INTRODUCTION
With increase of life expectancy, the prevalence of femoral neck fracture has increased by great amount. However, the elderly patients with femoral neck fracture often accompanies severe medical comorbidities and combined with the complications related to anesthesia, operation procedure and postoperative immobilization, the morbidity and the mortality rate has been reported to be high1). For the treatment, hip joint arthroplasty is considered to be the treatment of choice specially in the old age group as this could provide early ambulation which could potentially minimize postoperative complications such as deep vein thrombosis (DVT), pneumonia or congestive heart failure2).
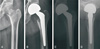
The femoral stem fixation using cement has advantage of providing immediate rigid stability which enables prompt weight bearing but has been reported to be associate with high rate of aseptic loosening and osteolysis in the long term follow up. For this reason, cementless stem fixation has been widely used and has been reported to develop durable interface with less associated complications3). In the old patient group however, severe osteoporosis is common and with the disturbance in the bony ingrowth, the intramedullary canal tend to become widen which in turn makes the cortex layer thinner (Fig. 1). With the consideration of change in femoral geometry, Dorr et al.4) has classified the morphology of the proximal femur into three types: A (Champagne), B (normal), C (stovepipe) (Fig. 1). In the patients with age above 60 years, C type proximal femur is common and combined with the poor bone quality and biological healing process, immediate stem stabilization is reported to be difficult with noncemented stem fixation4). In the current study, we followed the patients with age 75 years and more who had bipolar hemiarthroplasty with noncemented conical femoral stem due to femoral neck fracture. We report the clinical and the radiological outcome of these patients according to the proximal femur geometry.
MATERIALS AND METHODS
1. Study Subjects
Between September 2006 to December 2011, 86 patients (86 hips) with age 75 years and more and had Dorr type B or C proximal femur geometry were treated with noncemented conical femoral stem as a part of bipolar hemiarthroplasty procedure. Nine died and 2 were lost during the follow up and the remaining 75 patients (75 hips) who had minimum of 3 year follow up constitute the basis of our study. The retrospective review was performed using radiographic exams and the patient records. The mean age was 78 years (range, 75 to 95 years) at the time of the surgery and the majority of the patients were female (female, 61 [81.3%]; male, 14 [18.8%]) . Mean follow up was 46 months (range, 36 to 90 months) and all patients had underlying osteoporosis (mean, -3.62; range, -2.50 to -6.16) defined by T score less than -2.5 in dual energy X-ray absorptionmetry. The most common reason for fracture was slip down (64 hips, 85.3%) followed by fall down from height (8 cases, 10.7%) and car accident (3 cases, 4.0%). Using Dorr's classification of proximal femur geometry, the morphology of the femur was identified as type B in 34 hips and type C in 41 hips4).
2. Operation Methods
All operations were performed by a single surgeon with patient in a general or a spinal anesthesia. The time to operation was 4.3 days (range, 1 to 14 days) from the time of the injury. Operations were performed in lateral decubitus position using either posterolateral approach (32 hips) or anterolateral approach (43 hips). In all cases cementless conical femur stem was inserted by impaction and without use of cement. The stem used in this study, Wagner Cone Stem (Zimmer, Warsaw, IN, USA), is composed of titanium alloy and has corundum blasted finish along the surface of entire length. The stem has 8 longitudinal ribs with relatively sharp ridges which is intended to engage the femoral cortex (Fig. 2)5). Average length of the stem was 130 mm and 28 mm femoral head prosthesis was used in all cases.
To minimize the risk of leg length discrepancy, Kirschner wire was inserted at the iliac crest during the operation and the distance between this landmark to the tip of the greater trochanter was measured before the femoral head resection and after the stem was inserted. The size of the stem was corrected accordingly and the resultant leg length discrepancy was less than 5 mm in all cases.
For the postoperative rehabilitation, quadriceps strengthening exercise was started from the day of the operation and partial weight bearing ambulation with walker was initiated at 1 week. The level of weight bearing was slowly increased and reached full weight bearing by 12 weeks.
