Abstract
Subchondral bony cyst, large solitary or multiple cysts in acetabular dome usually exacerbate progression to degenerative osteoarthritis in the hip joint. But it can be treated through arthroscopic intervention. We report two cases that treated by arthroscopic curettage and bone graft for subchondral bony cysts in early osteoarthritis of the hip joint, and it may delay progression to moderate osteoarthritis.
Osteoarthritic subchondral cysts frequently occur in weight-bearing joints such as the hip. The etiology of these cysts in hip osteoarthritis remains uncertain. Traditionally, bone cysts on the hip joint have been treated conservatively. However, this approach is unsatisfactory for cysts that are large or occur in multiples or on the weight-bearing region of the joint, as they compromise the integrity of the articular surface1-3). Recently, improved operative technique and development of instruments, have enabled the application of arthroscopic approaches to numerous intra-articular and extraarticular hip conditions, such as acetabular labral tear, femoroacetabular impingement (FAI), cartilage injury, ligamentum teres injury, adhesive capsulitis, and septic arthritis. In this study, we report the short-term results of arthroscopic treatment of large or multiple bone cysts in patients with evidence of early osteoarthritis and FAI on radiology and without improvement of symptoms by conservative treatment. (But, main symptoms may be due to FAI.)
A 48-year-old male visited Department of Orthopedic Surgery, Chungnam National University Hospital complaining of right anterior thigh pain beginning six months prior without any history of trauma. He had begun having pain in the right inguinal area and difficulty in crossing his legs on the floor beginning six months earlier, and the pain had intensified over that period. He had no other medical issues and had been exercising regularly for over 10 years. On the first visit, physical examination indicated impingement and a simple X-ray revealed sclerotic changes on the right acetabular rim (center-edge [CE] angle of Wiberg, 30°; sourcil angle of Tönnis, 2.1°; Tönnis classification Grade I). Computed tomography and magnetic resonance images showed a partial tear of the ligamentum teres, a central acetabular osteophyte, a spur on the articular surface of the inferior margin of the femoral head/neck junction, and a 1.6×1.5×1.8 cm subchondral cystic lesion on the anterosuperior acetabulum (Fig. 1). Surgical treatments were performed after the six-month drug therapy which did not improve symptoms. Arthroscopic investigation revealed a partial tear of the ligamentum teres, labral tear and a subchondral fibrocartilagenous cystic lesion on the acetabulum.
Thus, ligamentum teres was managed by shrinkage and the labrum was re-fixed in the central compartment, and femoroplasty and acetabuloplasty (osteoplasty) were performed in the peripheral compartment. A C-arm image intensifier was then used to locate the cyst and using an awl, a hole was made on the cyst cover and the yellowish fluid inside the cyst was drained. Microfracture was carried out on the inner-surface of the cyst. Under arthroscopic guidance, the silicon drain tube was used to implant the allogeneic bone graft, which was extruded using a rod and into the cyst (Fig. 2). The patient was discharged 3 days after surgery and allowed to walk on crutches (so that only half the body weight was supported by the repaired hip) for the first 6 weeks after surgery, with gradual progression to full weight bearing thereafter. At 18 months post-surgery, the patient experiences only mild intermittent hip pain and modified Harris Hip Score (mHHS) was improved from 37 to 87, and visual analogue scale (VAS) score has decreased from 7 (before surgery) to 1. By radiology at last follow-up, the grafted bone was well maintained at its initial location and the graft was consolidating with the surrounding bone.
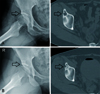
A 49-year-old female visited Department of Orthopedic Surgery, Chungnam National University Hospital complaining of right inguinal pain without any trauma history. She was a teacher and did not regularly engage in athletic activity. Her pain increased despite three months of treatment. On the initial visit, physical examination confirmed severe tenderness on the greater trochanter and positive sign of anterior impingement test. Radiology revealed mild hip dysplasia and multiple cystic lesions on the right anterior rim of acetabulum to the anterioinferior iliac spine (CE angle of Wiberg, 22°; sourcil angle of Tönnis, 8.8°; Tönnis classification Grade I). Surgical treatments were performed after the three-month drug therapy which did not improve the symptoms. Arthroscopy revealed a labral tear, a subchondral cyst of the acetabulum, and bone protrusion. Thus, femoroplasty and labral refixation were performed, followed by curettage and allogeneic bone graft as described for Case 1 (Fig. 3). 16 months post-surgery, some pain remains, but the patient's condition is improved relative to that before surgery. The mHHS improved from 56 to 75, VAS score has decreased from 7 (before surgery) to 3. And by radiography, the grafted bone was well maintained at its initial location.
