Abstract
Purpose
This study assessed the short term clinicoradiological results of primary total hip arthroplasty using third generation ceramic-ceramic articulation Accolade TMZF femoral stems.
Materials and Methods
Two hundred and seventy two patients (294 hips) with primary total hip arthroplasty using third generation ceramic-ceramic articulation Accolade TMZF femoral stems who had been followed-up for a minimum of 3 years were included. Clinicoradiological results were analyzed and postoperative complications were observed.
Results
At final follow-up, mean Harris hip score was increased from 52 to 94 points. On radiogical evaluation, the average acetabular inclination was 42 degrees and the average acetabular anteversion was 15 degrees. Neither osteolysis nor loosening were observed around the acetabulum or proximal femur. Among 294 acetabular cups, 293 cups (99.66%) achieved stable fixation. Regarding the 294 femoral stems, 286 (97.28%) had bony fixation, 7 (2.38%) had fibrous fixation, and none were found to have unstable stem fixation. Proximal bone resorption was observed in 17 hips (5.78%; only Grade 1) and radiolucent lines were observed in 88 hips (29.93%), however, all were around the distal smooth portion of the stems. Postoperative complications included dislocation in 6 hips (2.04%), heterotopic ossification in 3 hips (1.02%), ceramic fractures in 4 hips (1.36%), superficial infection in 1 hip (0.34%), and squeaking in 8 hips (2.72%).
Conclusion
The short term clinicoradiological results of primary total hip arthroplasty using third generation ceramic-ceramic articulation and Accolade TMZF femoral stems together with Secur-Fit acetabular cups were satisfactory. However, problems such as ceramic fractures and squeaking after arthroplasty were observed. Additional studies are necessary in order to develop methods that may reduce or eliminate these complications.
Total hip arthroplasty is a widely used method for reconstructing hip joints that have suffered diseases- or trauma-related injuries. However, studies on developing alternative materials for articulation have been conducted to prevent osteolysis (caused by wear debris that occurs between two bearing surfaces), aseptic loosening, and other problems that have a negative impact on the longevity of bearing articulation in conventional arthroplasty. To address these problems, cross-linked polyethylene, metal-on-metal articulation, and ceramic-on-ceramic articulation have been used. The primary advantage of using ceramic-on-ceramic articulation is low friction articulations with excellent wear resistance. Moreover, ceramic-on-ceramic articulation is known to have almost no risk of adverse reactions caused by wear particles due to a minimum coefficient of friction, and is therefore currently considered as the most ideal articulation with excellent biocompatibility. Although advances in ceramic techniques, manufacturing processes, and the use of third-generation ceramic-on-ceramic articulation have been associated with successful results attributable to enhanced durability and wear properties, the use of ceramic materials with brittleness remains controversial due to fracture potential, component damages, and "squeaking"1). The aim of the current study was to analyze and report clinicoradiological results and complications following the performance of primary cementless total hip arthroplasty using Accolade TMZF femoral stems (Howmedica Osteonics-Stryker, Cork, Ireland) and Secur-Fit peripheral self-locking (PSL) acetabular cups (Howmedica-Osteonics-Stryker) from November 2002 to July 2010 with a minimum follow-up of 3 years.
This study included 294 hips from 272 patients that could be followed-up for at least 3 years among 367 hips from 337 patients that underwent cementless total hip arthroplasty using ceramic articulation, Accolade TMZF femoral stems, and Secur-Fit cups due to hip-joint disease or trauma from November 2002 to July 2010. Subjects were 181 men and 91 women, and the male-to-female ratio was 2:1. Mean follow-up was 5.2 years (range, 3-11 years), and the mean patient age was 55 years (range, 21-86 years). In preoperative diagnosis, 184 cases were assessed as avascular necrosis, 58 as primary and secondary osteoarthritis, 44 as fracture, 3 as Legg-Calvé-Perthes disease sequalae, 2 as congenital acetabular dysplasia, and 3 as infection sequalae (Table 1).
Subjects were given antibiotics for 5 preoperative days. The posterior approach was used in all total hip arthroplasty patients by placing them in the lateral position. Accolade TMZF femoral stems and Secur-Fit PSL ceramic cups (Stryker Orthopaedics) were used in all surgical procedures. Postoperative adduction and medial rotation of the hip was restricted due to the risk of dislocation by thoroughly instructing all patients. On the first postoperative day, ambulation training was initiated using ambulation assist devices such as a walker after standing exercise on a tilt table, in addition to quadriceps femoris muscle strengthening. The drainage tube was removed once drainage was less than 100 mL (after 2-3 postoperative days on average). All patients began standing and ambulation training on the 1st postoperative day regardless of the presence of the drainage tube. Partial weight-bearing was performed using a walker or crutches until the 7th postoperative day, after which full weight-bearing was allowed in patients without preoperative gait disturbance from the 1st postoperative week.
