INTRODUCTION
The position of the implant is a critical factor influencing both functions and outcomes of total hip arthroplasty (THA)1). If it is located in an appropriated position, favorable clinical outcomes are expected in terms of longevity of the implant, range of motion, dislocation rates, and other parameters2,3,4). For artificial prostheses, a 'safe zone' of the acetabular cup location is generally recommended (40°±10°in inclination and 15°±10°in anteversion)5). Malposition of the acetabular cup is an important factor that increases the probability of the need for revision THA6).
Thus far, several methods have been suggested to be helpful for positioning the acetabular cup within the safe zone, such as preoperative templating, anatomical landmarks, and mechanical accessories for alignment1). A computer-assisted navigation system has been reported to lower the occurrence rate of outliers for acetabular cup position17), and suggested to be useful to avoid malpositioning of the acetabular cup for THA in patients with serious acetabular deformity8,9,10,11) as well as revision THA12,13,14).
Although computer-assisted navigation system-facilitated acetabular cup fixation has been introduced in South Korea, no domestic literature regarding clinical outcomes of such approach is available. The authors hypothesized that an image-free computer-assisted navigation system would be effective in lowering the risk of malposition of the acetabular cup in either THA in patients with acetabular deformity or revision THA. The purpose of this study was to test this hypothesis by retrospectively analyzing short-term follow-up results of acetabular cup fixation.
MATERIALS AND METHODS
A total of 103 patients were included who underwent THA from February 2011 through February 2013. Among them, 28 patients (16 THA cases and 12 revision THA cases) who (i) underwent acetabular cup fixation using an image-free navigation system (Orthopilot THA navigation system 3.1; B.Braun-Aesculap, Tuttlingen, Germany) and (ii) were eligible for radiological and clinical follow-up for at least 1 year were retrospectively analyzed. The average follow-up period was 17.1±5.3 months (range, 12-24 months). Among the 16 cases of THA, acetabular deformity was found in 8 cases of posttraumatic arthritis, 6 cases of hip dysplasia, and 2 cases of sequels of Legg-Calvé-Perthes disease. The 12 cases of revision THA included 6 cases of acetabular cup loosening, 2 cases of loosening of the acetabular cup and femoral stem, 2 cases of acetabular erosion after bipolar hemiarthroplasty, and 2 cases of ceramic liner fractures.
In the revision THA group, no dislocations were noted between THA and revision THA. When the 2 cases of acetabular erosion were excluded, malposition of the acetabular cup right after surgery was noted in 7 out of the 10 remaining cases. In 3 of these 10 cases, the position of the acetabular cup was changed due to osteolysis and loosening. In 2 of these 7 malposition cases, ceramic liner fractures were also found; these fractures occurred 1.5 years and 8 years after THA.
By the time of surgery, the average age of the patients was 66.1±6.1 years (range, 56-81 years); the average body mass index was 24.8±3.1 kg/m2 (range, 17.9-29.3 kg/m2). In all cases, the acetabular cup Plasmacup® (B.Braun-Aesculap) was used. The following femoral stems were used: Bicontact® (B.Braun-Aesculap; 8 cases), Excia® (B.Braun-Aesculap; 7 cases), and Solution® (Zimmer, Winterthur, Switzerland; 2 cases). Logica® (Lima, Udine, Italy) and Metha® (B.Braun-Aesculap) were also used in each case. Polyethylene (Chirulen®; Meditech, Plochingen, Germany) on ceramic (BIOLOX Forte®; Ceramtec, Plochingen, Germany) was used as a bearing surface in all cases except one. The average size of the acetabular cup was 56.1±5.6 mm (range, 44-66 mm). The acetabular cup was press-fitted in 8 cases of THA and 2 cases of revision THA. In 8 cases of THA and 10 cases of revision THA, the acetabular cup was fixed using line-to-line fixation with 2 or 3 screws.
