INTRODUCTION
Total hip arthroplasty (THA) is an effective and successful procedure; however, revision THA is required for some patients and the severity of proximal femoral deficiency affects the selection of femoral components during revision THA1).
The main goals of femoral revision surgery are to relieve pain, improve biomechanical function, and achieve stability of the revised femoral stem. Nevertheless, femoral bone defects are common during revision THA, and stable fixation of the prosthesis is often difficult to achieve. To resolve these problems, a variety of surgical procedures and femoral components have been developed and used. Recently, the use of modular femoral stems became common in complex primary THA or revision surgery because of easy adjustment of desired anteversion or leg length owing to modularity2) and stable fixation in the diaphyseal portion of the femur with relatively good bone quality achieved by bridging proximal femoral bone defects34).
The purpose of this study was to evaluate the clinical and radiological results of revision THA that used proximal modular, distally fixed cementless stems, and to examine the usefulness of these stems.
MATERIALS AND METHODS
Among 70 patients (73 hips) who received revision THA using cementless modular femoral stems because of proximal femoral bone defects from February 2006 to October 2012, 45 patients (47 hips) with a minimum follow-up of 2 years were analyzed retrospectively. We excluded 25 patients with pathologic fractures and those who could not be followed up for more than 2 years. The study included 29 males and 18 females. The causes of primary THA were osteonecrosis in 21 hips, femoral neck fracture in 16 hips, and osteoarthritis in 10 hips. The mean age at the time of revision surgery was 62.6 years (range, 41-85 years). The mean follow-up period was 53.4 months (range, 25-100 months).
Revitan® stems (Zimmer, Warsaw, IN, USA) used in this study are made of titanium alloy, consist of proximal and distal components, and use a Morse taper to achieve mechanical stability. The proximal component is designed with a 44 mm offset to improve gluteal muscle function and avoid excessive stress on connections. The distal component, which has 8 sharp vertical anchoring ribs in a conical design, was fixed into the femoral diaphyseal cortex to achieve mechanical stability (Fig. 1).
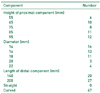
The causes of revision THA were aseptic loosening in 30 cases (63.8%), periprosthetic femoral fractures in 14 cases (29.8%), and other causes in 3 cases (6.4%). All operations were performed by a single surgeon with the use of the anterolateral approach. During revision surgery, only the stem was revised in 7 cases (14.9%), the stem and liner were revised in 2 cases (4.3%), and the stem and acetabular cup were revised in 38 cases (80.8%). The length of the femoral stem was chosen to be sufficient for stable fixation of the distal component. Extended trochanteric osteotomy was conducted in 15 cases (31.9%) because of the difficulty in removing the existing implants or bone cement. In addition, strut allografts were used in 4 cases (8.5%). The length of the distal part of the stem was 140 mm in 20 cases and 200 mm in 27 cases. The length of the proximal part was 55 mm in 6 cases, 65 mm in 10, 75 mm in 8, 85 mm in 11, and 95 mm in 12. The stem diameter was 14 mm in 16 cases, 16 mm in 13, 18 mm in 11, 20 mm in 3, and 22 mm in 4. Curved stems were used in all cases (Table 1). In revision THA, proximal femoral bone defects were found in all cases. According to the Paprosky classification5), 31 cases (66.0%) were type II, 7 (14.9%) type IIIA, and 9 (19.1%) type IIIB. Partial weight-bearing ambulation with crutches was permitted on the 3rd postoperative day and full weight-bearing was permitted from the 6th postoperative week.
Clinical results were analyzed by comparing the Harris hip score (HHS)6) and ambulatory status according to the Koval classification7) before revision THA and at the final follow-up. Radiological results were analyzed using a standard radiographic view of the pelvis and a lateral view of the hip. Stem stability, changes in the stem position, and the radiolucent line were examined using radiographs taken postoperatively on a regular basis. Femoral component fixation was graded as bony stable, fibrous stable, or unstable according to the criteria described by Engh et al8). Femoral stem stability was evaluated by measuring the distance from the proximal tip of the greater trochanter to the shoulder of the stem. When it was difficult to measure this distance directly, the distance between the proximal modular components of the femoral stem and wires fixed in the femur was measured instead. For the femoral component, subsidence of more than 5 mm, a radiolucent zone more than 2 mm wide around the whole stem, or a change in varus or valgus stem position was defined as loosening. Kaplan-Meier survival analysis was performed with the end point of re-revision THA conducted due to infection or dislocation9).