Clinical results were evaluated on the 3rd and 6th months postoperatively, at the 1st year pre- and postoperatively, and every following postoperative year until the 11th postoperative year by measuring thigh pain and Harris hip scores. Hips with a score >90 points, >80 points, ≥70 points, and <70 points were defined as having excellent, good, fair, and poor results, respectively. Outpatients were asked to choose from a visual analogue scale (VAS) of 1-10 to determine their degree of thigh pain. The current study used VAS scores obtained at the final follow-up. The Dorr classification2) was used to assess the preoperative quality of the femoral bone. Based on radiographs, the stability and osteolysis around the acetabular cups and femoral stems were assessed. Conditions of femoral stem fixation were classified into bony ingrowth, stable fibrous ingrowth, and unstable fixation according to radiolucent lines and stem movement using the classification system described by Engh et al3). The presence and degree of changes in bones around the femoral stems were evaluated based on spot welds on both the medial and distal cortical hypertrophy, the stress shielding of the proximal femur, osteolysis, and radiolucency around the stem. Changes in bone positions of the femoral stems were determined according to the classification system described by Guren et al4). Loosening of the femoral stem was defined as vertical subsidence of more than 2 mm or valgus and varus deformities in the stem. Movement of the acetabular cup was compared using radiographs taken in the immediate postoperative period and at the final follow-up based on the anterior and posterior views of the hip. According to the method of Dorr et al.2), the distances between the acetabular component and Kohler's line and the teardrop were measured. Acetabular cup inclination angles were measured using the method of Callaghan et al.5), and acetabular anteversion was measured using the method of Boardman et al6). Osteolysis around the acetabular cup was presented as DeLee and Charnley7) zones. The acetabular cup was defined as loosening if there was movement in the position of the cup of more than 2 mm vertically, medially, or laterally, if the radiolucent lines were widened more than 2 mm in the anterior, posterior, or lateral radiographs of the acetabular cup, or if the inclination angle changed by more than 5 degrees. We identified the presence of complications including infection, dislocation, fractures in the ceramic head and liner, heterotopic ossification, and squeaking.
The average Harris hip score improved from 52 points (minimum 22, maximum 68) preoperatively to 94 points (minimum 72, maximum 99) postoperatively. There were 245 excellent cases (83.33%), 43 good cases (14.63%), 6 fair cases (2.04%), and no poor cases (0%). Three patients (1.02%) complained of thigh pain with scores of 3, 5, and 3 points, respectively, on the 10-point VAS.
The average acetabular inclination was 42 degrees (range, 34-60) and the average acetabular anteversion was 15 degrees (range, 7-16). In the final follow-up, 294 hips (100%) showed stable fixation. Of these, 293 hips (99.66%) had no osteolysis or loosening around the acetabular cups with the exception of 1 case with penetration of the acetabular metal cup after a ceramic liner fracture. There was no horizontal or vertical movement of acetabular cups. Although radiolucent lines with a width <2 mm were observed in 24 hips (8.16%), all 24 acetabular cups were found to be stable.
According to the classification system of Engh et al.3) regarding femoral stem fixation, bony ingrowth was observed in 287 cases (97.62%) and stable fibrous ingrowth was observed in 7 cases (2.38%). No cases of postoperative unstable fixation were observed at the final follow-up. Stress shielding bone resorption in the proximal femur was found in 17 hips (5.78%, all Grade 1) according to Engh's criteria8). Radiolucent lines detected in 88 hips (29.93%) around the femoral stems were all <2 mm thick. Additionally, all were found around the distal part of the stem without porous coating in Gruen zones 3, 4, and 5. There were 3 cases (1.02%) that showed varus and valgus <1 mm in the distal femoral stem. Widened interfaces >2 mm, defined as loosening, were not seen. There were no cases with fracture or vertical subsidence of more than 2 mm in the femoral stems.
