Abstract
A 62-year-old man with an infected periprosthetic femoral fracture, which occurred after a cementless total hip arthroplasty (THA) procedure, was treated utilizing an antibiotic-impregnated cement plate for internal fixation. Open reduction and internal fixation using a cable plate were initially attempted in his case, but a deep infection with methicillin-resistant staphylococcus epidermidis at the fracture site occurred 2 months after the initial cable plate procedure. Using an antibiotic-impregnated cement plate for internal fixation, one month later, the fracture had stabilized. Successful fusion occurred at 12 months after deploying the antibiotic-impregnated cement plate. This technique was useful in this complicated case because it facilitated the goals of eradicating infection, alleviating pain, and improving function.
Periprosthetic femoral fracture is a problematic complication of total hip arthroplasty (THA). Although treatment protocols for periprosthetic femoral fracture have been reported1-4), treatment protocols for periprosthetic fracture with accompanying infection have rarely been published5,6). When these two complications occur together, it becomes more difficult to meet the goals of eradicating infection, alleviating pain, and improving function. The periprosthetic fracture should be stabilized with a technique that does not compromise the goal of eradicating infection. In cases of infected periprosthetic fracture, traditional methods of open reduction and internal fixation with metal plates and screws are not ideal because the metal implants may serve as a sanctuary for bacteria. That bacterial nidus could subsequently infect the reimplanted metals. We present a case in which successful fixation of an infected periprosthetic femoral fracture after THA was achieved using an antibiotic-impregnated cement plate and wiring.
A 62-year-old man with essential hypertension and chronic obstructive pulmonary disease had bilateral avascular necrosis of the femoral head and underwent bilateral cementless THA 18 years prior to presentation. In December 2009, he slipped and fell and subsequently developed painful swelling of the right thigh. The initial diagnosis was a right periprosthetic femoral fracture. On plain radiographs, his right femur showed an oblique fracture distal to the stem tip, which was classified as type C according to the Vancouver classification, without loosening around femoral stem (Fig. 1).
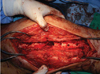
He underwent open reduction and internal fixation for the right periprosthetic fracture using a cable plate (Fig. 2). Two months after surgery, he experienced painful swelling and a sensation of heat in his right thigh. Minimal wire loosening was seen on plain radiographs, and we choose observation because callus formation was observed at the fracture site. After one month, the wire loosening progressed and a varus deformity occurred following the collapse of the medial wall of femoral shaft (Fig. 3). C-reactive protein was elevated from 1.73 to 5.12 mg/dL, and the erythrocyte sedimentation rate was continuously as high as 120 mm/hr during the three months after surgery. We suspected the presence of deep infection around the femoral fracture site. The cable plate was removed, and surgical irrigation and debridement of the fracture site were performed without exposure of the hip implants. Intraoperative examination of frozen-section specimens showed acute inflammation. Because there was a bony defect on the lateral wall of the femoral shaft (3×5 cm) after debridement, proper filling of the defect was needed for fixation (Fig. 4). The medial callus and soft tissue were not dissected in order to provide a hinge for plate fixation, similar to three-point fixation. The entire surgical field was covered with a vinyl sheet for contouring of the defect. The antibiotic-impregnated cement (2 g vancomycin and 1 g cefamandole per 3 packs of cement) was prepared and poured onto to the vinyl sheet before the cement became firm. The plate was mounted and pressure was applied to cause it to sink down under the cement. After curing of the cement, the cement-plate complex was separated from the vinyl sheet (Fig. 5). The antibiotic-impregnated cement-plate complex was placed over the defect site and appropriate stability was achieved with wiring and a medial soft tissue hinge.
Tissue culture revealed methicillin resistant coagulase-negative staphylococcus. Initially, the patient was treated with an intravenous second-generation cephalosporin. After the culture report, he was treated with intravenous vancomycin for 2 weeks and then oral levofloxacin with rifampin for 3 months.
C-reactive protein decreased from 1.59 mg/dL 2 weeks after surgery to 0.5 mg/dL 3 months after surgery. The erythrocyte sedimentation rate also decreased from 84 to 77 mm/hr during the same period. Twelve months after surgery, radiologic bone union was seen on follow-up x-rays (Fig. 6). The patient was able to walk without any support and was pain free.
