INTRODUCTION
Cementless total hip arthroplasty (THA) has been associated with favorable results at both mid- and long-term follow-ups1,2). To achieve long-term survival rates of the cementless components, several biological fixation methods have been introduced3,4). As several studies have demonstrated that hydroxyapatite (HA) is a non-toxic, biocompatible, and osteoconductive material that enables strong osteointegration in a short period of time, HA coatings have long been used in THA. The ABG-I (Anatomical Benoist Giraud, Howmedica, London, UK) prosthesis, designed in the 1980s as an acetabular cup and a proximal femoral stem with a surface coating of HA, has shown good clinical and radiological results by achieving stable biological fixation between the prosthetic components and the femur in studies with relatively short follow-up periods5,6,7). However, the acetabular cup revision rate is reported to be high and attributable to acetabular osteolysis caused by polyethylene wear8,9,10). Although HA-coated acetabular cups have shown unfavorable outcomes, HA-coated femoral stems have been associated with more favorable outcomes11,12,13,14). Despite positive results based on the femoral components, HA-coated prostheses have failed to show better clinical and radiological results than porous-coated prostheses at mid- and long-term follow-ups. Therefore, the use of HA-coated components in THA remains controversial15,16). The aim of the current study was to investigate the radiological results and survival rates associated with the use of HA-coated anatomical femoral stems in patients who underwent THA and were followed-up for ≥12 years.
MATERIALS AND METHODS
Of the 178 hips that received THA with HA-coated hip prosthesis from April 1992 to May 1997, this study comprised 86 patients (102 hips) who underwent THA with HA-coated ABG-I prosthesis and were able to undergo radiography at the final follow up. We excluded 17 deceased subjects and 59 hips that could not be traced. Study subjects included 64 men (79 hips) and 22 women (23 hips). THA was performed on the right side in 55 hips and on the left side in 47 hips. The mean age at the time of surgery was 53.4 years (range, 30-75 years), and the mean duration of follow-up was 17.1 years (range, 12.1-21 years). The causes of THA were avascular necrosis of the femoral head in 89 cases (87%), osteoarthritis in 9 cases (8%), infectious disease in 3 cases (3%), and fracture around the hip in 1 case (1%).
In the current study, ABG-I was used as an anatomical femoral stem prosthesis composed of a titanium alloy (Ti6Al4V) and designed to achieve maximum fixation with a press-fit in the metaphyseal region. The proximal third of the femoral stem was coated with HA on a macro-relief surface to a thickness of 60±10µm through a plasma spray, and the distal part had a grit-blasted surface (roughness, 2.59µm) without HA coating. The ABG-I HA-coated acetabular cup was used in all cases.
All operations were performed by a single surgeon, and THAs were performed in a lateral position using a posterolateral approach without involving greater trochanteric osteotomy. The interval of follow-up was 3 months for the first postoperative year, and one year thereafter. The Harris hip score (HHS) was used for preoperative and final follow-up clinical evaluations. Hips with a score of ≥90 points were defined as excellent, 80-89 as good, 70-79 as fair, and <70 as poor17). The presence of postoperative thigh pain was also examined. The relationship of thigh pain with radiolucent lines observed on radiographs, cortical hypertrophy, and pedestal formation was investigated. For radiological assessment, subsidence of femoral components, stress shielding, cortical hypertrophy, periprosthetic reactive lines, and osteolysis were examined by dividing the proximal femur into Gruen zones18) on anteroposterior and lateral radiographs around the femoral components. Femoral component fixation was graded as bony stable, fibrous stable, or unstable according to the criteria described by Engh et al.19). For the femoral component, subsidence of >5 mm was classified as loosening according to the method of Callaghan et al.20). A decrease in bone mineral density caused by stress shielding was graded according to the criteria of Engh et al.19), and the degree of stress shielding was observed during follow-up. Cortical hypertrophy was defined as an increase in the diameter of the cortex measured at the point of maximum hypertrophy. A reactive line was defined as a parallel radiolucent line adjacent to the prosthesis.
Revision of the femoral component was defined as the failure of survival, and the 95% confidence interval for the survival rate was calculated using a Kaplan-Meier survival analysis. All statistical analyses were performed using PASW Statistics version 18.0 (IBM Co., Armonk, NY, USA), and paired t-tests and chi-square tests were conducted as appropriate. P-values <0.05 were considered statistically significant. This study was performed after gaining Institutional Review Board approval from our hospital.