Six hips (2.04%) with postoperative dislocation were managed using closed reduction and hip abduction orthosis. Patients wore a brace for an average of 3 months. According to the classification system described by Brooker et al.9), heterotopic ossification was detected in 3 (1.02%) hips (2 hips Grade 1, 1 hip Grade 2). However, there were no reports of pain or observations suggestive of significant restrictions in the range of movement of the hip. Ceramic liner fracture was observed in 4 hips (1.36%), and acetabular cup revision was performed in 1 case (0.34%) with penetration of the acetabular metal cup after ceramic liner breakage. Favorable clinical results were demonstrated after revision. Squeaking was detected at a relatively high frequency (8 cases, 2.72%). Superficial infection occurred in 1 case (0.34%), and the patient was treated with wound cleansing, removal of dead cells, and use of antibiotics (Table 2).
Total hip arthroplasty has demonstrated good results in concert with the continuous development of articulation materials, improvements in structural design, and advancements in surgical techniques10). The leading causes of total hip arthroplasty failure are osteolysis and loosening of the artificial hip joints caused by fine wear particles from the artificial articulations. Ceramic-on-ceramic articulation has favorable biological response and an extremely low coefficient of friction that minimizes the occurrence of wear debris particles and osteolysis11). The current study used Accolade TMZF femoral stems12,13) and Secur-Fit acetabular cups made of a beta titanium alloy with a 25% higher flexibility and a 20% higher tensile strength than those of the Ti-6Al-4V titanium alloy. Several previous studies have already reported satisfactory Harris hip scores in total hip arthroplasty with cementless tapered-wedge femoral stems14). Parvizi et al.15) reported satisfactory results at a mean Harris hip score of 92.1 in 129 hips with taperloc femoral stems including a case of revision surgery through a long-term follow-up. The current study also obtained a comparable outcome from a mean preoperative Harris hip score of 52 points (minimum 22, maximum 68) which increased to a mean follow-up Harris hip score of 94 points (minimum 72, maximum 99). The frequency of thigh pain was found to be low in tapered-wedge femoral stems16,17), and may have been attributable to successful osteointegration and primary stability, as weight bearing of the femur is evenly distributed from the proximal part to the distal part with a gradual decrease of stiffness in femoral stems around the distal portion of stems18). A low incidence of thigh pain was observed (3 cases, 1.02%) after insertion of tapered-wedge femoral stems in the current study (Fig. 1).
Stress-shielding of the proximal femur results in bone resorption when stress is reduced in femoral stems around the femur postoperatively, as the stress from weight-bearing is restricted from the proximal part. This occurs in cases of incomplete osteointegration of the femoral stem in the proximal femur, fixation at the distal part, or use of metal femoral stems with a high degree of stiffness19). In the current study, a relatively lower frequency of stress-shielding was observed in 17 hips (5.78%). Reduced stress shielding is thought to be the result of compression fixation using tapered-wedge femoral stems with the lower hardness of beta titanium and facilitated osteointegration with the proximal femoral stem. A relatively high osteolysis rate leading to failure of total hip arthroplasty has been verified in conventionally designed femoral stems. Studies conducted by Kim and Kim20), and Woolson and Maloney16) reported osteolysis in 38 femoral stems (32.76%) among 116 porous coated anatomic femoral stems, and in 15 femoral stems (21.73%) among 69 Harris-Galante-porous femoral stems. Therefore, the need for new designs and materials for femoral stems has been demonstrated, and a tapered-wedge design has been newly developed. In tapered-wedge femoral stems, osteolysis of the proximal part is caused by the sheath of the proximal femoral stem, as well as osteointegration due to peripherial bone tissues and bone growth. However, the incidence of osteolysis of the distal part is rare21). Despite the occurrence of osteolysis, it is thought to be limited to the proximal part22). Instability of femoral stems was not detected in the current study and favorable results of cementless tapered-wedge femoral stems were comparable to those of previous studies.
"Squeaking" has recently become one of the most controversial complications associated with total hip arthroplasty using ceramic-on-ceramic articulation. Until recently, squeaking was attributed to wear caused by material instability of ceramic articulations prior to the third generation, the elevated metal rim around the acetabular cup used to secure alumina ceramic liners of the cup, and neck impingement. The frequency of squeaking has been reported to range between 0.48-21% in ceramic-on-ceramic articulation23). Moreover, it has been reported to occur due to wear caused by fine glass particles from neck impingement of Trident acetabular cups (Stryker, Mahwah, NJ, USA)24,25). Due to the progression of fine wear, the possibility of squeaking remained for second generation components and has also been reported for third-generation ceramics17,24,25), as they can be affected by abnormal or unevenly applied force due to improper postoperative position of the acetabular cup and ceramic head, subluxation26), bearing mismatch27), microseparation damage of the ceramic head and fluid film of the articulation due to wear debris26), the patient's body mass index, or certain activities of the hip28). By using Accolade TMZF femoral stems, the current study allowed for variety in the length of the femoral neck according to the trapezoidal neck design and stem size to reduce femoral neck impingement with the metal rim around the acetabular cup. However, squeaking was detected in 8 cases (2.72%), which was relatively high and required long-term follow-up. As no pain was reported in all cases, these patients are still under follow-up will be further monitored.
