Abstract
Purpose
To investigate the clinical and radiologic outcomes following treatment of intertrochanteric fractures using the Compression Hip Nail® (CHN), which has a sliding lag screw.
Materials and Methods
Twenty-eight cases of intertrochanteric fractures treated with CHN from November 2012 to October 2013 and followed-up for >6 months were included. The patient population consisted of 11 men and 17 women with a mean age of 75.2 years at the time of surgery. For the initial 11 cases, 10 mm sliding lag screws were used; the remaining 17 cases used 20 mm sliding lag screws. Clinical variables including operation time, amount of transfusion, weight-bearing start time, postoperative physical activity, and complications were investigated. The average sliding of lag screws and the average union were investigated radiologically at 3 and 6 months after surgery.
Results
In an analysis of 23 cases (exclusion of 3 cases of lag screw cutout and 2 cases of nonunion), 11 (48%) recovered their pre-injury activity level. In an analysis of 25 cases (exclusion of 3 cases of cutout), 17 (68%) and 23 (92%) showed radiological union at postoperative months 3 and 6, respectively. Seven complications were noted. Cutout of the lag screw and the lateral protrusion of barrels were significantly greater in the group with 10 mm sliding lag screws as compared to the group using 20 mm sliding lag screws.
Compression hip screws have been widely utilized as treatments for intertrochanteric fractures; however, high fixation failure rates have been reported when they have been used to treat unstable fractures1,2). Therefore, intramedullary nailing has become a commonly used treatment option in recently years, while replacement arthroplasty has become increasingly reserved for limited cases3,4,5,6).
The Compression Hip Nail® (CHN®; Tradimedics, Seongnam, Korea; Fig. 1) utilized in the current study possesses a few of the advantages associated with the proximal femoral nailing approach, and is also free from the protrusion of lag screws. Additionally, irritation of the trochanter has been minimized by the sliding barrels. The aim of the current study was to examine the clinical and radiological outcomes of intertrochanteric fractures treated with the CHN.
Of the 43 cases of intertrochanteric fractures seen from November 2012 to October 2013, a total of 28 cases treated with CHN® in our orthopedics department and followed up for >6 months were included in the current study. Follow-up for 15 cases was not possible due to deaths and other patient-specific issues. Operations were performed by 2 surgeons and analyzed retrospectively. Eleven patients were male and 17 patients were female. The average age at surgery was 75.2 years (range, 44-89 years) and the average follow-up period was 9.2 months (range, 6.1-16.5 months). As per Evans' classification7), 17 cases were stable fractures and 11 cases were unstable fractures.
Patients under either general anesthesia or lower-body anesthesia were placed in the supine position on the fracture bed prior to being moved. The operation was started upon confirmation of successful reduction through the use of an image amplification device. In some cases, the reduction of posteromedial bone fractures was conducted via a percutaneous operation. Once the location of the greater trochanter was confirmed, a skin incision approximately 5 cm long was made in parallel with the long axis of the femur from the apex through the proximal greater trochanter.
A small split window was made on the glutaeus maximus and musculus glutaeus medius so that a guide pin could be inserted on the apex of the greater trochanter. Once the location of the guide pin was confirmed to be in the middle of the medullary cavity of the bone utilizing an image amplification device, an insertion site for the intramedullary nail was made with a power reamer prior to insertion of the proximal femoral nail.
The lag screws combined with a barrel were placed in the middle of the head of the femur with the aid of anteroposterior and lateral images from the image amplification device, and inserted considering the appropriate tip-apex distance (TAD). In 25 cases, 1 distal locking screw was inserted, while 2 locking screws were used in the other 3 cases. Two types of end caps, static and dynamic, were used. Dynamic end caps were inserted through the proximal screw grooves of the intramedullary nails while closely attaching to the convexo-concave surface of the upper part of the barrel, thereby holding the barrel on the intramedullary nail and allowing sliding of the lag screws in the barrel. In contrast, static end caps were slightly longer and could be inserted even deeper, distorting the upper part of the barrel and hindering the sliding of lag screws via a tight attachment between the barrel and lag screws. In the current study, the extension cap was used after the dynamic end cap, instead of the static end cap, in order to allow lag screws to slide in all cases. A drainage tube was not inserted in the surgical incision window. Once the operation was completed, walking with the aid of a walker as soon as possible was recommended, and weight-bearing was also allowed. In advance of walking, patients were periodically subjected to an air pressure device in order to prevent cardiac arrhythmia thrombus. For the initial 11 cases, 10 mm sliding lag screws were used; 20 mm sliding lag screws were chosen for later 17 cases as suggested by the authors.
