Abstract
Total hip arthroplasty (THA) is rarely performed in below-knee amputee patients. To the best of the authors' knowledge, periprosthetic femoral fracture in such patients has not been previously reported. Such devastating complication can occur even with minor trauma. To prevent occurrence of such events, there may be several important factors to be considered in performance of THA surgery in below-knee amputee patients and during the course of rehabilitation. In this report, we describe a case involving a below-knee amputee patient who experienced multiple periprosthetic femoral fractures after THA.
Patients with lower-limb amputations can have various musculoskeletal problems, such as osteoporosis in the amputated limb, and osteoarthritis in either ipsilateral or contralateral limb1). Total hip arthroplasty (THA) in below-knee amputees (BKA) have been described previously2,3). In lower limb amputee patients undergoing THA, there may be important pre- and intraoperative considerations and patients may present a challenging acute postoperative rehabilitation course relative to non-amputee patients4).
The incidence of periprosthetic femual fractures has increased and is still on the rise with growing numbers of THAs5). Even in non amputee patients, the treatment of these fractures is complex and challenging and requires the skills of both trauma surgery and revisional arthroplasty6). Surgical options in displaced periprosthetic femoral fractures include open reduction and internal fixation, an arthroplasty revision procedure, or a combination of two5-10).
In this report, a case of a refracture after treatment of periprosthethic femoral fracture in a patient with BKA who underwent cementless THA for femur neck fracture is presented. Not only there are limited literature about the outcomes and role of THA in lower limb amputee patients2,3), to the author's knowledge, this is the first report of periprosthetic femoral fracture developed after THA in lower limb amputee patient. The patient to be presented was informed that the data concerning the case would be submitted for publication and he consented.
In January, 2010, a 69-year-old Vietnam War veteran presented with right hip pain developed after slip down. He had a background history of below knee amputation for his ipsilateral right leg from severe gunshot injury 40 years ago. Radiographs revealed a displaced subcapital femoral fracture (Fig. 1A). Bone mineral densitometry revealed T-score of -3.2 on the contralateral femoral neck area. The patient was treated with a cementless THA (Summit, DePuy®, U.S.A) using a posterolateral approach with a regional anesthesia. Prior to surgery, the patient was able to ambulate three to four blocks with a cane and negotiated stairs in a non-reciprocating manner (Harris hip score11), of 90). Postoperative radiograph after THA showed satisfactory implant positions (Fig. 1B). On the 14th postoperative day, he was able to progress from walker to crutches.
Two months after his THA operation, the patient visited outpatient clinic complaining of right thigh pain with swelling which occurred after slip down while removing his prosthesis. Radiographs revealed a Vancouver type12). B1 postoperative peroprosthetic femoral fracture (Fig. 2A). It was a spiral fracture with minimal displacement. The previous implanted femoral stem seemed to be in well-fixed state compared to previous follow-up radiographs. Fracture management was done by open reduction with cerclage wiring (Fig. 2B). Four weeks after periprosthetic femoral fracture operation, he was permitted to ambulate using the walker. Walking exercise with parallel-bar was encouraged thereafter for another four weeks.
The patient revisited with painful thigh swelling which was developed about three months after the 2nd operation. The patient claimed that the swelling developed after walking exercise without major traumatic event. Radiographs demonstrated a Vancouver type12). B1 postoperative periprosthetic femoral fracture (Fig. 3). The fracture line was at the distal portion of the femoral stem tip. It was short oblique pattern, with displacement. The femoral stem, however, was still in well-fixed state compared to previous radiographs. Fracture stabilization was performed by use of plate (Broad curved locking compression plate, Synthes®, Switzerland) together with 15 cc of auto cancellous iliac bone graft (Fig. 4). Intraoperatively, previous operated Vancouver type B1 femoral fracture (spiral pattern) site was healed with good stability. Postoperatively, the patient was allowed to ambulate with ischial supported long leg prosthesis using bilateral crutches. Partial weight bearing was permitted after 3 weeks. In supine position, range of motion in his hip and knee joint was encouraged. Fracture was healed at 9 months postoperatively. At latest follow up (2 years after initial THA operation), he presented with Harris hip score of 80.
Periprosthetic femoral fractures after THA in BKA patients may be one of serious complications. While fracture stabilization can be achieved by conventional technique, special care is needed during postoperative rehabilitation period. General rehabilitation protocols which are applied to non-amputee THA patients should not be applied to amputee patients in same manner, since amputee patients have various musculoskeletal problems.
Although there are limited information about THA procedures in patients with lower extremity amputations, THA to treat displaced subcapital femoral fracture has been demonstrated to be effective in BKAs4). Salai et al.2) reported on five BKA patients who were treated with THA for displaced subcapital femoral head fractures and found that THA in these patients may prevent functional deterioration and preserve functional capacity. In this presented case, besides the periprosthetic fractures, the THA procedures including the cementless femoral stem remained stable.
However, the events the patient underwent in this report have demonstrated that lower extremity amputee patients present a challenging postoperative rehabilitation course relative to non-amputee patients. In a previous gait analysis study, Hurley et al.13) found that BKA patients demonstrate a lesser degree of limb symmetry during gait than non-amputees. Long et al.14), founded that there was continued muscle weakness of the operated hip in eighteen cementless THA patients at two years postoperatively and suggested that a prolonged exercise program be employed. From these observations, authors' recommend that the first two months after surgery are critical period with respect to enforcing the standard hip precautions. Special precautions should be alarmed while placing and removing their prosthesis.
Subject specific loading conditions affect stress distribution after THA. Jonkers et al.15) demonstrated that inclusion of subject-specific loading conditions drastically influences the calculated stress distribution, and hence influences the correlation between calculated stress distributions and changes in bone mineral density after THA. They recommended that inclusion of patient-specific loading is essential to obtain accurate input for the analysis of stress distribution after THA15). When treating periprosthethic femoral fractures, the site of the fracture, the stability of the implant, and the condition of surrounding bone stock should be taken into account. Considering these comments in non-amputee limbs, the variety of reported surgical options for Vancouver type B1 postoperative periprosthetic femoral fractures5-10), reflect the lack of consensus for treatment of these injuries. Amputated limbs may be in further specialized situations. The cerclage wiring, although performed widely in periprosthetic fractures after THA in non-amputee patients, may not be suitable in amputated limbs. Rigid fixation using locking plates may be better option.
Figures and Tables
Fig. 1
(A) Pre- and (B) postoperative anteroposterior radiograph. Postoperative radiographs revealed an acceptable implant position.
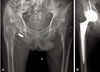
Fig. 2
First periprosthetic fracture. A Vancouver type B1 periprosthethic femoral fracture was stabilized by the multiple cerclage wires. (A) pre- (B) postoperative anteroposterior radiograph.

