports on bilateral BMES4). In the Korean literature, this is the first case report, to our knowledge, on bilateral BMES with different onset times. The authors experienced this rare case of rapid, spontaneous regression of symptoms treated conservatively by administering non-steroidal anti-inflammatory drugs (NSAIDs), and we report this case as it may be considered valuable for basic research relating to the pathogenesis of BMES.
CASE REPORT
A 52-year old man visited our hospital complaining of pain in the right hip and gait disturbance beginning one month prior without any traumatic injury. The patient, a policeman, spent about 45 minutes a day for a year commuting to work until the pain started. He had no history of regular exercise and the pain gradually worsened. He was able to do level-ground walking until admission, but had progressive discomfort while ascending stairs and his gait disturbance developed to the degree of being limited to walking no higher than a single story.
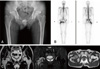
Physical examination revealed no limitations to range of motion and the patient was negative for Patrick's test and signs of impingement. No local heating sense or erythema around involved side was observed, and systemic symptoms indicating infectious condition were not present. There was no specific finding in plain radiography of the hip joints, but increased uptake of the radioactive isotope was detected in the right femoral head in technetium-99m nuclear medicine imaging. Non-enhanced MRI of the hip joints revealed low signal intensity on T-1 weighted images and high signal intensity on T-2 weighted images in the right femoral head, neck, marrow of the proximal metaphysis, and surrounding soft-tissue edema. In addition, about 1.5 cm-long fluid collection was observed in the iliopsoas muscle (Fig. 1). Blood cell counts, liver and renal functional tests and a serum electrolyte test revealed normal results, a white blood cell count of 8,600/µL (normal range, 4,000-10,000/µL), 63% segmented neutrophils (normal range, 40-80%), an erythrocyte sedimentation rate of 5 mm/hr (normal range, 0-15 mm/hr), and a C-reactive protein of 0.02 mg/dL (normal range, 0-0.5 mg/dL), excluding a uric acid of 8.1 mg/dL (normal range, 4.0-7.0 mg/dL). Since there was no evidence of bone tumor or malignancy, the patient was diagnosed with BMES. T-score was –2.3 (bone mineral density [BMD] 0.770 g/cm2) in the L4 according to lumbar spine BMD using dual energy X-ray absorptiometry (DEXA).
We planned to perform femoral head core decompression if symptoms worsen and followed up with the patient every other week concurrent with oral administration of NSAIDs (aceclofenac 100 mg, twice a day; 8 weeks) and limited physical activity. Follow-up MRI was performed 2 and 3 months after symptoms started. Although the hip pain and gait disturbance were improved from the 6th week after onset of symptoms, no changes were observed between MRI scans taken initially and 2 months after presenting symptoms. The patient showed more than 90% improvement 3 months after symptoms started. Follow-up MRI presented significantly decreased signal intensity in bone marrow and soft tissues compared to the previous MRI scan and fluid collection within the iliopsoas muscle decreased (Fig. 2). The patient returned to daily activities 5 months after onset of disease without pain and no physical limitation was present. For the following 3 years, the patient made no visits to our hospital.
After 3 years, however, the patient was re-admitted with newly developed left hip pain that had persisted for the previous 3 weeks without a history of trauma. The patient reported experiencing no discomfort for 3 years after remittance and no change in occupation or daily activities. As a daily routine, he commuted to work the same distance. No definitive abnormal findings were shown in plain radiography of the hip joints, and MRI showed low signal intensity on T1-weighted images in the left femoral head, neck, and greater and lesser trochanteric area, and high signal intensity (representing bone marrow edema on T2-weighted images. Previously observed fluid collection in the right side was not found in the iliopsoas muscle (Fig. 3). Excluding fluid collection in the iliopsoas muscle, when compared to previous MRI findings on the right side, the involved lesion area and signal intensity had similar patterns. Using the DEXA test, the T-score was –2.3 (BMD 0.760 g/cm2) in the L4 and –1.2 (BMD 0.776 g/cm2) in the left femoral neck. There was no evidence of infectious or other diseases.
The patient was administered, administered NSAIDs (aceclofenac 100 mg, twice a day; 4 weeks) and advised to avoid excessive physical activity again. His pain and gait disturbance began to improve and completely resolved 2 months after onset of symptoms. Bone marrow edema detected in the left femoral area disappeared completely (Fig. 4). The patient was satisfied with treatment and returned to normal daily activities, and no abnormal findings were found six months after symptoms started.
DISCUSSION
Bone marrow edema syndrome (BMES) is a rare disease of unknown etiology that needs to be differentiated from other conditions among patients complaining of hip pain. According to Resnick and Niwayama5), BMES is assumed to be associated with neurovascular problems, reflex sympathetic dystrophy, ischemic necrosis and others. Although there is a controversy about progression from BMES to avascular necrosis of the femoral head among researchers, the presence of osteonecrosis when bone marrow edema is observed is known as an important factor for treatment and a predictor of disease progression. According to Solomon2), bone marrow edema without osteonecrosis is characterized by hypervascularity and spontaneous regression; however, the condition associated with osteonecrosis may progress to ischemic injury with femoral head collapse and joint destruction2). Moreover, MRI is used as a modality in confirming initial diagnosis and for follow-up as it may provide definite findings3). The patient in this case report was diagnosed with BMES based on the presence of bone marrow edema without osteonecrosis.
Since BMES is a self-limiting condition, conservative management should be initiated first6). Conservative therapy includes non-weight bearing, immobilisation of the affected area, and pain management using medications such as NSAIDs and opiates7). In addition to analgesics, steroids, bisphosphonates and calcium channel blockers can be administered7), high energy extracorporeal shock wave therapy can be used when treating severe or chronic pain6), or core decompression can be performed to prevent progression to osteonecrosis if pain and dysfunction persist despite conservative therapy7). Despite spontaneous regression over time, the effects of conservative treatment including medications and long-term prognosis have been insufficiently investigated. Although we followed a conservative treatment plan with the patient, considering surgical management only as an alternative option, symptoms improved within a relatively short period of time (3 months after onset of symptoms on the right side and 2 months after onset on the left side). All MRI findings of bone marrow edema were improved.
Niimi et al.8) reported a case with low BMD in the femoral neck at the time of diagnosis and spontaneous recovery. In our case report, we were unable to measure changes in BMD at the time of symptom onset and recovery because DEXA was performed on the spine only at the initial onset of symptoms. Low T-score on the lumbar spine (–2.3 at L4 at the first and the second admission) implies that previous poor bone quality may be associated with the occurrence of BMES, however, the relatively high T-score on the hip area is diminishing the relation between bone quality and the occurrence of BMES.
Previous studies reported cases of unilateral or simultaneous bilateral BMES. In this case report, under nearly same social and physical conditions, BMES was diagnosed at different times on each side of the hip and a similar case has not been previously reported in the domestic literature. Additional studies are warranted to further investigate endogenous pathogenetic factors related to BMES. Furthermore, although BMES is a rare condition, differential diagnosis with other diseases associated with bone marrow edema is crucial, and the possibility of BMES on the opposite side of the hip at different onset times should not be ruled out.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download