Detailed operative procedures for acetabular cup fixation using the navigation system were as follows: 1. The software program provided by the supplier was started (THACup only FS219; B.Braun -Aesculap); 2. Following the instructions, a camera was installed 2 m in front of the surgical site and patient's shoulder joint; 3. The camera was aimed at the surgical site at a 45° angle; 4. After anesthesia, a screw was inserted in the iliac crest in a supine position in order to mount a transmitter; 5. Using image amplification, anatomical reference points (both anterior superior iliac spines and symphysis pubis) were subsequently scanned with a probe and then registered in the image-free navigation system. After registration, the patient was asked to change their position to lateral; additional time was required before performed a surgical approach. In all cases, a posterolateral approach was used.
Once the joint was opened, acetabular reaming was performed while monitoring changes in inclination and anteversion (shown on the image-free navigation system screen) and making certain that both values are within the safe zone5). The acetabular cup was then inserted while the values of inclination and anteversion were within the safe zone. During insertion of the femoral stem, its anteversion angle was measured relative to the posterior lesser trochanteric line15,16). The latter connects the apical posterior lesser trochanter and the posterolateral femoral cortical bone; previous studies using computed tomography (CT) addressed the usefulness of the posterior lesser trochanteric line for predicting the anteversion of the femoral stem15,16). The joint was reduced and its stability as well as soft tissue tension were evaluated. In the cases of either unsatisfactory joint stability or unequal length of the legs, additional surgical operations were performed to improve joint stability such as insertion of an elevated liner, changing the size and length of the femoral head, and replacement of femoral stem. Two to three days after surgery, the patients were recommended to start active joint exercise and to move in a wheelchair; a week after surgery, the patients started to gradually increase weight-bearing exercises according to their physical condition.
Radiological inclination and anteversion of the acetabular cup were measured using the method of Widmer17). Anteroposterior radiological images of the hip joint at the final follow up were acquired using Picture archiving and communication systems (PACS; Infinite, Seoul, Korea) interfaced with PiViewStar Version 5080 software (Infinite). Radiological images were taken of both sides of the hip joint and symphysis pubis unit at the center. When taking images, particular care was taken to avoid any rotation and inclination of the pelvis in relation to the vertical and horizontal axes. Two orthopedic surgeons (observers 1 and 2), who did not participate in the operations, assessed inclination and anteversion of the acetabular cup. The intraobserver and interobserver intra-class correlation coefficient (ICC) for inclination and anteversion were 0.95, 0.96, 0.92 and 0.89, 0.91, 0.87, respectively.
As mentioned above, the safe zone was set as 40°±10°for inclination and 15°±10°for anteversion of the acetabular cup5) and then the results of radiological data and the image-free navigation system analyzed if they are distributed within that zone. In addition, Pearson's correlation coefficients were determined to assess the correlation between the results of the image-free navigation system and simple radiological data; the results were visualized using scatter plots. To evaluate clinical outcomes, preoperative and last follow-up Harris hip scores were compared; in addition, the occurrence of complications was also assessed. For statistical analyses, SPSS software version 10.1 (SPSS Inc, Chicago, IL, USA) was used; P-values <0.05 were considered statistically significant.
RESULTS
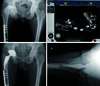
The average inclination and anteversion of the acetabular cup were 38.5°±4.7°(range, 32°-50°) and 16.6°±4.0°(range, 8°-23°), respectively, when measured with the image-free navigation system. According to the simple radiological data, the average inclination and anteversion were 40.5°±4.6°(range, 32°-50°) and 19.5°±4.2°(range, 8°-25°), respectively. Regardless of the method used, all values were within the safe zone (Fig. 1, 2). There was a statistically significant correlations between the data from the image-free navigation system and simple radiology (inclination: r=0.88; anteversion: r=0.85, P<0.05). The Harris hip score was significantly improved (P<0.05) after surgery: 52.3±14.4 points (range, 29-87 points) before the operation vs. 88.0±9.0 points (range, 65-99 points) after the operation. No dislocations or acetabular cup loosening were found (Fig. 3, 4). Postoperative complications were found in two cases. Metallosis was reported in one patient 18 months after revision THA that used a metal femoral head and polyethylene liner; metallosis was likely due to ceramic liner fracture. This patient underwent re-revision THA using a ceramic-on-ceramic bearing surface and did not report any further complications except for mild limping 6 months after surgery. In another case, a patient with posttraumatic osteoarthritis experienced nerve injury due to excessive bleeding after surgery; although conservative treatment was provided, the patient had foot drop and muscular weakness (muscle power: 4th grade) 1 year after the surgery. Currently, the patient is under rehabilitation.