RESULTS
The HHS was improved from an average of 50.5 points preoperatively to an average of 84.2 points at the final follow-up. According to the HHS, 13 hips (12.7%) were graded as having excellent results, 48 (47%) were graded as good, 34 (33.3%) were graded as fair, and 7 (6.8%) were graded as having poor results. At the final follow-up, thigh pain was observed in 12 cases (11.7%) without limiting daily living activities or requiring medication. Thigh pain had no statistical relationship with cortical hypertrophy, radiolucency, or pedestal formation (all P>0.05).
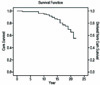
According to radiological evaluations, fixation was graded as bony stable in 98 hips and as fibrous stable in 4 hips. In the fifth postoperative year, radiolucent lines were observed on the postoperative radiographs around the uncoated femoral stem in 69 hips (67%) and at Gruen zones 3, 4, and 5. At the last follow-up, radiolucent lines were observed in only in 13 hips (12%) and were not associated with loosening. Subsidence of the femoral stem occurred in 2 hips during the first postoperative year; however, migration was less than 5 mm and these cases showed bony ingrowth fixation at the last follow-up. Stress shielding of the femur was detected in 67 hips (65%), 64 of which showed first and second degree stress shielding, and 3 that showed third degree stress shielding with bone loss below the lesser trochanter according to Engh's19) criteria. Cortical hypertrophy was observed in 38 hips (37%), primarily in the distal area of the femoral stem. Periprosthetic osteolysis was seen in 72 hips (70%) at Gruen zones 1 and 7, but undetected in the distal area. Postoperative complications included ipsilateral fracture of the femur in 8 hips, dislocation in 7 hips, and infection in 5 hips. All fractures occurred postoperatively. Of the 8 fracture cases, revision operations were conducted in 4 hips, plate fixation in 3 hips, and conservative treatment in one hip. The patient with conservative treatment had loosening during follow-up and underwent a revision operation. Of the 7 cases with dislocation, 3 hips received acetabular cup revision due to recurrent dislocation, and the other 4 hips underwent 6-weeks of conservative treatment using a hip abduction orthosis. Of the 5 infection cases, infection developed within the first 2 postoperative years in one patient, and at an average of 12.1 years in 4 hips. All of these hips received a 2-stage revision. Revision surgery was performed in a total of 24 hips (23.5%) due to femoral osteolysis in 14 hips, infection in 5 hips, and fracture in 5 hips. When revision was regarded as an end point indicative of failure using the Kaplan-Meier curve, the 17.1-year survival rate was 75% (Fig. 1). When loosening was regarded as the end point indicative of failure, the survival rate was 100%.
DISCUSSION
HA-coated femoral components were first introduced for use in THA by Furlong and Osborn21) in 1985 and by Geesink et al.22) in 1986. Since then, a large number of authors have reported short- and mid-term follow-up results of THA with HA-coated anatomical femoral stem5,6,12). Although the clinical outcomes from using HA-coated hip prostheses at mid-term follow-ups were favorable, long-term follow-up results pertaining to acetabular and femoral components showed considerable differences. The HA-coated acetabular cup was shown to have had high loosening and revision rates8,9). Conversely, the HA-coated femoral stem was associated with high survival rates in both mid- and long-term follow-ups11,13). In a previous study, the significant difference in the survival rates of the acetabular cup and femoral stem in THA with HA-coated hip prosthesis was explored23). After osteolysis due to polyethylene wear had been identified as the main cause for the poor outcomes associated with the use of the acetabular cup, investigators attempted to increase its survival rate by using highly cross-linked polyethylene for the acetabular cup surfaces24,25). Favorable clinical and radiological results have been suggested in studies of HA-coated hip prostheses5,6,11,12). Rajaratnam et al.11) proposed a survival rate of 97.4% based on revision surgery in a 17-year follow-up, and a survival rate of 100% based on loosening. In the current study, the HHS was improved to an average of 84.2 points over the 17-year follow-up period, and relatively favorable results were obtained with good outcomes in 60% of subjects. The survival rates were 75% based on revision surgery, and 100% based on loosening. The common cause of revision was proximal femoral osteolysis in most cases, and revision surgery was performed concurrently with acetabular cup revision. Thus, the survival rate of the femoral stem is anticipated to increase with the use of bearings generating less wear debris. However, whether the HA-coated femoral stems are associated with more favorable clinical and radiological results and longer survival rates than those of conventional porous-coated hip prostheses remains uncertain. It also remains unclear whether the HA-coated femoral stem increases survival rates remarkably. In fact, a few previous studies suggested that the HA coating had an insignificant effect on the survival rate of the femoral component26,27).
