Abstract
The term tumoral calcinosis in used to describe the deposition of nodular calcareous masses in the soft tissue around large joints, such as the hips, shoulders, and elbows. Although the cause has not yet been clearly determined, according to the hypothesis, failure of phosphorus metabolism in the proximal tubule in kidney, chronic renal disease and hyperparathyroidism may cause tumoral calcinosis. No cases of tumoral calcinosis treated with surgical resection in chronic renal failure patients on hemodialysis, so called uremic tumoral calcinosis, have been reported in Korea. The authors experienced the case of a 57-year-old woman with chronic kidney disease on hemodialysis who presented with a mass around the hip. We made a diagnosis using plain radiographs, magnetic resonance imaging, and computed tomography of tumoral calcinosis, and treated the patient successfully with surgical resection. We report on a case of uremic tumoral calcinosis with a review of the literature.
Figures and Tables
Fig. 1
Anterior view of the pelvis shows huge bulging mass (arrows) located around the right proximal hip. There were no redness or skin lesion around the mass.

Fig. 2
Plain pelvic AP and lateral radiographs shows large radioopaque lesion at soft tissue around hip joint consisted of multiple round calcified masses.
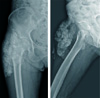
Fig. 3
(A) Coronal non-contrast T1-weighted image through the pelvis demonstrates 6.7×6.6×13.4 cm sized multiple conglomerated low signal mass around right iliotibial band, vastus lateralis and iliopsoas muscle. There was no definite enhancement in the lesion. (B) Coronal non-contrast T2-weighted image demonstrates dark signal mass. (C) Coronal T1-weighted enhance image shows no definite enhancement in the lesion.

Fig. 4
Three-dimensional computed tomography shows accumulation of multinodular calcareous deposits around right hip joint.
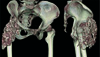
Fig. 5
(A) Intraoperative photographs shows protruded mass which is partially adherent to the adjacent muscles. (B) The mass contained highly concentrated whitish milk-like fluid.

Fig. 6
(A) The specimen was divided into two major chunks. And the size of each were 9.0×6.0×3.0 cm and 5.5×2.5×2.0 cm. (B) Bisection plane of the specimen shows yellow and white of the solid component with surrounding liquid component.

Fig. 7
Postoperative plain pelvis AP and lateral radiographs shows the clearance of calcified masses around the hip joint.

Fig. 8
(A) The lobules are separated by fibrous septa, with a lining of mixed fibrous and inflammatory tissue with surrounding soft-tissue fibrosis and inflammatory changes. (B, C) Microscopic pictures show amorphous eosinophilic material and many macrophages (hematoxylin & eosin stain; B, ×100; C, ×400).

References
3. Mitnick PD, Goldfarb S, Slatopolsky E, Lemann J Jr, Gray RW, Agus ZS. Calcium and phosphate metabolism in tumoral calcinosis. Ann Intern Med. 1980; 92:482–487.

4. Chalmers GW, Brown WR, Stienstra JJ. Tumoral calcinosis-like lesion of the foot. A case report. J Am Podiatr Med Assoc. 1998; 88:87–91.

6. Duret MH. Tumeurs multiples et singulieres des bourse sereuses. Bull Soc Anat Paris. 1899; 74:725–731.
7. Teutschlaender O. Lipid calcinosis. Zieglers Beitr. 1947; 110:402–405.
8. Martinez S, Vogler JB 3rd, Harrelson JM, Lyles KW. Imaging of tumoral calcinosis: new observations. Radiology. 1990; 174:215–222.

9. Smack D, Norton SA, Fitzpatrick JE. Proposal for a pathogenesis-based classification of tumoral calcinosis. Int J Dermatol. 1996; 35:265–271.

10. Olsen KM, Chew FS. Tumoral calcinosis: pearls, polemics, and alternative possibilities. Radiographics. 2006; 26:871–885.

11. Eisenberg B, Tzamaloukas AH, Hartshorne MF, Listrom MB, Arrington ER, Sherrard DJ. Periarticular tumoral calcinosis and hypercalcemia in a hemodialysis patient without hyperparathyroidism: a case report. J Nucl Med. 1990; 31:1099–1103.
12. Zins B, Zingraff J, Basile C, et al. Tumoral calcifications in hemodialysis patients: possible role of aluminum intoxication. Nephron. 1992; 60:260–267.

13. Benkert A, Tschammler A, Bahner U, Heidbreder E, Hahn D. The follow-up assessment of tumorous calcinosis before and after parathyroidectomy in secondary hyperparathyroidism. Rofo. 1994; 161:90–92.

14. Thomason AJS, Frewer JD, Marya SK. Accessory patella. An unusual presentation of tumoral calcinosis. Orthopaedics. 1996; 4:207–208.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download