Ceramic head and liner fractures are the second most commonly reported complication, followed by squeaking, in ceramic-on-ceramic articular surfaces. Recent advances in manufacturing techniques and processes have enabled the production of smoother ceramic surfaces, and the frequency of fractures has been reduced to 0.04% along with improvements in stiffness and designs29). However, the frequency of ceramic head and liner fractures has increased in concert with the increased demand for total hip arthroplasty using ceramic articulations. Repeated impingement between the neck of the femoral stem and the ceramic liner of the cup is thought to be one of the main causes of ceramic fractures. Therefore, a way to decrease impingement has been proposed and involves maintaining a low ratio between the head and neck diameters using the design of the femoral stem neck with a small circular diameter and a 28 mm ceramic head30). In addition, neck length has been identified as another cause of ceramic fracture. Specifically, a short-neck ceramic head has been reported to be vulnerable to fractures due to a thin ceramic head with larger mating surfaces between the trunion of the femoral stem and the ceramic head and their relatively deeper insertion as compared to the standard, long-neck ceramic head31). On the other hand, the incidence of ceramic head fracture has been reported to be higher in a ceramic head with a long-neck due to stress created below the stem resulting in expanded tension force from the inner side to the upper part due to a shallow mating surface with the internal ceramic head32). Impingement has been implicated as the main cause of ceramic fractures in Asians with a wide range of motion in the hip. Koo et al.33) suggested that ceramic head fractures could be caused by design problems, short necks, scratched femoral heads, and high physical activity levels. Min et al.34) also proposed that repeated impingement between the neck of the femoral stem and the ceramic liner could lead to liner breakage in Asians with an excessive range of movement in the hip due to sitting with crossed legs, squatting, and kneeling. Toni et al.35) postulated that liner breakage could also occur on the other side of the impingement due to micro-dislocation or subluxation. In the current study, there were 4 hips (1.36%) with ceramic liner breakage. Of these fractures that occurred in 3 patients, one was sustained during farming work, another during cycling, and one had no known cause. These cases are thought to be attributable to impingement caused by an excessive range of motion or wear debris. The other case of fracture was ascribed to injury from car accident trauma. One case (0.34%) with penetration of the acetabular metal cup after ceramic liner breakage demonstrated stable fixation after performance of acetabular cup revision and head and liner revision. Revisions were conducted in 3 hips (1.02%) with head and liner fractures (Table 3) (Fig. 2).
The results of the current study demonstrated more stable and improved clinicoradiological outcomes in cementless total hip arthroplasty using third generation ceramic-on-ceramic articulation Accolade TMZF femoral stems with a minimum follow-up of 3 years as compared to those of previous studies that used cross-linked polyethylene or metal-on-metal articulations. However, ceramic liner fracture and squeaking were detected at a relatively higher frequency of 1.36% (4 hips) and 2.72%, respectively, among the most controversial complications. Therefore, additional studies are necessary in order to further investigate these complications and reduce their frequency.
Figures and Tables
Fig. 1
(A) This anteroposterior radiography shows avascular necrosis of the femoral head in a 47-year-old male. (B) The immediate postoperative radiography shows good positioning of the prosthesis. (C) After 6 years, the radiograph shows no osteolysis around the right acetabular and femoral component, and stable components with proper bony ingrowth.
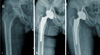
Fig. 2
(A) This immediate postoperative radiography shows total hip arthroplasty with the Accolade hip system in a 47-year-old male. (B) After 2 years, the radiography shows ceramic fracture and dissociation, as well as some alumina chips around the neck of the stem. (C) The ceramic head and liner were replaced.

