Abstract
Symptomatic aneurysmal bone cysts with expansible lesions in the pelvis are rare in children. The management of an aggressive vascular lesion in a female child is challenging. The standard treatment for aneurysmal bone cysts is accompanied by a high risk of local recurrence. A 12-year-old female presented with a history of pelvic pain for 5 months. Plain radiographs and magnetic resonance imaging showed a very large expansile lytic lesion arising from the right iliac bone. Intralesional curettage, electric cauterization, chemical sclerotherapy and allogeneic bone graft were performed through the window of the iliac crest. At a follow-up consultation 3.5 years post-surgery, the child had painless full-range movement in the hip joint with no recurrence. Although many treatment options are described, our patient was treated successfully using curettage and allogeneic bone graft without recurrence.
Although aneurysmal bone cysts are characterized by local damage and active lesions with in the blood stream, they have been classified as a benign tumor. These cysts are mostly swellings of eccentric form in the metaphyseal area of the upper or lower long bone and the posterior spine; bone destruction, pathological fractures, and local recurrence are some of the related problems. Common treatments for aneurysmal bone cysts include palliative curettage and bone grafting, selective artery embolic treatment, minimally invasive sclerotherapy, electric cauterization and partial resection1,2,3,4). However, the problem of these treatments is recurrence. For instance, in cases where 1) the patient is young; 2) the aneurysmal bone cyst is larger than 5 cm; and 3) if the location is difficult to access, the recurrence rate is 10-59%5). We report a case (with a relevant literature review) of a large aneurysmal bone cyst covering approximately 2/3 of the iliac bone, which was successfully treated without complications via a combination of several treatments.
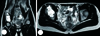
A 12-year-old female patient visited the hospital due to pain in her right pelvis and hip joint, which had started 5 months ago. The pain was dull and the patient walked with a slight limp. There was no pain radiating to the pelvic limb, but she complained of numbness in her right inner thigh. Physical examinations showed pressure pain around the right pelvis, while no oedema was noted. The patient did not have any pain in her right hip joint with passive range of motion and flexion, and there was no reduction in strength of the abductor muscle. An anteroposterior radiograph of the pelvis showed expansile osteolytic lesions throughout the acetabulum and right iliac bone. The lesions were invading up to the superior border of the acetabulum, but no lesions were found on the articular surface of the hip joint (Fig. 1). An magnetic resonance image showed well-defined multi-lobulated lesions with clear boundaries (11×9×5 cm) in the right iliac bone and the superior border of the acetabulum. The lesions showed multiple cysts with fluid-like signal intensity. Multiple fluid-fluid surfaces were detected in the cysts, suggesting a possibility of various levels of bleeding (Fig. 2). The patient was diagnosed with primary aneurysmal bone cyst, and subsequent biopsies and treatment were performed. A window (1×5 cm) was made on the crista iliaca and curettage was performed using a long curette; the lesions were filled with a vast amount of blood. Complete curettage was performed up to the superior border of the acetabulum, followed by electric cauterization of the inner surface of the iliac bone.
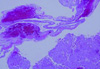
Lastly, the surgical area was washed with 30 mL of 70% ethanol. A commercially available allogeneic cancellous bone (60 mL), 'Cancellous coarse' (Community Tissue Services®, Kettering, OH, USA) was applied. Histological examinations of the tissues obtained from curettage confirmed the diagnosis of aneurysmal bone cysts, as they revealed 1) fibrous walls and septa containing blood components, 2) inflammatory cells and osteoclasts sparsely scattered around cystic spaces (Fig. 3). Three days post-surgery, the patient was able to move in a wheelchair. Partial weight bearing was started on crutches for up to 6 weeks. Six weeks post-surgery, full weight bearing was allowed. Follow-up consultation was done for 3.5 years. There was no local recurrence and the patient was able to walk without pain (Fig. 4).
Aneurysmal bone cysts are often found in metaphyseal area of upper or lower long bone, sternum, and spine, but usually not in the pelvic iliac bone. The occurrence rate for the pelvis is 8-12% but is slightly higher in young women (<20 years old)1). Aneurysmal bone cysts are very rarely found in children, and aggressive vascular lesions are challenging to treat properly. Treatment options should be carefully chosen depending on patients' age, the location of the lesions, their size and vascularity, and the degree of invasion. In the case presented here, we used a combination of previously reported treatments (intralesional curettage, electric cauterization, chemical sclerotherapy, and allogeneic bone graft), which resulted in a successful outcome without recurrence.
Curettage and bone grafting are known as palliative treatments for aneurysmal bone cysts2). However, the recurrence rate after either curettage or a combination of curettage and bond grafting is 13%1). Either selective artery embolic treatment or a combination of chemical sclerotherapy and electrocautery before surgery has been suggested to reduce recurrence2,3,4). Preoperative selective artery embolic treatment has been performed either as primary treatment or for difficult-to-access lesions; it has also been used to reduce operative bleeding3,4). However, artery embolic treatment is not easy to perform, since there is often more than one feeding artery in aneurysmal bone cysts. In addition, if a normal artery is invaded, ischemic necrosis may occur in normal tissues as well as nerves3). When it comes to pelvic aneurysmal bone cysts, embolic treatment should not be performed in lateral circumflex femoral arteries and pudendal arteries, which are distributed over sciatic, femoral and lateral femoral cutaneous nerves6).
Chemical sclerotherapy has been performed alone via a minimal invasive approach using phenol, polymethylmethacrylate, liquid nitrogen or ethanol. It can be also performed in parallel with other treatments such as curettage and embolization2). In this case, particular attention should be paid to prevention of other possible complications including burning sensation at the injection site, local pain, and cellulitis. Ethanol has been widely used as a sclerotherapy agent for malformations of soft tissues in the venous and lymphatic systems; Lambot-Juhan et al.7) reported that 90% of aneurysmal bone cysts could be treated with percutaneously applied ethanol. Notably, high doses of ethanol (higher than either 1 mL/kg body weight or 0.07% of ethanol in the blood) may cause dyspnoea, cardiac arrhythmias, convulsions and hypoglycaemia, hence the dose should be carefully determined and limited8).
Electric cauterization is normally performed with a bipolar electric cautery and is followed by appropriate palliative curettage. In most cases, it is performed in parallel with bone grafting. Electric cauterization is relatively simple and easy to apply, and is less expensive than other supplementary treatments. Furthermore, it results in a low occurrence rate of complications due to little impact on adjacent tissues4).
Prognostic factors for clinical outcomes of treatments of pelvic aneurysmal bone cysts are lesion sizes and patients' age. If the patient is younger than 16 years and the diameter of a lesion is >5 cm, frequent local recurrences and prolonged symptoms can be expected3). If the lesion is larger than 5 cm, there is a higher likelihood of complications such as medial dislocation of the femoral head, pathological fractures of the iliac bone, and sacrum invasion because of structural damage to the acetabulum. Therefore, active measurements are warranted, including en bloc excision, as well as comprehensive curettage3).
Although Agarwal et al.9) suggested that surgical resection would be the fundamental treatment for aneurysmal bone cysts in the iliac bone, maintaining stability and the range of motion of the hip joint should also be critical. Sharifah et al.10) addressed the technical difficulties and risks of a combination of partial resection and bone grafting for treating large aneurysmal bone cysts of the pelvis or spine and concluded that curettage along with bone grafting would be the best option.
In the present case report, a 12-year-old female patient had a vascular lesion, 11×9×5 cm in size, covering approximately 2/3 of the right iliac bone. The location of the lesion was found to be in the superior border of the acetabulum.
Because of commonly expected complications (e.g., dislocation of a hip joint) after en bloc excision or partial resection, in our case palliative curettage and bone grafting were chosen to minimize such risks. To minimize the risk of recurrence, a combination of electric cauterization and ethanol sclerotherapy were chosen, which were relatively easy and safe to perform as a supplemental treatments. Subsequently, allogeneic bone grafting was performed through the window of the iliac crest. Further investigations and case reports are warranted regarding other favourable lesions (e.g., metaphyseal area of upper or lower long bone and spine) as well as various sizes of lesions.
Overall, treatment should be carefully planned and consider the size, aggressiveness, and location of the lesions. In particular, it is recommended to adopt a combination of treatments rather than a single option to minimize the recurrence rate.
In conclusion, we herein report a successful case of treatment of primary aneurysmal bone cysts in the iliac bone, which did not result in any complications, via a combination of comprehensive curettage and bone grafting as a palliative treatment, along with supplemental treatments, chemical sclerotherapy and electric cauterization.
Figures and Tables
Fig. 1
Pre-operative anteroposterior radiograph of the pelvis showing an expansile osteolytic lesion involving to the superior border of the acetabulum with multiple septation.

