Abstract
Purpose
We evaluate the clinical and radiographic midterm results of primary total hip arthroplasty (THA) using a 36 mm diameter femoral head on highly cross-linked polyethylene (minimum 7-year follow-up).
Materials and Methods
We retrospectively reviewed 73 patients (74 hips) that underwent primary THA with a 36 mm diameter femoral head on highly cross-linked polyethylene between July 2004 and February 2007. Clinical follow-ups included specific measurements like modified Harris hip scores (HHS) and Merle d'Aubigne and Postel score. For radiologic evaluations, together with position of acetabular cup at 6 weeks later of post-operation, we separately calculated the penentrations of femoral heads into polyethylene liners during post-operation and one year later check-ups, and during one year later check-ups and final check-ups.
Results
There were no complications except for one case of dislocation. Average modified HHS at final follow-up was 88±7.5 (range, 81-96), and Merle d'Aubigne and Postel scores were more than 15 (range, 15-18). Mean acetabular cup inclination and anteversion were 50.1°(range, 35°-58°) and 23.6°(range, 5°-38°), respectively. Average femoral head penetration during the first postoperative year was 0.071±0.034 mm/year, and steady-state wear rate determined using radiographs taken at one-year postoperatively and at latest follow-up was 0.051±0.022 mm/year. Average femoral head penetration during entire follow-ups was 0.058±0.013 mm/year.
Until today, total hip arthroplasty (THA) procedure has been recognized as the wonderful procedure in terms of patient's satisfaction. But, such a procedure also have a few complications. One of the most devastating is a dislocation1). Thanks to the advent of large diameter femoral head, we can lower a probability of dislocation after THA. But such a large head also have a few trade-off. What we must consider is a probability of increase in volumetric wear amount2). Large diameter femoral heads provide a means of reducing the risk of dislocation, but increases in wear debris have prevented the widespread use of this option in primary articulation3,4).
Highly cross-linked polyethylene was introduced for use in primary THA to reduce periprosthetic osteolysis due to a reduction in wear debris. Early and intermediate-term results of primary THA using highly cross-linked polyethylene bearing surfaces are promising4,5).
Base on these findings, we hypothesized that THA conducted using a 36-mm femoral head paired with highly cross-linked polyethylene would show low rates of dislocation and no appreciable wear debris. However, it is unclear whether these lower wear rates are really achieved in Korean population over long time beyond 7 years. Accordingly, the purpose of this study was to evaluate the clinical and radiographic midterm results of primary THA using a large diameter femoral head on highly cross-linked polyethylene (minimum 7-year follow-up).
We retrospectively reviewed 73 patients (74 hips) that underwent THA with a large diameter femoral head on highly cross-linked polyethylene between July 2004 and February 2007 (Table 1). Twenty-four cases out of 74 cases were osteonecrosis. One patient underwent both THA sequentially due to osteonecrosis of femoral head. We had also 2 cases of pathologic femoral neck fracture due to benign bone tumor. One of them was diagnosed as chondroblastoma. Mean patient age was 62 years (range, 21-86 years; 37 males and 36 females), and mean follow-up was 96 months (range, 84-122 months) (Table 2). A cementless acetabular cup with a porous coating (Trilogy®; Zimmer Inc., Warsaw, IN, USA) and a highly cross-linked polyethylene liner with an inner diameter of 36 mm (Longevity®: Zimmer Inc.) was placed in all patients. Based on surgeon's preference, one or two screw augmentations were adopted. Acetabular components had a average outer diameter of 54.7 mm (range, 50-62 mm). The polyethylene liners were machined from GUR 1050 polyethylene, which had been pre-heated and cross-linked with a 9.5 Mrad electron-beam. The preforms were then melted to eliminate the remaining free radicals and sterilized using a gas plasma. Fixture mount transfer (Zimmer Inc.) components were used in 66 case underwent cementless femoral fixation (Fig. 1) and Versys (Zimmer Inc.) components in 8 case underwent cemented femoral fixation. If cementless femoral stem had a unstable fixation intraoperatively, we used cemented femoral fixation regardless of patient's age. All cementless stems were inserted using standard press fit techniques to insure longitudinal and rotational stability, and all cemented femoral stems were inserted using meticulous third generation cementing techniques. All surgical procedures were performed by one surgeon (MRC) using a modified Harding's approach with the patient in the lateral position. Sixty patients underwent capsular repair closure. Prophylactic antibiotics were administrated to all 73 patients, and the same post-operative protocol was used in all. Patients were allowed to sit on the first postoperative day and stand with support, according to ability, after blood drainage removal. No range of motion (ROM) limitation was present immediately after surgery, and no abduction pillow was used in any patient.