RESULTS
The mean HHS improved from 39.5 (30-70) points preoperatively to 91.3 (82-96) points at the final follow-up (P<0.01). Walking ability improved in all cases except one patient with a history of cerebral infarction.
In all cases, the modular femoral stem showed stable fixation on radiographs, and stem loosening was not observed during follow-up (Fig. 2, 3). In one case of fibrous stable fixation, the femoral stem showed a subsidence of 5 mm, but the subsidence did not progress further after the first postoperative year and stable fixation was confirmed at the final follow-up.
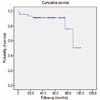
Postoperative complications included 5 cases of infection and 2 cases of dislocation; re-revision surgery was performed in all these cases. In all 5 cases of infection, the infection was deep and the patients were treated using a prosthesis of antibiotic-loaded acrylic cement (PROSTALAC). Of these, one patient underwent re-revision THA with the cup-in-cage technique10) after the infection was apparently cleared. In the 2 cases with dislocation, there was no association between dislocation and stem subsidence and re-revision THA was performed using constrained liners. The 8-year survival rate was 86% (95% confidence interval, 75.7-95.7%) as the end point of re-revision surgery due to infection and dislocation (Fig. 4).
DISCUSSION
The goals of revision THA are to achieve implant stability by reconstructing bone defects, to restore hip biomechanics, and to correct leg length inequality. To achieve these goals, a wide range of arthroplasty procedures have been conducted that used cemented femoral stems1112), collarless conical femoral stems131415), fixation to the distal shaft using extensively porouscoated cementless stems11617), and proximal or distal fixation using cementless modular stems1819202122). The success rate of revision surgery using cemented femoral stems ranges between 50% and 90%. According to Hunter et al.23), surgical outcomes were good in 24% of cases and fair in 51% during a minimum follow-up of 6 months, and re-revision was performed in 22% of the patients. Early implant loosening may occur after surgery using cemented femoral stems, since a firm bond cannot be achieved in the medullary cavity using cement. On the contrary, revision using cementless femoral stems can preserve bone mass to the maximum extent without cement-related complications, and minimizes the risk of liner wear caused by cement wear debris2425).
For proximal femoral defects of Paprosky type II and higher, modular femoral stems have been used to improve stem stability and facilitate restoration of equal leg lengths. A modular distal fixation stem consists of a proximal sleeve and a shaft component; it can easily and precisely provide stable fixation of the distal stem in the diaphyseal portion of the femur, which has relatively good bone quality, by bridging bone defects, and can be conveniently assembled at the desired anteversion angle or leg length intra-operatively52026). Cameron18) conducted a 3.5-year follow-up of patients who underwent THA with modular femoral stems and reported a success rate of 94%. Chandler et al.27) achieved favorable outcomes in more than 84% of 52 patients who underwent revision THA and were followed up for 3 years on average; only 4% of the patients complained of thigh pain. Kwong et al.21) reported a success rate of 97.2% in hips after revision surgery that used the LINK MP modular distal fixation stems (Waldemar LINK, Hamburg, Germany); the mean follow-up in this study was 3.3 years. In a study by Amanatullah et al.28), who used stems of the same type, the mid-term follow-up results indicated a high success rate of osseointegration. In revision surgery with modular MRP-Titan revision stems (Peter Brehm GmbH, Weisendorf, Germany), Wirtz et al.22) and Schuh et al.29) reported success rates of 95.8% and 96.2%, respectively. In the present study, which used Revitan® stems for revision THA, femoral stem stability was achieved in all patients, and the mean subsidence was 0.6 mm at the final follow-up.
Hoberg et al.30) performed revision using the MRP-Titan stems and reported a revision rate of 6.8% and a 9.75-year survival rate of 85.6% according to Kaplan-Meier survival analysis. In a study by Wirtz et al.31), the revision rate was 6% and the 15-year survival rate was 85%. Brown et al.32) reported a 12-year survival rate of 95%. In this study, according to Kaplan-Meier survival analysis, the 8-year survival rate was 86%.
Possible disadvantages of modular distal fixation stems are wear in the modular part, metal wear debrisinduced loosening, stress shielding in the proximal femur, the loss of bond strength in the modular portion, and metal failure193334). However, we did not detect any mechanical defects or stress shielding in the present study.
This study has some limitations. Since we used a retrospective study design without controls, the successful restoration using the modular femoral stem system is difficult to compare to other systems. Moreover, the mid-term follow-up results are insufficient to fully examine the long-term survival rates or outcomes. Despite these limitations, this study was meaningful because all surgical procedures were carried out by the same surgeon using identical femoral stems.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download