DISCUSSION
In the present study, the authors investigated 28 cases of acetabular cup fixation using an image-free navigation system for THA patients with acetabular deformity and revision THA; in all cases, the acetabular cup was within the safe zone according to radiology and the data from the image-free navigation system. No dislocations or acetabular cup loosening were noted, whilst the Harris hip score was significantly improved in all cases. Therefore, the authors conclude that the image-free navigation system helps to prevent malpositioning of the acetabular cup as well as related complications.
Of the 12 revision THA cases, malposition of the acetabular cup was reported in 7 out of 10 cases (when 2 cases with acetabular erosion were excluded) (Fig. 4); in 3 of these 10 cases, the position of the acetabular cup was changed due to osteolysis and loosening. Considering that malposition of the acetabular cup is one of the most important factors that increase chances that revision THA will be needed6), our results indicate that positioning the acetabular cup in the safe zone is necessary for the longevity of artificial joints. Furthermore, in 2 cases, ceramic liner fractures in addition to the malposition of the acetabular cup were found, which made it difficult to completely remove ceramic particles and select the bearing surface, in line with other reports18,19,20). In one case of ceramic liner fracture, metallosis was observed 18 months after the operation (revision THA), hence re-revision arthroplasty was performed. Given the increasing use of ceramic-onceramic bearing surfaces and their intrinsic properties (they are more brittle than other bearing surfaces and thus are more vulnerable to mechanical damage)21), more efforts should be made to place the acetabular cup within the safe zone as much as possible when performing THA in order to secure the longevity of the artificial hip joint and to prevent ceramic liner fractures.
In cases of accompanying acetabular deformity, it is extremely difficult to place the acetabular cup within the safe zone even when THA is performed by skillful surgeons11,22,23,24). This is because anatomical landmarks, which aid in appropriate positioning of the acetabular cup, become less useful due to acetabular deformity, bone defects, and the absence of soft tissues (e.g., normal acetabular margin and transverse acetabular ligament)22,25). Furthermore, frequent subchondral sclerosis due to degenerative changes makes subsequent acetabular reaming difficult while maintaining the proper position of reamer. Bone defects after revision THA may be caused by either osteolysis or acetabular reaming. Such defects also hinder the insertion of the acetabular cup within the safe zone12,13,14). In addition, according to a study on the learning curve of surgeons who perform acetabular cup insertion26), at least 50 attempts of acetabular fixation are required for stable and successful insertion of the acetabular cup within the safe zone. However, THA in patients with acetabular deformity and revision THA are not common, hence a stable learning curve might not be achieved as expected. For example, although the authors had experience of at least 50 cases of acetabular cup fixation per year, only 10 cases per year could be considered as uncommon. Because of the difficulties in securing a stable learning curve, the authors used an image-free navigation system, which enabled monitoring changes in inclination and anteversion with simultaneous acetabular reaming and successful insertion of the acetabular cup within the safe zone, which resulted in favorable radiological and clinical outcomes. In this study, we found a statistically significant correlation between the results of assessment using the navigation system and radiology. However, there is inconsistency between the both results. Although the cause of this difference was not analyzed in the study, it might be due to differences in body mass index27), thickness of the soft tissue28), pelvic tilt29), or racial differences in pelvic shape30). Additional investigations regarding such inconsistency are warranted.
There are several limitations of this study. First, we did not measure postoperative anteversion of the femoral stem, which made it impossible to measure combined anteversion predicted during surgery. Additional studies regarding this issue are needed. Second, this study retrospectively analyzed a small number of cases and did not have a control group. Third, due to characteristics of our institution, we had a biased sex ratio; therefore, prospective randomization clinical trials are needed for objective analysis. Lastly, since we did not perform CT scans (which were performed in the previous studies31,32)), the accuracy of the image-free navigation system could not be objectively evaluated.
CONCLUSION
As demonstrated in the present study, image-free navigation system-assisted acetabular cup fixation prevented malpositioning of the acetabular cup as well as complications in THA in patients with acetabular deformity and revision THA. Such clinically favorable results warrant further long-them follow-up studies and additional investigations.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download