The clinical results of arthroscopic surgery to treat acetabular cysts accompanied by FAI were reported by Imam et al. at the International Society for Hip Arthroscopy Conference in 2013. According to their report, while most solitary rim cysts do not progress, large solitary or multiple cysts in acetabular dome usually exacerbate progression. Moreover, other studies have reported that growing bone cysts around the hip joint are caused by fluid influx through an injured acetabular labrum or adjacent cartilage injury, and progression to osteoarthritis12345).
A few cases of bone cysts on the acetabulum or femoral neck region have been reported in patients with FAI6). As discussed above, the authors assumed that no treatment is considered necessary for small cysts with no change in size, but treatment is required for cysts that grow or that threaten to compromise of articular surface, so the arthroscopic treatments were expected to slow down the progression to arthritis in the early osteoarthritis with large and multiple cysts.
Large or multiple cysts develop on the weight-bearing portion of the joint and occasionally induce invasive change on the articular surface. Theories on their pathogenesis include that they originate from intrusion of synovial fluid into the bone at the joint surface, initiate in areas of bone necrosis, or are confined to pressure segments in the femoral head and acetabulum135789). Additionally, these lesions seldom heal spontaneously.
Bone cysts on the hip joint are usually located deep beneath the thick soft tissue, and are thus difficult to approach percutaneously for treatment. Open approaches such as Smith-Peterson or Kocher-Langenbeck are invasive and can cause complications including postoperative hematoma, infection, scar formation, and myositis ossificans. However, since arthroscopic surgery allows access to soft tissues and bony structures around the hip joint with only small skin incisions, it is less invasive and allows more rapid rehabilitation. Further, because cysts along the acetabulum are associated with labral pathology10), arthroscopic surgery allows concomitant diagnosis and treatment of both problems.
Here, we report preliminary clinical results of two cases employing arthroscopic debridement and allogeneic bone grafts to treat bone cysts of the hip. The hip arthroscopy of patients with subchondral bone cyst showed arthritic change, and treating which by debridement and bone graft needs long term follow up. Nevertheless, this study has the particular significance for the possibility that the bone graft for the bone cyst in the hip joint can be successfully performed through arthroscopy. In further long-term comparative studies with a larger sample size, the usefulness of the arthroscopic diagnoses and treatments, and the effects of the bone graft on the bone cysts in early osteoarthritis patients, may be confirmed.
Figures and Tables
Fig. 1
(A) Preoperative simple X-ray and computed tomography (CT) image of Case 1. A large cyst (arrow) is located on the acetabular dome. (B) Postoperative immediately CT image and plain radiographs at last follow-up. The bone graft appears well maintained (arrow).
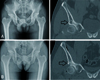
Fig. 2
Cyst location and arthroscopic procedure. (A) A C-arm image intensifier allows the cyst to be located. (B) Osteoarthritis finding in arthroscopy. (C) Opening of the cyst and the yellowish serous fluid drained and curettage of the outer and inner surface of the cyst. (D) Allogeneic bone graft inside the cyst using a silicon tube.
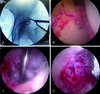
Fig. 3
(A) Preoperative simple X-ray and computed tomography (CT) image for Case 2. Multiple cysts (arrow) are revealed on the acetabular dome. (B) Postoperative immediately CT image and plain radiograph at last follow-up. The allogeneic bone graft is well maintained at its initial location (arrows).
References
1. Sabokbar A, Crawford R, Murray DW, Athanasou NA. Macrophage-osteoclast differentiation and bone resorption in osteoarthrotic subchondral acetabular cysts. Acta Orthop Scand. 2000; 71:255–261.

3. Dürr HD, Martin H, Pellengahr C, Schlemmer M, Maier M, Jansson V. The cause of subchondral bone cysts in osteoarthrosis: a finite element analysis. Acta Orthop Scand. 2004; 75:554–558.

4. Leunig M, Beck M, Kalhor M, Kim YJ, Werlen S, Ganz R. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement. Radiology. 2005; 236:237–246.

5. Schmalzried TP, Akizuki KH, Fedenko AN, Mirra J. The role of access of joint fluid to bone in periarticular osteolysis. A report of four cases. J Bone Joint Surg Am. 1997; 79:447–452.
6. Jamali AA, Fritz AT, Reddy D, Meehan JP. Minimally invasive bone grafting of cysts of the femoral head and acetabulum in femoroacetabular impingement: arthroscopic technique and case presentation. Arthroscopy. 2010; 26:279–285.

7. Ferguson AB Jr. The pathology of degenerative arthritis of the hip and the use of osteotomy in its treatment. Clin Orthop Relat Res. 1971; 77:84–97.
8. Milgram JW. Morphologic alterations of the subchondral bone in advanced degenerative arthritis. Clin Orthop Relat Res. 1983; 173:293–312.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download