Fig. 2
T2-weighted magnetic resonance imaging coronal view (A) shows 11×9×5 cm large, well defined lesion and axial view (B) shows multiseptations forming cysts containing fluid-like signal intensity.
References
1. Papagelopoulos PJ, Choudhury SN, Frassica FJ, Bond JR, Unni KK, Sim FH. Treatment of aneurysmal bone cysts of the pelvis and sacrum. J Bone Joint Surg Am. 2001; 83-A:1674–1681.

2. Campanacci M, Capanna R, Picci P. Unicameral and aneurysmal bone cysts. Clin Orthop Relat Res. 1986; 204:25–36.

3. Rossi G, Rimondi E, Bartalena T, et al. Selective arterial embolization of 36 aneurysmal bone cysts of the skeleton with N-2-butyl cyanoacrylate. Skeletal Radiol. 2010; 39:161–167.

4. Al-Qattan MM. Bipolar electric cauterization as adjuvant treatment after curettage of aneurysmal bone cysts of the hand. Ann Plast Surg. 2014; 72:38–40.

5. Cottalorda J, Kohler R, Chotel F, et al. Recurrence of aneurysmal bone cysts in young children: a multicentre study. J Pediatr Orthop B. 2005; 14:212–218.

6. Rossi G, Mavrogenis AF, Papagelopoulos PJ, Rimondi E, Ruggieri P. Successful treatment of aggressive aneurysmal bone cyst of the pelvis with serial embolization. Orthopedics. 2012; 35:e963–e968.

7. Lambot-Juhan K, Pannier S, Grévent D, et al. Primary aneurysmal bone cysts in children: percutaneous sclerotherapy with absolute alcohol and proposal of a vascular classification. Pediatr Radiol. 2012; 42:599–605.

8. Mason KP, Michna E, Zurakowski D, Koka BV, Burrows PE. Serum ethanol levels in children and adults after ethanol embolization or sclerotherapy for vascular anomalies. Radiology. 2000; 217:127–132.

9. Agarwal A, Goel P, Khan SA, Kumar P, Qureshi NA. Large aneurysmal bone cyst of iliac bone in a female child: a case report. J Orthop Surg Res. 2010; 5:24.

10. Sharifah M, Nurhazla H, Suraya A, Tan S. Pelvic aneurysmal bone cyst. Biomed Imaging Interv J. 2011; 7:e24.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download