Introduction
The prevalence of osteoporotic fractures is increasing because of a growing elderly population, and sacral insufficiency fractures (SIFs) are no longer a rare type of fracture in the elderly1,2). To date, SIFs have typically been treated conservatively1,2). However, conservative treatment involves long-term bed rest, increase pain medication use, and frequently leads to nonunion and subsequent chronic pain. Recently, in the treatment of SIFs, sacroplasty has been used with a good result3,4). But sacroplasty is not a biological fixation for sacral fracture induced by shear force. Authors performed percutaneous iliosacral screw fixation with cement augmentation for SIFs. It was able to get a secure fixation of the screw in osteoporotic bone and obtained a biological bone union.
Case Report
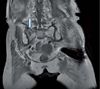
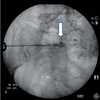
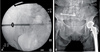
A 75 year-old female patient visited the outpatient department with right buttock pain. For the previous month, she had experienced dull pain in her right buttock during weight bearing when walking. She had undergone hemiarthroplasty for femoral neck fracture 3 years ago and was taking bisphophonate (Fosamax®, MSD) for severe osteoporosis with -3.5 T-score of lumbar spine. No fracture was found on plain radiography (Fig. 1). Radiotracer uptake in an H-pattern was seen on the posterior planar scintigraphic image of a Tc-99 m medronate methylene diphosphonate (MDP) bone scan (Fig. 2). On coronal T1-weighted MR images, there was low-signal intensity edema and a hypointense fracture line (Fig. 3). We decided to perform surgical treatment for symptomatic right sacral fracture to relieve the pain and mobilize the patient out of bed as soon as possible. It was not necessary to fix the left sacral fracture because patient did not feel any pain while on daily activities. Percutaneous iliosacral scew fixation using a 7.3 mm cannulated, 16 mm thread, AO sacral screw was performed under fluoroscopic guidance (Fig. 4A). On follow-up radiography 3 days after operation, the screw had migrated out backward (Fig. 4B). We decided on revision surgery with cement-augmented screw fixation. We had explained this new surgical technique for insufficient sacral fracture to the patient and her family before surgery and have got consent of the patient. She walked without pain 3 days after reoperation. On the follow-up radiographs 6 months after reoperation, there was no sign of screw loosening (Fig. 4C).
Surgical Technique
The patient was placed in the supine position on a radiolucent table. A guide wire, 0.45 mm in diameter, was inserted into the sacrum through the cannula of the loosened screw, and the screw was removed. A biopsy needle was inserted over the guide wire, and the wire was removed. Contrast media was injected through the needle to determine the safety of cement injection (Fig. 5). After confirmation that the cement would not enter the spinal canal or critical areas, 2 cc cement (Osteopal®V, Heraeus Kulzer GmbH, Germany) was injected into the sacrum in the region of screw thread. When the cement had attained a dough-like state, the guide wire was inserted and the biopsy needle was removed. A 6.5 mm cannulated screw was then inserted over the guide wire (Fig. 6).
Discussion
SIFs were first described as a distinct clinical entity by Lourie in 1982, and were regarded as a very rare fracture at that time. However SIFs are no longer uncommon because of the recent growth in the population of the elderly. They commonly affect elderly woman with osteoporosis and are a common cause of diffuse low back pain in the elderly. However, diagnosis of SIFs is often delayed because clinical symptoms are vague and nonspecific. It is also difficult to find out the fractures on plain radiographs. Bone scintigraphy and MR imaging are the most sensitive studies to detect SIFs5,6). CT is less sensitive than bone scintigraphy or MR imaging, but may be helpful to determine if the fracture lines extend into the neural foramina.
Conservative treatment of SIFs has been the standard of care. However not all patients improve with conservative therapy, and prolonged bed rest is associated with significant mobility and mortality in the elderly. Sacroplasty with PMMA cement was introduced as a treatment of SIFs to reduce the disadvantages of conservative therapy and for early return to pre-fracture functional level. Similar to vertebroplasty in the thoracic and lumbar spine, PMMA cement is injected into the fracture site of sacrum under fluoroscopic guidance. Sacroplasty can safely and effectively provide early symptomatic relief3,4). Finite elemental analysis in cadaveric models showed that fracture gap micromotion was diminished significantly after sacroplasty7). However, sacroplasty disrupts normal osseous healing and cement leakage into neural foramina may occur.
Percutaneous iliosacral screw fixation is an established technique for fixation of sacral fracture in biomechanical studies. Iliosacral full threaded lag screw fixation results in superior biological bone healing for sacral fractures caused by shear force. Further, orthopaedic surgeons are familiar with iliosacral screw fixation. However, it is difficult to achieve strong purchase of screw against shear force in osteoporotic bone8,9). We thus introduced a modified iliosacral screw fixation technique with cement augmentation for treatment of SIFs. Our surgical technique has several advantages compared with sacroplasty. First, strong fixation is achieved, which minimizes the shear-force at the fracture site. Park et al10) reported that cement augmentation of the lag screw in compression hip screw (CHS) fixation for intertrochanteric fracture in the elderly with osteoporosis could decrease cut-out of the screw from the femoral head and result in less failure of fixation in osteoporotic bone. Like cement augmentation of lag screw in CHS fixation, cement augmentation of a cannulated screw in osteoporotic bone can achieve a strong purchase. In our case, the patient could walk without pain after surgery and we could not detect any loosening of the screw on follow-up radiographs. Therefore we considered cement augmentation of the screw provided adequate strength of fixation against shear force at the fracture site. Second, biological bone healing is obtained. On follow-up radiographs, we detected union of the fracture of the sacrum 3 months after fixation. We consider that union of the fracture is more biologically compatible than cementation of fracture site. Third, the procedure is simple and safe. There is no need of special equipments with our modified iliosacral screw fixation, and there is no risk of leakage of cement into the neural foramina or spinal canal.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download