HA-coated femoral components were found to have strong osteointegration with bone tissue in the early stage3,20), and the initial subsidence of the femoral stem ceased to progress28). In a study by Tonino et al.5) on 222 patients using HA-coated femoral components, 6 femoral stems showed migrations of <5 mm in a minimum follow-up of 2 years, but showed no further migration. In the current study, although subsidence of less than 5 mm was detected within the first postoperative year in 2 hips (1.9%), subsidence was not observed to progress any further during the remainder of the study period. It should be noted that endosteal bone formation was observed around the hip prostheses. Bony ingrowth fixation was achieved without subsidence or loosening in 24 cases using slightly smaller prostheses incompletely fitting within the femoral metaphysis. As 98% of hips showed bony ingrowth fixation at the last follow-up, early bone formation using the HA-coated prosthesis was found to be maintained in the long-term follow-up. However, several concerning radiological findings were detected on final follow-up radiographs.
Rocci et al.29) reported that radiolucent lines were observed at Gruen zones 3, 4, and 5 in 21% of subjects at the sixth postoperative month. According to Tonino et al.5), radiolucent lines were observed in the uncoated distal part of the femoral stem in 12.8% of subjects. Although radiolucent lines were observed at Gruen zones 3, 4, and 5 without an HA coating in 69 hips (67%) in the fifth postoperative year in the current study, they were observed in only 13 hips (12%) at the last follow-up. This is thought to be attributable to radiolucent lines appearing as a response to slight motion in the uncoated distal portion of the prosthesis over-reamed during the early postoperative phase and gradually disappearing with bone formation around the distal part with a grit-blasted surface. Subsidence is anticipated to be avoided by bone formation with a pedestal shape in the distal part of the femoral stem as radiolucent lines disappear when stability of a prosthesis is weakened by extensive osteolysis in the proximal part of prosthesisby reinforcing weakened stability in the proximal part caused by osteolysis.
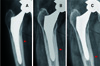
D'Antonio et al.30) reported that cortical hypertrophy increased by 47% and that calcar resorption increased by 63% at Gruen zone 5 in a 6-year follow-up study using HA-coated femoral components. Additionally, Canales et al.31) observed stress shielding in 90% of THA cases during a 10-year follow-up study that used the same femoral stem as was used in the current study. In the current study, stress shielding was observed in 67 hips (65%) postoperatively over an average follow-up of 17.1 years. Stress shielding of grade 1 or 2 was seen in most cases, and grade 3 stress shielding was observed in 3 hips. Cortical hypertrophy was detected in 38 hips and progressed from the distal junction to more distal regions. Several other radiographic findings are thought to be attributable to the unique characteristics of ABG-I femoral stems. The ABG-I stems are designed to reduce the proximal femoral bone resorption due to stress shielding by facilitating osteointegration and expanding pores in the distal part with proximally HA-coated femoral prostheses. As weight loading gradually moved from the proximal to the distal direction with bone formation increasing with follow-up time around the grit-blasted distal region, cortical hypertrophy limited to Gruen zones 2 and 6 expanded to Gruen zones 3 and 5, and proximal bone loss occurred due to stress shielding (Fig. 2).
Oosterbos et al.32) used HA-coated anatomical femoral stems and reported periprosthetic osteolysis in 8% of cases over a 10-year follow-up. Moreover, Bidar et al.13) proposed that the rate of femoral osteolysis was 65.2% at Gruen zone 1 and 18.8% at Gruen zone 7. In the current study, femoral osteolysis was observed in 72 hips (70.5%) and all were found at the proximal portion (Gruen zones 1 and 7). Extensive osteolysis of the proximal femur was the primary cause of revision surgery. Of 24 hips that underwent revision of the femoral components, proximal osteolysis was the cause in 14 cases (Fig. 3). Accounting for a high rate of polyethylene wear in acetabular components used in this study, the osteolysis rate of the proximal region was high compared to that of other prostheses with different coatings. The results of the current study support the conclusion that HA-coating of the femoral prosthesis had an insignificant influence on improving the survival rate of the femoral prosthesis and maintaining the bone quality of the femur over a long-term follow-up period after THA.
A limitation of the current study was that the survival rate of the femoral prosthesis was affected by acetabular cup revision which was performed concurrently with femoral revision in all cases with osteolysis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download