Patients were followed at 6 weeks, and at 3, 6, and 12 months postoperatively. After then, we asked patients to visit every 6 months. The clinical and radiographic examinations were performed by an another orthopedic surgeon. Clinical follow-ups included specific assessments of possible dislocation. In addition, modified Harris hip scores (HHS) and Merle d'Aubigne and Postel score were determined. Modified HHS were classified as excellent (91-100), good (81-90), fair (71-80), or poor (61-70), and the Merle d'Aubigne and Postel scores were used to categorize patients to six grades according to level of pain (1-6), mobility (1-6), and the ability to walk (1-6).
In cases that underwent uncemented fixation, the status of fixation of femoral component was assessed using Engh et al.'s method6), and in cases that underwent cemented fixation, femoral components were assessed the amount of cement filling using Barrack et al.'s method7) using immediate postoperative radiographs. All radiographic examinations included an anteroposterior view of the pelvis centered over the pubis, and axial view by a shoot through lateral of the hip. Acetabular cup abduction angles were measured using Engh et al.8) and Kennedy et al's9) methods. Acetabular cup anteversion angles were measured using Widmer's10) method and it also calculated using polyWare pro three-dimensional (3D) distal version 5.10 software (Drafware Developers Inc., Vevay, IN, USA). The evidence of linear radiolucencies, bony ingrowth, fracture, and osteolysis were determined using sequential radiographic views, which also allowed comparative assessments of component position versus immediate postoperative views to determine the presence of component migration and/or loosening.
Penetrations of femoral heads into polyethylene liners were calculated as two-dimensional linear penetrations on anteroposterior radiographs of the pelvis using polyWare pro 3D distal version 5.10 software. In this program, wear rate is calculated through the 3-point marked on edges of the femoral head and acetabular cup using serial plain radiograph (Fig. 2). The mean total femoral head penetration was calculated by determining the magnitude of femoral head penetration shown first postoperative and final follow-up radiographs, and normalizing with respect to the duration of radiographic follow-up. The total penetration rate of the femoral head into the acetabular polyethylene is a result of the plastic creep and wear of the liner. To separate the early bedding-in process from steady-state wear, we also calculated mean total femoral head penetration shown by first post-operative and one-year radiographs and by one-year and final follow-up radiographs.
Average modified HHS at final follow-up was 88±7.5 (range, 81-96), and it was better than 'good' in all cases, and Merle d'Aubigne and Postel scores were more than 15 (range, 15-18) in all cases. There was no difference of functional hip scores in different causes of operation. But we could guess who had better previous hip functional scores had a tendency to earn the better post operation functional hip scores.
Radiographic final follow-up exams showed stable fixation in all patients with uncemented femoral components, and Barrack type A or B in all patients with cemented femoral components. Mean acetabular cup inclination and anteversion were 50.1°(range, 35°-58°) and 23.6°(range, 5°-38°), respectively. There was no radiographic evidence of osteolysis in the pelvis or proximal femur, and no acetabular cup or femoral stem failing due to aseptic loosening (Table 3).
But, one patient developed a hip dislocation. She sustained car accident and had a injury of femoral head posterior dislocation with acetabular fracture. After acetabular fracture fixation, she underwent THA due to secondary hip osteoarthritis. After one year of operation, she had a dislocation (Fig. 3). In this patient, anteversion of the index cup was 8°. The patient underwent isolated acetabular revision just after second dislocation, and has done routine indoor activity well since then.
In all patients, average femoral head penetration during the first postoperative year (predominantly representing polyethylene creep) was 0.071±0.034 mm/year, and the average steady-state wear rate determined using radiographs taken at one-year postoperatively and at latest follow-up was 0.051±0.022 mm/year. Average femoral head penetration during entire follow-ups was 0.058±0.013 mm/year.