3. Clinical Assessment
The patient's clinical outcomes were evaluated using Harris hip score and were collected prospectively at 6 week, 3 months, 6 months, 12 months, and yearly thereafter. The score above 90 was defined as excellent, between 80 to 90 as good, between 70 to 90 as fair and under 70 as poor. Walking ability was also measured at each follow up time points using the categories of walking ability as described by Koval et al6). Additionally, any notable clinical symptoms including thigh pain, edema or sign of infection was carefully monitored throughout the entire follow up.
4. Radiographic Evaluation
For the radiographic evaluation, anteroposterior and the cross table lateral view of hip joint was used which included entire stem length. At each follow up, the radiographic images were compared with the index image immediately after the operation and the radiographic features of the aseptic loosening was carefully assessed at each Gruen zones7). Postoperative stem stabilization were evaluated according to the classification suggested by Engh et al.8) which used anteroposterior radiographs to assess the press fit of the stem, defined by contacting both endosteal cortices at the isthmus, and those without. The alignment of the stem was identified using the method described by Rothman et al.30) which defined neutral as less than 5 degree difference between the center line of the prosthesis and the femur. Also the subsidence of the stem was measured according to the definition by Callaghan et al.10) and if the displacement between the greater trochanter tip and the superolateral shoulder of the stem increased by more than 5 mm in sequential radiographs, it was considered as a significant subsidence1011) (Fig. 3). Osteolysis and loosening was defined when bone absorption occurs as an localized cyst or scallop shape and when the obvious change in the position of the prosthesis occur such as when progression of varus or valgus misalignment was observed12). Additionally, the acetabular wear was evaluated by measuring distance between upper most margin of the hemiarthroplasty cup to the acetabular bone in the sequential anteroposterior simple radiographs. Any evidence of stress shield, heterotopic ossification was also carefully monitored.
5. Statistical Analysis
Chi-square analysis was performed to compare the stem size, Harris hip score and the Koval ambulation category between Dorr type B group and type C group. Commercially available statistic software (SPSS for Windows release ver. 12.0; SPSS Inc., Chicago, IL, USA) was used with significance set at P<0.05.
RESULTS
1. Clinical Results
At the latest follow up, the overall Harris hip score was 86.2 (range, 70 to 92) with excellent result in 2 hips (2.7%), Good in 61 hips (81.3%), fair on 12 hips (16.0%) and no hips with poor result. The walking ability recovery to preoperative level was observed in 49 hips (65.3%) while 24 hips (32.0%) showed decreased ability by 1 category and 2 hips (2.7%) showed decrease by 2 category according to the categories of walking ability descried by Koval et al6). There was no statistical correlation between type B group and type C group when Harris hip score and walking ability were compared (Table 1).
Of the 70 patients who could ambulated without assist before the operation, the mean time to initiate walking with assist of walker or crutches were 9.6 days (range, 3 to 14 days).
2. Radiographic Results
In all cases, press fit was confirmed in anteroposterior X-ray immediately following the operation and the bony stability was achieved in all cases at the latest follow up (Fig. 4, 5). The evaluation of the stem reveled no hips with more than 5 degree varus or valgus malalignment. Three hips showed less than 5 degree varus change but did not show additional progression. Subsidence was observed in 4 hips but all were less than 5 mm and had no clinical symptoms. Also, no hips developed osteolysis, stem loosening or periprosthetic fracture. Acetabular erosion and the cup migration was observed in one case but was later identified to be result of delayed deep infection.
3. Complications
Despite the use of compressive stalking, intermittent air compression pump and the preventive anticoagulation agents, DVT was the most common complication occurring in 8 patients. The patients were treated conservatively with medication and were recovered uneventably. Heterotopic ossification was developed in 3 hips but were classified as Brooker type I ossification and did not cause motion limitation or pain13). Pulmonary embolism, posterior dislocation and delayed deep joint infection was observed in 1 hips respectively. The hip with posterior dislocation was treated by close reduction and immobilized with brace and no subsequent dislocation had occurred. Deep joint infection occurred 2 years after the index surgery and were treated with two stage eradication procedure using custom made PROSTALAC (prosthesis of antibiotics-loaded acrylic cement).