References
1. Barrack RL, Burak C, Skinner HB. Concerns about ceramics in THA. Clin Orthop Relat Res. 2004; 429:73–79.

2. Dorr LD, Wan Z, Song M, Ranawat A. Bilateral total hip arthroplasty comparing hydroxyapatite coating to porous-coated fixation. J Arthroplasty. 1998; 13:729–736.

3. Engh CA, Hooten JP Jr, Zettl-Schaffer KF, et al. Porous-coated total hip replacement. Clin Orthop Relat Res. 1994; 298:89–96.

4. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; 141:17–27.
5. Callaghan JJ, Dysart SH, Savory CG. The uncemented porous-coated anatomic total hip prosthesis. Two-year results of a prospective consecutive series. J Bone Joint Surg Am. 1988; 70:337–346.

6. Boardman DL. A simple and reliable method of estimating radiographic acetabular anteversion. In : Proceedings of the 68th Annual Meeting of the American Academy of Orthopaedic Surgeons (February 28-March 4); San Francisco, CA: American Academy of Orthopaedic Surgeons;2001. p. 497.
7. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; 121:20–32.

8. Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990; 257:107–128.

9. Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973; 55:1629–1632.
10. Older J. Charnley low-friction arthroplasty: a worldwide retrospective review at 15 to 20 years. J Arthroplasty. 2002; 17:675–680.
11. Synder M, Drobniewski M, Kozłowski P, Grzegorzewski A. Ceramic-ceramic articulation in uncemented total hip arthroplasty. Wiad Lek. 2005; 58:193–197.
12. Casper DS, Kim GK, Restrepo C, Parvizi J, Rothman RH. Primary total hip arthroplasty with an uncemented femoral component five- to nine-year results. J Arthroplasty. 2011; 26:838–841.
13. Issa K, Pivec R, Wuestemann T, Tatevossian T, Nevelos J, Mont MA. Radiographic fit and fill analysis of a new second-generation proximally coated cementless stem compared to its predicate design. J Arthroplasty. 2014; 29:192–198.

14. McLaughlin JR, Lee KR. Total hip arthroplasty with an uncemented tapered femoral component. J Bone Joint Surg Am. 2008; 90:1290–1296.

15. Parvizi J, Keisu KS, Hozack WJ, Sharkey PF, Rothman RH. Primary total hip arthroplasty with an uncemented femoral component: a long-term study of the Taperloc stem. J Arthroplasty. 2004; 19:151–156.
16. Woolson ST, Maloney WJ. Cementless total hip arthroplasty using a porous-coated prosthesis for bone ingrowth fixation. 3 1/2-year follow-up. J Arthroplasty. 1992; 7:Suppl. 381–388.