Clinically, operation time, amount of transfusion, and start time of weight-bearing with a walker were investigated based on the medical records from all cases. Except for the 5 cases who underwent reoperation due to cutout of 1 or more lag screws or fracture non-union, functional recovery as well as postoperative physical activity were analyzed in 23 cases using the modified Koval index8,9)(Table 1). Radiologically, TAD10) and the Cleveland index11) were measured in 28 cases that were available for follow-up at >6 months. Except for the 3 reoperation cases (due to cutout of 1 or more lag screws or fracture non-union), sliding of lag screws was measured immediately after the surgery and at the end of follow-up period in 23 cases. Furthermore, the bone union was evaluated after 3 and 6 months of surgery. The bone union was defined by the formation of a bony callus observed in the anteroposterior and lateral radiological images, as well as an absence of pain as self-reported by the patients.
For statistical analysis, PASW Statistics ver. 18.0 (IBM Co., Armonk, NY, USA) was utilized. The multivariable logistic regression analysis was performed in order to analyze correlations between sliding distance before and after improvement of lag screws, sex, age, Evans' classification, TAD, Cleveland index, and occurrence of complications. Chi-squared tests and t-tests were performed to analyze differences in sex, age, sliding distance, and TAD between stable and unstable fractures as suggested by the Evans'classification. A P-value <0.05 was considered statistically significant.
The average operation time for all cases was 65 minutes (range, 40-140 minutes). In cases when the hemoglobin level was less than 8.0 (18 cases, 64%), an average of 2.4 units of red blood cell concentrate (range, 1-4 units) was transfused. The average time to weight-bearing was 2.7 days (range, 2-4 days) after the operation. Except for 5 patients who underwent reoperation due to cutout of 1 or more lag screws or fracture non-union, pre- and postinjury ambulatory ability was compared in 23 cases. Results indicated a score of 3.9±0.7 at the final follow-up, which was decreased as compared to a mean preinjury score of 4.3±0.8. In 11 (48%) cases, ambulatory ability was fully recovered, while it worsened in 12 cases (52%; Table 2).
In all cases, the average of TAD measured after the surgery was 20.6±6.77 mm. Regarding the Cleveland index, 2, 4, and 12 cases were well located in regions 2, 3, and 5, respectively. Additionally, 7 and 3 cases were located in regions 6 and 8, respectively, which accounted for 71% of all cases. Of 25 cases (excluding 3 patients who had replacement arthroplasty due to cutout of 1 or more lag screws; Fig. 2), 17 (68%) and 23 (92%) showed radiological union at postoperative months 3 and 6, respectively (Fig. 3). Reoperation was performed in 2 cases that did not show radiological union at postoperative month 6. The average sliding distance of the lag screws was 7.6±4.5 mm (0.4-15.9 mm) in 23 cases (excluding 5 cases of reoperation due to cutout of 1 or more lag screws or fracture non-union; Table 3).
Complications were noted in 7 cases (21%): cutout of the lag screws in 3 cases (11%), non-union in 2 cases (8%), lateral protrusion of barrels in 1 case (4%) and fractures around the inserts in 1 case (4%). One patient had both lateral protrusion of barrels and non-union simultaneously (Fig. 4). The TAD was >25 mm in 1 of the 3 cases of cutout of the lag screws and in 1 of the 2 cases of non-union. No significant association was found between sex, age, Evans'classification, TAD, or Cleveland index in the multivariable logistic regression analysis (P=0.295, 0.377, 0.564, 0.135, and 0.096 for sex, age, Evans' classification, TAD, and Cleveland index, respectively).
One case of lateral protrusion of barrels and 3 cases of cutout of the lag screws were found in the group with the 10 mm sliding lag screws (n=11), while only 1 case of non-union was found in the group with 20 mm sliding lag screws. Furthermore, no cases were noted to display lateral protrusion of barrels as well as cutout of the lag screws in the group with the 20 mm sliding lag screws. The complication occurrence rate was significantly higher in the group with the 10 mm sliding lag screws as compared to that observed for the group who used the 20 mm sliding lag screws (P=0.03).
No statistical differences in sex (chi-square test, P=0.315), age, TAD, and sliding distance (t-test, P=0.531, 0.966, and 0.643, respectively) were found between stable and unstable fractures as defined per the Evans' classification. Other medical complications including myocardial infarction, pulmonary embolism, and stroke were not observed.
Intertrochanteric femoral fractures are very commonly observed, account for approximately half of all hip fractures12), and result in loss of independent living skills, as well as incomplete recovery of physical ability in approximately 50% of cases13,14,15). Several treatment options, such as compression hip screws, metal plates, and intramedullary nails are available, while replacement arthroplasty is performed only in limited cases3,4,5,6). These approaches represent various advantages and disadvantages, and therefore, a number of studies regarding their clinical outcomes have been reported13). Recently, the use of intramedullary nailing is increasing, as it can be applied for almost all fracture cases including reverse oblique fractures and high subtrochanteric fractures. Additionally, intramedullary nailing is among the more minimally invasive techniques and allows for earlier weight-bearing17,18,19).