Larger diameter femoral heads are believed to be less prone to dislocation and facilitate higher ROMs2). However, the widespread adoption of larger diameter femoral heads against conventional polyethylene is limited by the risk of accelerated wear and resulting osteolysis. The development of a new cross-linked polyethylene with improved wear characteristics, according to early laboratory and clinical studies, could reduce the risk of wear. Hip simulator studies have also demonstrated very low wear rates for even larger heads when a highly cross-linked polyethylene liners are used4,11). In other case of using 36- and 40-mm femoral head with a highly cross-linked polyethylene liner, Martell had a result of 0.075 mm/year wear rate in 5 to 8 years follow-up12). Our institute outcome is comparable with this result.
In the present study, even though one patient experienced a hip dislocation, patient satisfaction was high due to no ROM or hip posture limitation during the early post-operative period. However, despite the stability advantage observed during this study, the occurrences of this dislocation indicates the importance of proper orientation of the acetabular and femoral components during surgery13).
Polyethylene thickness is considered an important wear rate factor, a patient must have a 50 mm diameter acetabulum to allow a 36-mm femoral head to be used. When we used 50 mm diameter of acetabulum, the polyethylene thickness was 5.8 mm. On basis many opinions advocate that even though diameter of liner is just only 3 mm, this can be used without concerns of problematic wear increase relatively14), our research have used that implant system. Furthermore, now US Food and Drug Administration approved the use of more than 3 mm diameter of liner. But, this matter need more investigations. Even though insuring adequate polyethylene thickness may or may not be an issue with highly cross-linked polyethylene, this evidence concerns the increased wear rates of thin ultra high molecular weight polyethylene (UHWPE) liners11,15,16).
The early bedding-in of the femoral head resulting from plastic creep and other factors can confound early measurements of wear. Estok et al.17) reported a femoral head penetration resulting from creep of -0.1 mm for both conventional and highly cross-linked polyethylene. In the present study, the magnitude of femoral head penetration during the first postoperative year was 0.071±0.034 mm/year. On the other hand, steady-state wear rate was 0.051±0.022 mm/year. And, average femoral head penetration during entire follow-ups was 0.058±0.013 mm/year. However, it should be noted that the present study has limited statistical power because the cohort was not prospectively randomized. Also, we have some limitations in measuring wear rate. As to method of wear measurement, radiostereometric analysis (RSA) is the most accurate tool for in vivo assessment of polyethylene wear18). However, many radiographic in vivo studies of polyethylene wear in THA are restricted to measurements on plain radiographs because the RSA set-up is expensive and not widely available. Our institute used PolyWare software, which uses plain radiographs. PolyWare software does not supply the accuracy required, and for such situations we recommend RSA. For assessment of medium-term or long-term wear measurements in larger groups of patients, It is known as the PolyWare method is optimal, simple, and in relatively close agreement with the gold standard of RSA.
Nonetheless, the mid-terms results of primary THA with a 36 mm diameter femoral head on highly cross-linked polyethylene in patients was found to be comparable with in vitro laboratory hip simulation studies, and was found to be associated with high patient satisfaction due to no ROM or hip posture limitations during the early post-operative period. However, further follow-up studies are required to evaluate long-term wear-rates, the development of osteolysis, and the problem of the tribocorrosion developed between artificial head and neck of the stem.
Primary THA with a 36 mm diameter femoral head on highly cross-linked polyethylene was found to produce the low wear rates of 0.058±0.013 mm/year which comparable to previous in vitro laboratory hip simulation studies. In particular, patient satisfaction was high due to no ROM or hip posture limitation during the early postoperative period.
Figures and Tables
Fig. 1
Fifty-eight years man underwent with primary total hip replacement arthroplasty with 36 mm femoral head due to avascular necrosis of femoral head. Anteroposterior view of post-operation (A) and axial view (B).
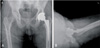
Fig. 2
If we designate 3 points at outer-shape of head and cup, PolyWare Pro three-dimensional program make circle-line automatically. The program calculates the penetration rate with comparing between initial X-ray circle line (A) and follow-up X-ray circle-line (B).