17. Hamilton WG, McAuley JP, Dennis DA, Murphy JA, Blumenfeld TJ, Politi J. THA with Delta ceramic on ceramic: results of a multicenter investigational device exemption trial. Clin Orthop Relat Res. 2010; 468:358–366.

18. Head WC, Mallory TH, Emerson RH Jr. The proximal porous coating alternative for primary total hip arthroplasty. Orthopedics. 1999; 22:813–815.

19. Heekin RD, Callaghan JJ, Hopkinson WJ, Savory CG, Xenos JS. The porous-coated anatomic total hip prosthesis, inserted without cement. Results after five to seven years in a prospective study. J Bone Joint Surg Am. 1993; 75:77–91.

20. Kim YH, Kim VE. Results of the Harris-Galante cementless hip prosthesis. J Bone Joint Surg Br. 1992; 74:83–87.

21. Archibeck MJ, Berger RA, Jacobs JJ, et al. Second-generation cementless total hip arthroplasty. Eight to eleven-year results. J Bone Joint Surg Am. 2001; 83-A:1666–1673.
22. Sporer SM, Paprosky WG. Biologic fixation and bone ingrowth. Orthop Clin North Am. 2005; 36:105–111. vii

23. Keurentjes JC, Kuipers RM, Wever DJ, Schreurs BW. High incidence of squeaking in THAs with alumina ceramic-on-ceramic bearings. Clin Orthop Relat Res. 2008; 466:1438–1443.

24. Yang CC, Kim RH, Dennis DA. The squeaking hip: a cause for concern-disagrees. Orthopedics. 2007; 30:739–742.

25. Walter WL, Insley GM, Walter WK, Tuke MA. Edge loading in third generation alumina ceramic-on-ceramic bearings: stripe wear. J Arthroplasty. 2004; 19:402–413.
26. Ranawat AS, Ranawat CS. The squeaking hip: a cause for concern-agrees. Orthopedics. 2007; 30:738. 743.

27. Morlock M, Nassutt R, Janssen R, Willmann G, Honl M. Mismatched wear couple zirconium oxide and aluminum oxide in total hip arthroplasty. J Arthroplasty. 2001; 16:1071–1074.

28. Walter WL, O'toole GC, Walter WK, Ellis A, Zicat BA. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplasty. 2007; 22:496–503.
29. Heck DA, Partridge CM, Reuben JD, Lanzer WL, Lewis CG, Keating EM. Prosthetic component failures in hip arthroplasty surgery. J Arthroplasty. 1995; 10:575–580.

30. Yamaguchi M, Akisue T, Bauer TW, Hashimoto Y. The spatial location of impingement in total hip arthroplasty. J Arthroplasty. 2000; 15:305–313.

31. Maccauro G, Piconi C, Burger W, et al. Fracture of a Y-TZP ceramic femoral head. Analysis of a fault. J Bone Joint Surg Br. 2004; 86:1192–1196.
32. Masonis JL, Bourne RB, Ries MD, McCalden RW, Salehi A, Kelman DC. Zirconia femoral head fractures: a clinical and retrieval analysis. J Arthroplasty. 2004; 19:898–905.
33. Koo KH, Ha YC, Jung WH, Kim SR, Yoo JJ, Kim HJ. Isolated fracture of the ceramic head after third-generation alumina-on-alumina total hip arthroplasty. J Bone Joint Surg Am. 2008; 90:329–336.

34. Min BW, Song KS, Kang CH, Bae KC, Won YY, Lee KY. Delayed fracture of a ceramic insert with modern ceramic total hip replacement. J Arthroplasty. 2007; 22:136–139.

35. Toni A, Traina F, Stea S, et al. Early diagnosis of ceramic liner fracture. Guidelines based on a twelve-year clinical experience. J Bone Joint Surg Am. 2006; 88:Suppl 4. 55–63.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download