Several studies have reported on the operation time associated with the use of intramedullary compression hip screws and intramedullary nails with varying results. In the current study, the average operation time was shown to be 65 minutes, which is somewhat similar to other reports20). The average of amount of transfusion was approximately 2.4 units, a result that was slightly higher than that of a previous study20) and which may have been attributable to the high proportion of patients (6, 21%) who were taking anticoagulants such as aspirin.
Schipper et al.22) asserted that the cutout of lag screws was most likely due to the position of the screws rather than issues with the instruments. In the current study, we found that TAD results were favorable and that no complications were noted due to TAD. For the initial 11 cases, the 10 mm sliding lag screws were used; however, the 20 mm sliding lag screws were chosen for the later 17 cases. It is important to note that we only found the cutout of lag screws and the lateral protrusion of barrels in the initial cases that used the 10 mm sliding lag screws. Furthermore, in the radiological images of all cases of cutout, the sliding of the lag screws reached the upper limit of 10 mm, suggesting that the cutout of the lag screws may have been attributable to the pressing force applied to the fractures once the screws reached their maximal sliding distance (i.e., 10 mm). Upon modification of the maximal sliding distance up to 20 mm, such complications were not found. Given these results, sliding distance is considered as an important factor for the cutout of lag screws, and the optimal sliding distance for lag screws would be approximately 20 mm.
One case of fractures around nails was due to an additional injury from a fall. Other than 1 case of non-union, no complications were observed in the group with the 20 mm sliding lag screws.
The current study had several strengths. First, we investigated the effects of sliding lag screws on clinical and radiological outcomes that had not received a great deal of previous attention. Second, the current study investigated the clinical outcomes of surgical instruments manufactured domestically, which may be helpful in advancing the further development of Korean instruments and related business interests. Lastly, the results of the current study demonstrated that clinical surgical outcomes were improved through the advances in instruments based on surgeons' needs and may serve to emphasize the advantages of utilizing domestic instruments with regard to the selection and development of instruments in the future.
The current study also had several limitations. First, the statistical power of the study was relatively weak due to the small sample size. Second, all surgeries were performed by 2 surgeons and this may have had an influence on the surgical outcomes. Third, even though all operations were conducted by 2 independent surgeons, we did not compare them to each other. Lastly, we were not able to evaluate bone mineral density in all cases, and thus related analyses were not performed. Taking into account the aforementioned weaknesses, further prospective studies with larger numbers of subjects are warranted.
The results of CHN use for the treatment of intertrochanteric fractures were shown to be poor due to a high complication rate. In contrast, clinical outcomes were more favorable in the group with the 20 mm sliding lag screws. Collectively, these results support a recommendation for the use of the 20 mm sliding lag screw for the treatment of intertrochanteric fractures.
Figures and Tables
Fig. 1
Gross photograph of assembled Compression Hip Nail® (Tradimedics, Seongnam, Korea). (A) Pre-sliding state, the doubleheaded arrow denotes pre-sliding length. (B) Post-sliding state, the arrow denotes lateral protrusion of the lag screw did not occur even when the lag screw slided completely.
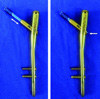
Fig. 2
(A) Immediate postoperative hip anteroposterior radiograph of 80 years old female. (B) Cutout of the lag screw was observed on postoperative 1 month radiograph. (C) Total replacement arthroplasty was done.
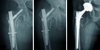
Fig. 3
(A) Hip anteroposterior (AP) radiograph of 82 years old female patient shows unstable intertrochanteric fracture. (B) Immediate postoperative radiograph shows well reduced fracture. (C) Postoperative 6 months, hip AP radiograph shows solid union of fracture and 4.5 mm sliding of lag screw without lateral protrusion of lag screw. White arrows indicate pre- and post-sliding lengths.
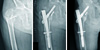
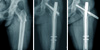
Fig. 4
(A) Hip anteroposterior (AP) radiograph of 82 years old female patient shows unstable intertrochanteric fracture. (B) Immediate postoperative radiograph. (C) Postoperative 6 months, hip AP radiograph shows lateral protrusion of the barrel.
References
1. Flores LA, Harrington IJ, Heller M. The stability of intertrochanteric fractures treated with a sliding screw-plate. J Bone Joint Surg Br. 1990; 72:37–40.