In 3 hips, intermittent thigh pain was observed after walking for more than 50 m but did not show any evidence of radiographic instability. The patients were treated conservatively with active quadriceps strengthening exercise and medication and the pain improved over time.
DISCUSSION
The goal of treating femoral neck fracture in elderly patients is to achieve early rigid stem fixation to allow early ambulation and rehabilitation and prevent complications from prolong immobilization. The treatment of choice for osteoporotic femoral neck fracture is considered to be hip arthroplasty as internal fixation has high likelihood of developing nonunion, avascular necrosis and fixation failure14).
When the hip joint arthroplasty was first introduced in 1970, John Charnley15) used poly(methyl methacrylate) (PMMA) to secure femoral stem and the cemented fixation has been considered as a standard method to fixate femoral stem. However, in the 1970s number of studies reported complication from cement fixation and the used of cement has became a debatable issue. The recent meta-analysis of mortality following cemented hip arthorplasty shows, little but significant increase of cumulative mortability rate upto first postoperative day16). As compared to noncemented prosthesis, use of cement resulted in 2.3 times greater risk of perioperative death and the risk was still 1.7 times higher one day after the operation. Also, number of studies reported potential risk of cement which includes pulmonary embolism, cement toxicity, hyptension which could cause fatal circulatory or respiratory problems1718). As such, the cementless prosthesis which promotes biological fixation are currently widely used. The stability of non-cemented type prosthesis depends on the initial press fitting stability and later biological fixation. The primary stability largely depends on the design and the surface finish of the prosthesis as well as the experience of the surgeon. When the noncemented type prosthesis was first introduced, common concern was that the early rigid fixation may not be achieved due to wide femoral canal and relatively thin cortical layer of the osteoportic femur19). However, the study by Hungerford and Jones3) claimed that the poor bone quality in the osteoportic bone should not be considered as a contraindication for using noncemented type prosthesis as durable interface can develop without PMMA. Also, the study from Carlsson and Nilsson20) reported that the bone mass do not have direct effect on the lossening of the femoral component in hip replacement. Regarding bony ingrowth to the prosthesis, Engh et al.8) reported that the decreased bone mass or the bony trabecular does not cause significant effect on the bone ingrowth and also the effect of patient's age, gender to the proximal femur remodeling is minimal. These findings suggest that even in the old patients accompanying osteoporosis, if appropriated prosthesis is used, early stabilization can be achieved through press fitting while later bony ingrowth can be achieved for long term stability. The conical stem used in the current study has been previously used with favorable result for the individuals suffering from the secondary osteoarthrtis of pyogenic coxarthritis, Legg-Calve-Perthes and developmental dysplasia of hip which result in deformation of proximal femur morphology521). Our institution decided to use this particular stem as most old age patients had underwent degenerative change in trabecular and the cortex layer resulting in stovepipe shape of proximal femur which is similar to the femoral shape from the diseases described earlier.
Dorr et al.4) had developed a classification for proximal femur bone quality by correlating radiographic appearance of bone and cortical index with bone mineral density which is widely used tool for matching femoral implant fixation in patient with total hip replacement. According to the study by Shon et al.22), the A type which resembles the champagne flute is common in the young age while the type C resembling stovepipe is more common in age over 60 years22). The common belief is that the strong, dense bone with thick cortices are better suit with cemetless fixation where as more osteoporotic bone with thin cortices are better fit for cement fixation.
Early mobilization following the operation is an important factor that could minimize post operative complications as this could decrease the risk of pneumonia, bed sore, urinary tract infection and joint contratracture which could ultimately lower mortality23). Hinchey and Day24) suggested that the ambulation should start within 2 to 3 weeks from the operation to minimize the complication and number of previous literatures suggests weight bearing ambulation by 12 weeks at the latest. The mean duration to walking was mean of 9.6 days in our study which is similar or shorter than the previous literature. The earlier ambulation was allowed in our institution as we believe the design of the prosthesis, which has multiple longitudinal ribs with sharp ridges, will tightly engage against the femoral cortex thereby provide secure initial stability. As no subsidence or loosening occurred after early ambulation, we believe our hypothesis is correct.