References
1. Burke MJ, Roman V, Wright V. Bone and joint changes in lower limb amputees. Ann Rheum Dis. 1978. 37:252–254.

2. Salai M, Amit Y, Chechik A, Blankstein A, Dudkiewicz I. Total hip arthroplasty in patients with below-knee amputations. J Arthroplasty. 2000. 15:999–1002.

3. Mak J, Solomon M, Faux S. Ipsilateral total hip arthroplasty in a dysvascular below-knee amputee for advanced hip osteoarthritis: A case report and review of the literature. Prosthet Orthot Int. 2008. 32:155–159.

4. Nejat EJ, Meyer A, Sánchez PM, Schaefer SH, Westrich GH. Total hip arthroplasty and rehabilitation in ambulatory lower extremity amputees--a case series. Iowa Orthop J. 2005. 25:38–41.
5. Xue H, Tu Y, Cai M, Yang A. Locking compression plate and cerclage band for type B1 periprosthetic femoral fractures preliminary results at average 30-month follow-up. J Arthroplasty. 2011. 26:467–471.e1.
6. Buttaro MA, Farfalli G, Paredes Núñez M, Comba F, Piccaluga F. Locking compression plate fixation of Vancouver type-B1 periprosthetic femoral fractures. J Bone Joint Surg Am. 2007. 89:1964–1969.

7. Chandler HP, King D, Limbird R, et al. The use of cortical allograft struts for fixation of fractures associated with well-fixed total joint prostheses. Semin Arthroplasty. 1993. 4:99–107.
8. Haddad FS, Duncan CP, Berry DJ, Lewallen DG, Gross AE, Chandler HP. Periprosthetic femoral fractures around well-fixed implants: use of cortical onlay allografts with or without a plate. J Bone Joint Surg Am. 2002. 84-A:945–950.
9. Howell JR, Masri BA, Garbuz DS, Greidanus NV, Duncan CP. Cable plates and onlay allografts in periprosthetic femoral fractures after hip replacement: laboratory and clinical observations. Instr Course Lect. 2004. 53:99–110.
10. Tsiridis E, Haddad FS, Gie GA. Dall-Miles plates for periprosthetic femoral fractures. A critical review of 16 cases. Injury. 2003. 34:107–110.

11. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969. 51:737–755.

12. Brady OH, Garbuz DS, Masri BA, Duncan CP. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty. 2000. 15:59–62.

13. Hurley GR, McKenney R, Robinson M, Zadravec M, Pierrynowski MR. The role of the contralateral limb in below-knee amputee gait. Prosthet Orthot Int. 1990. 14:33–42.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download