2. Davis TR, Sher JL, Horsman A, Simpson M, Porter BB, Checketts RG. Intertrochanteric femoral fractures. Mechanical failure after internal fixation. J Bone Joint Surg Br. 1990; 72:26–31.

3. Dávid A, von der Heyde D, Pommer A. Therapeutic possibilities in trochanteric fractures. Safe--fast--stable. Orthopade. 2000; 29:294–301.
4. Ostermann PA, Haase N, Ekkernkamp N. Techniques of extramedullary osteosynthesis in proximal femoral fractures. Chirurg. 2001; 72:1271–1276.
5. Kim SS, Lee KY, Kim CH, et al. Comparison of the dyna locking trochanteric nail, proximal femoral nail antirotation and gamma 3 nail in treatment of intertrochanteric fracture of the femur. Hip Pelvis. 2013; 25:211–219.

6. Kho D, Nam K, Kang D, Kim H. Bipolar Hemiarthroplasty using calcar replacement stem for unstable intertrochanteric femoral fracture in elderly patients. Hip Pelvis. 2013; 25:203–210.

7. Evans EM. The treatment of trochanteric fractures of the femur. J Bone Joint Surg Br. 1949; 31B:190–203.

8. Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995; 310:150–159.
9. Koval KJ, Zuckerman JD. Functional recovery after fracture of the hip. J Bone Joint Surg Am. 1994; 76:751–758.

10. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995; 77:1058–1064.

11. CLeveland M, Bosworth DM, Thompson FR, Wilson HJ Jr, Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959; 41-A:1399–1408.

12. Chapman MW. Fractures of the hips and proximal femur. In : Chapman MW, editor. Chapman's Orthopaedic Surgery. 3rd ed. Philadelphia: Lippincott Williams & Wilkins;2001. p. 634–650.
13. Ganz SB, Peterson MG, Russo PW, Guccione A. Functional recovery after hip fracture in the subacute setting. HSS J. 2007; 3:50–57.

14. Pajarinen J, Lindahl J, Michelsson O, Savolainen V, Hirvensalo E. Pertrochanteric femoral fractures treated with a dynamic hip screw or a proximal femoral nail. A randomised study comparing post-operative rehabilitation. J Bone Joint Surg Br. 2005; 87:76–81.
15. Banan H, Al-Sabti A, Jimulia T, Hart AJ. The treatment of unstable, extracapsular hip fractures with the AO/ASIF proximal femoral nail (PFN)--our first 60 cases. Injury. 2002; 33:401–405.

16. Moon YW, Suh DH, Kang ST, Kwon DJ, Ji YN, Lee KB. The proximal femoral nail for intertrochanteric fracture of the femur. J Korean Soc Fract. 2003; 16:29–36.

17. Lorich DG, Geller DS, Nielson JH. Osteoporotic pertrochanteric hip fractures: management and current controversies. Instr Course Lect. 2004; 53:441–454.
18. Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg Am. 2001; 83-A:643–650.

19. Kyle RF, Gustilo RB, Premer RF. Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg Am. 1979; 61:216–221.

20. Shin DK, Kwun KW, Kim SK, Lee SW, Choi CH, Kim KM. Proximal femoral nail (PFN) for femur intertrochanteric fracture. J Korean Soc Fract. 2002; 15:328–335.

21. Steinberg GG, Desai SS, Kornwitz NA, Sullivan TJ. The intertrochanteric hip fracture. A retrospective analysis. Orthopedics. 1988; 11:265–273.

22. Schipper IB, Steyerberg EW, Castelein RM, et al. Treatment of unstable trochanteric fractures. Randomised comparison of the gamma nail and the proximal femoral nail. J Bone Joint Surg Br. 2004; 86:86–94.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download