The thigh pain after femoral stem insertion are thought to be derived from the micromotion of unstable stem, the stress shielding phenomenon or the mechanical alteration of weight distribution and has been reported to occur in 13% after the operation25). This problem has been noted to occur in patients who start walking 6 to 8 weeks after the operation without application of brace. Most of this symptom disappear with time but if the pain persist the stability of the stem needs to be checked26). The unique prosthesis design of the conical stem used in the current study has reported to provide optimal rotational stability without use of cement and we believe this has decrease the rate of thigh pain27). The thigh pain occurred in only 3 hips (4.0%) in our series but the symptoms were very mild and completely disappeared within a year.
Engh and Bobyn28) reported that the proximal femur bone absorption occurs due to stress shielding which is from tight stem fixation at the femur isthmus and decreased stress to the femoral neck or calcar femorale. The conical shape femoral stem is designed as a distally fitted stem and theoretically stress shielding is more likely to occur in this design but this was not observed in our study. The conical stem is composed of titanium and compare to the stems made of cobart alloy, the elastic property is similar to the native cortex. Also, structurally, this type of stem has relatively smaller core diameter as compare to the ones without the ribs, therefore it has lower rigidity but superior elasticity which is optimal for weight distribution. Additionally, the space between each rib are the space where cortical bone do not directly contact with the stem and the thus angiogenesis at this region can occur before the bone resorption which ultimately can promote angiogenesis of the medullary canal5). Due to these features, we believe no complication associated with stress shielding was observe in our series. Another advantage of this stem is its sand blasting surface finish along the entire length which was proven in the previous literature to promote abundant surface bony growth in the animal and in the cadaver study. This surface finish can also minimize formation of particles less than 1 µm which could cause third body wear29).
In our series, sufficient endosteal bone formation was observed except in the Gruen zone 4 and at the latest follow up and the bone stability was achieved in all hips without evidence of significant subsidence or angular malalignment. The subsidence occurs as a result of change of contact between the femoral stem and the cortical bone. As the viscoelastic properties of the cortical bone is different from the prosthesis, applied stress can result in bone deformation which can lead to reduction of surface contact pressure at the bone to component interface1030). The minimal subsidence observed in the current study is due to the likelihood that the conical stem may have acted as a wedge which may have minimized prosthesis from sinking distally.
The fracture around the calcar femorale area is a common complication after impacting noncemented type femoral prosthesis and has been reported to occur in 1.5% to 27.8%. We experienced no fracture around the calcar area and we believed this is because the conical stem is design to press fit and have the tight contact with the femur at the distal portion. We had very carefully determined the size of the prosthesis before the prosthesis and during the operation, portable fluoroscopy was used to determine the size of the prosthesis so that the scratch fit could occurs at least 5 to 6 cm from the isthmus region. Also, in the stove-pipe type femur, the stem was inserted after 1 mm under reaming to maximize the stabilization.
The limitation of this study includes possible selection bias of the patients reviewed. The patients included in the current study are old patients with generally poor medical conditions. More than likely, there is possibility that the patients with poor walking ability and lack of personal assistance were unable to revisit the clinic while those with better outcome were more accessible for follow up. However, all patients in the current study had minimum of 3 year follow up and only 2 were lost during the follow up, we believe that the results we derived could be applied in general old age population. Other limitations include retrospective nature of the study, absence of the long-term follow up and the single institution review which should be considered in the future studies.
CONCLUSION
In our study, bipolar hemiarthroplasty using the cementless conical femoral stem showed excellent clinical and radiographic outcome for the osteoporotic femoral neck fracture regardless of the shape of the proximal femur. We believe this type of stem can be used effectively to treat patients with Dorr type B and C femur.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download