Periprosthetic femoral fracture is a problematic complication of THA. With a substantial increase in the number of THAs being performed and the growing number of patients with THA who are immobile for longer periods, the prevalence of periprosthetic fracture is on the rise1). The incidence of periprosthetic fracture, although variable, is reported to be approximately 1%5,6). But there are few reports about cases of periprosthetic fracture accompanied by simultaneous infection7,8). Although the etiology of the infection in the present case is unknown, several contributory factors have been described, including advanced age, compromised nutritional status, secondary cerebral vascular accident, and the presence of a decubitus ulcer on the fibular head8). The treatment options for periprosthetic fractures with associated infection at the fracture site have not been clearly established and are dependent on the state of the hip implants. When there is associated prosthetic infection or loosening, removal of the acetabular and femoral components with placement of an antibiotic-impregnated cement-coated spacer or Ender nail and 2-stage exchange are required7). In cases of periprosthetic femoral fracture after THA with deep infection without stem loosening, external fixation could also be a good option8). But in this case, the fracture site was too short to insert screws or pins for external fixation; therefore, we decided to use an antibiotic-impregnated cement and plate fixation. The present case demonstrates several benefits over external fixation. First, this method provides stable fixation. In the present study, the femoral fracture was a spiral fracture well distal to the stem tip and was classified as type C according to the Vancouver classification; therefore, plate fixation was more suitable than external fixation. Generally, locked plate, enough to overlap the femoral stem proximally, is preferred to provide fixed angle stability and improved fixation in an osteoporotic shaft fragment. Fixation in the proximal fragment is with multiple screws distal to the stem into the native shaft fragment and in supplemented with cables around the plate in the zone of the femoral prosthesis. However, in this presentation, there was not enough native shaft fragment of proximal fragment to fix a screw and, even at the distal fragment, screw fixation was not a considerable option because of the disuse osteoporosis and bone defect after screw removal. Instead of the screw fixation, proximally 3 and distally 4 cable fixation was performed, which provide appropriate stability achieved with wiring and a medial soft tissue hinge 3-point fixation. Second, this method is more comfortable for patients. External fixation is external, antibiotic-impregnated cement and plate fixation is internal. Third, there was no need for external fixator removal, which makes it more cost-effective. Fourth, early weight bearing leads to callus formation by micromotion of the fracture site. In cases with large bony defects, this method is more suitable because it provides an appropriate cement spacer for filling the defect and for increased stability.
The limitation of this study includes the use of conventional antibiotic-impregnated cement before tissue culture. In principle, susceptible antibiotics should be mixed to the cement in order to eradicate infection. However, in this presentation, without draining sinus or open wound, it was hard to get infected tissue before the surgery.
This technique may be valuable in cases in which deep prosthetic infection is suspected but not confirmed. We achieved initial stability of the fracture and began treating the suspected infection with locally delivered antibiotics.
Although this is a rare situation, when periprosthetic fracture and infection coexist, antibiotic-impregnated cement and plate fixation could be a safe and reliable method for the treatment of an infected periprosthetic femoral fracture.
Figures and Tables
 | Fig. 1Anteroposterior hip radiograph showing the Vancouver type C periprosthetic fracture without component loosening. |
 | Fig. 2Anteroposterior hip radiograph showing open reduction and internal fixation using a cable plate. |
References
1. Parvizi J, Rapuri VR, Purtill JJ, Sharkey PF, Rothman RH, Hozack WJ. Treatment protocol for proximal femoral periprosthetic fractures. J Bone Joint Surg Am. 2004. 86-A:Suppl 2. 8–16.

2. Singh JR, Greenberg JS, Colavita P. Atypical clinical presentation of periprosthetic femur fracture after revision total hip arthroplasty. Am J Phys Med Rehabil. 2010. 89:772–775.

3. Park SK, Kim YG, Kim SY. Treatment of periprosthetic femoral fractures in hip arthroplasty. Clin Orthop Surg. 2011. 3:101–106.

4. Parvizi J, Vegari DN. Periprosthetic proximal femur fractures: current concepts. J Orthop Trauma. 2011. 25:Suppl 2. S77–S81.

5. Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999. 30:183–190.
6. Pike J, Davidson D, Garbuz D, Duncan CP, O'Brien PJ, Masri BA. Principles of treatment for periprosthetic femoral shaft fractures around well-fixed total hip arthroplasty. J Am Acad Orthop Surg. 2009. 17:677–688.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download