The crescent fracture has been named by the shape of a fracture fragment of posterior superior iliac spine, which looks like a crescent. It has been reported in the literature when a strong lateral compression force is applied to the pelvis, the iliac fracture, as extended by the ipsilateral sacroiliac joints, occurs posterior fracture-dislocations of the sacroiliac joints. Posterior fracture fragment of ilium is placed normally near the sacrum due to the strong posterior ligaments of sacroiliac joint, and this fracture fragment is visible as a crescent shape in pelvis AP radiograph, so we call this fracture as crescent fracture. Also, this fracture occurs by the lateral compression force, by which the ligament of pelvic floor is not damaged, so the crescent fracture is unstable by rotational and stable by vertical shear force. We report a patient with atypical pelvic crescent fracture that is mainly influenced by vertical shear injury and is characterized by posterior fracture-dislocations of the sacroiliac joint. In this case report, we review the literature on classification and treatment of atypical type of crescent fracture.
CASE REPORT
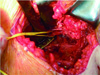
Forty five-year-old woman had a pelvic injury by falling from an apartment of three story, damage to the ipsilateral intertrochanteric area of femur and elbow comminuted fracture. She was hospitalized at other clinic and transferred to our hospital (Fig. 1, 2). The initial treatment of this patient was skeletal traction (Fig. 3). She was transferred to our hospital with improved general condition on 5 days after fall from height and had the operation on 7 days after accident. We choose the front approaches to reduce and fix the fracture of pelvic rami at the same operating field. We exposed the fracture site on supine position with the modified ilioinguinal approach which limits the original one to minimize the exposure of ilioinguinal neurovascular complex. Reduction of posterior fracture-dislocations of the sacroiliac joints was possible by using the indirect reduction technique which is fixing the end of preanatomical bending plate with a screw to the sacrum firmly and pull out the posterior dislocated fracture fragment of iliac wing by tightening of another screw in ilium. An another plate and screws was applied and fixed in front of the sacroiliac joints for reinforcement with 90-degree angle to previous plate. Surgical fusion of the sacroiliac joints was done to use the autogenous iliac cancellous bone graft after curettage of intra-articular cartilage. During the operation, we found the fifth lumbar nerve root descending anterior to adjacent sacrum and carefully applied the plate and screws not to irritate nerve (Fig. 4). Postoperatively she did not complained any neurologic symptom. Partial weight bearing started at postoperative 4-week follow-up, and full weight bearing was permitted at postoperative 8-week follow-up. At the last follow-up (2 year 6 months), she has regained her active daily living activities (Fig. 5).
DISCUSSION
Generally the crescent ilium fracture means posterior fracture-dislocations of the sacroiliac joint by lateral compression injury and the incidence of the crescent fracture is reported in approximately 10-15% of pelvic fractures4,5). In most cases, crescent fractures are type 61-B2.2 in AO/OTA classification and the lateral compression type II (LC II) in Young-Burgess classification. It is widely known that the crescent fracture is hemodynamically stable so, significant retroperitoneal hemorrhage is rare4,5).
Day and his colleagues1) classified the crescent fracture in 3 types depending on the size of the crescent fragment and the degree of dislocation. Type I is characterised by a large crescent fragment and the dislocation comprises no more than one-third of the sacroiliac joint, which is typically inferior. Type II fractures are associated with an intermediate-size crescent fragment and the dislocation comprises between one- and two-thirds of the joint. Type III fractures are associated with a small crescent fragment where the dislocation comprises most, but not all of the joint1). According to the crescent fracture classification, this case is classified to type III as demonstrated a crescent fracture of the left hemipelvis in which more than two-third of the sacroiliac joint was dislocated and is associated with a relatively small-sized crescent fragment.
In this presenting case, a buckling of anterior aspect of sacrum or sacral fracture, which is a specific finding of lateral compression injury, could not be seen on pelvis computed tomography, so we think the main fracture mechanism can be inferred from the vertical shear injury. Because ipsilateral fractured pubic rami is very unstable at manipulation and observed to move up and down during operation and contralateral fractured pubic rami is less unstable and less movable at same manipulation. So, the contralateral pelvic rami fractures are thought to be caused by a different mechanism. This case is thought to be type C1.2 in AO/OTA classification and can be rare event by vertical shear injury. It is notable in current case as the posterior fracture-dislocation of the sacroiliac joints was not reduced by the longitudinal skeletal traction for several days before surgery.
With surgical treatment, skeletal stabilization and early motion is possible, and depending on the surgeon's preference several surgical techniques can be considered, which are open reduction and internal fixation with plate and screws or with screws penetrating the sacroiliac joints4). Surgical approaches to the injured site are depending on the preference of the surgeons, are the front or rear access. In anterior internal fixation to reduce the injury of posterior pelvic soft tissue, two plates are fixed crossly with an angle past the sacroiliac joint. We highly recommend that the screw fixed to sacrum should be inserted only one, to prevent the injury of the fifth lumbar nerve roots driving forwards the sacrum. Posterior internal fixation could be performed in prone position, has benefits to dissect easily and safely and to fix accurately by direct exposure of dislocated sacroiliac joint. But neurologic, vascular and gastrointestinal complications are reported in fewer cases, and transarticular fixation could cause osteomyelitis4,5). This case is thought to be a good reference of surgical approaches about pelvic crescent fracture in the future.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download