Fig. 3
Radiograph images. (A) Anteroposterior (AP) radiograph of 31-year-old woman showed posterior dislocation with acetabular fracture. (B) Acetabular was reducted and fixed with recon-plate. (C) AP radiograph showed a total hip replacement arthroplasty state using 36-mm femoral head with highly cross-linked polyethylene. (D) Dislocation state.

References
1. Sikes CV, Lai LP, Schreiber M, Mont MA, Jinnah RH, Seyler TM. Instability after total hip arthroplasty: treatment with large femoral heads vs constrained liners. J Arthroplasty. 2008; 23:7 Suppl. 59–63.
2. Rathi P, Pereira GC, Giordani M, Di Cesare PE. The pros and cons of using larger femoral heads in total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2013; 42:E53–E59.
3. Burroughs BR, Rubash HE, Harris WH. Femoral head sizes larger than 32 mm against highly cross-linked polyethylene. Clin Orthop Relat Res. 2002; 405:150–157.

4. Geller JA, Malchau H, Bragdon C, Greene M, Harris WH, Freiberg AA. Large diameter femoral heads on highly cross-linked polyethylene: minimum 3-year results. Clin Orthop Relat Res. 2006; 447:53–59.
5. Park CM, Cho MR, Kim SK, Choo WK, Kwon JB. Femoral head size of 36 mm against highly cross-linked polyethylene in patients younger than 60 years: minimun three years of follow up. J Korean Orthop Assoc. 2012; 47:28–34.

6. Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987; 69:45–55.

7. Barrack RL, Mulroy RD Jr, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg Br. 1992; 74:385–389.

8. Engh CA, Griffin WL, Marx CL. Cementless acetabular components. J Bone Joint Surg Br. 1990; 72:53–59.

9. Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998; 13:530–534.

10. Widmer KH. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004; 19:387–390.

11. Heisel C, Silva M, dela Rosa MA, Schmalzried TP. Short-term in vivo wear of cross-linked polyethylene. J Bone Joint Surg Am. 2004; 86-A:748–751.

12. Lachiewicz PF, Heckman DS, Soileau ES, Mangla J, Martell JM. Femoral head size and wear of highly cross-linked polyethylene at 5 to 8 years. Clin Orthop Relat Res. 2009; 467:3290–3296.

13. Barrack RL. Dislocation after total hip arthroplasty: implant design and orientation. J Am Acad Orthop Surg. 2003; 11:89–99.

14. Kelly NH, Rajadhyaksha AD, Wright TM, Maher SA, Westrich GH. High stress conditions do not increase wear of thin highly crosslinked UHMWPE. Clin Orthop Relat Res. 2010; 468:418–423.

15. Bradford L, Kurland R, Sankaran M, Kim H, Pruitt LA, Ries MD. Early failure due to osteolysis associated with contemporary highly cross-linked ultra-high molecular weight polyethylene. A case report. J Bone Joint Surg Am. 2004; 86-A:1051–1056.
16. Dowd JE, Sychterz CJ, Young AM, Engh CA. Characterization of long-term femoral-head-penetration rates. Association with and prediction of osteolysis. J Bone Joint Surg Am. 2000; 82-A:1102–1107.
17. Estok DM 2nd, Bragdon CR, Plank GR, Huang A, Muratoglu OK, Harris WH. The measurement of creep in ultrahigh molecular weight polyethylene: a comparison of conventional versus highly cross-linked polyethylene. J Arthroplasty. 2005; 20:239–243.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download