Abstract
Purpose
This study is aimed at identifying the effects of telephone counseling as nursing support on distress, anxiety, depression, and adverse events in cancer patients undergoing their first chemotherapy.
Methods
This was a randomized controlled trial (pretest-posttest design). A total of 70 patients who showed 4 or higher distress scores were selected from the screening process. Four patients dropped out; therefore, 66 patients participated in this research. Thirty-two and 34 patients were randomly assigned to the experimental and the control group, respectively. After a preliminary survey, telephone counseling support was given to the experimental group at three time points. The post survey was done before the second cycle of chemotherapy.
Results
Regarding distress, both groups showed a statistically significant decrease in the scores: 3.4 for the experimental group and 1.8 for the control group (p=.002). Furthermore, the experimental group demonstrated a statistically significant decrease relative to the control group. Anxiety and depression showed no statistically significant difference between the two groups.
Figures and Tables
Table 1
Protocol of the Telephone Counseling

Table 2
Homogeneity Test of General, Disease related Characteristics and Dependent Variables between Experimental and Control Group (N=66)
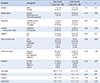
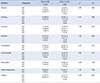
Table 3
Comparison of Change in Distress, Anxiety, and Depression between Experimental and Control Group (N=66)

Table 4
Comparison of Chemotherapy related Adverse Events (N=66)
References
1. Park YS, Han KJ, Ha YS, Song MS, Kim SJ, Chung CW, et al. Effects of telephone counseling on health and service satisfaction after discharge in gynecologic cancer women. J Korean Acad Soc Nurs Educ. 2008; 14:294–304.

2. Yarbro CH, Frogge MH, Goodman M, Groenwald SL. Cancer nursing: principles and practice. 5th ed. Sudbury, MA: Jones and Bartlett;2000.
3. Berger AM, Higginbotham P. Correlates of fatigue during and following adjuvant breast cancer chemotherapy: a pilot study. Oncol Nurs Forum. 2000; 27:1443–1448.
4. Byar KL, Berger AM, Bakken SL, Cetak MA. Impact of adjuvant breast cancer chemotherapy on fatigue, other symptoms, and quality of life. Oncol Nurs Forum. 2006; 33:E18–E26.

5. Paraska K, Bender CM. Cognitive dysfunction following adjuvant chemotherapy for breast cancer: two case studies. Oncol Nurs Forum. 2003; 30:473–478.

6. Chung CW. Longitudinal study on the profiles of symptom distress and functional status in gynecologic cancer patients receiving chemotherapy. Korean J Women Health Nurs. 2006; 12:53–60.

7. Greer S. Psychological intervention. The gap between research and practice. Acta Oncol. 2002; 41:238–243.
8. Grabsch B, Clarke DM, Love A, McKenzie DP, Snyder RD, Bloch S, et al. Psychological morbidity and quality of life in women with advanced breast cancer: a cross-sectional survey. Palliat Support Care. 2006; 4:47–56.

9. Galway K, Black A, Cantwell M, Cardwell CR, Mills M, Donnelly M. Psychosocial interventions to improve quality of life and emotional wellbeing for recently diagnosed cancer patients. Cochrane Database Syst Rev. 2012; 11:CD007064.

10. Chun SY, Shim EJ, Hwang JW, Hahm BJ. Prevalence of distress and its influence on quality of life in breast cancer patients. Korean J Psychosom Med. 2010; 18:72–81.
11. National Comprehensive Cancer Network (US). NCCN clinical practice guidelines in oncology. Distress management, version 1. 2013 [Internet]. Accessed June 3, 2013. Available from: https://www.nccn.org/professionals/physician_gls/pdf/distress.pdf.
12. Knowles G, Sherwood L, Dunlop MG, Dean G, Jodrell D, McLean C, et al. Developing and piloting a nurse-led model of follow-up in the multidisciplinary management of colorectal cancer. Eur J Oncol Nurs. 2007; 11:212–223.

14. Lee HY. Effect of Individualized teaching and telephone counseling on self-care behavior among patients with hematologic cancer [dissertation]. Seoul: Yonsei Univ.;2000.
15. Jang OJ, Woo SH, Park YS. Effects of telephone follow-up on the self-care performance for cancer patients undergoing chemotherapy and role stress of family caregivers. J Korean Acad Fundam Nurs. 2006; 13:50–59.
16. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates;1988.
17. Miller WR, Rollnick S. Ten things that motivational interviewing is not. Behav Cogn Psychother. 2009; 37:129–140.

18. Sarna L, Cooley ME, Brown JK, Williams RD, Chernecky C, Padilla G, et al. Quality of life and health status of dyads of women with lung cancer and family members. Oncol Nurs Forum. 2006; 33:1109–1116.

19. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67:361–370.

20. Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans: a comparison of normal, depressed and anxious groups. J Korean Neuropsychiatr Assoc. 1999; 38:289–296.
21. National Cancer Institute (US). Common terminology criteria for adverse events: v.4.0 [Internet]. Accessed April 15, 2013. Available from: https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_40.
22. Kim MY. Transition of symptoms and quality of life in cancer patients on chemotherapy. J Korean Acad Nurs. 2009; 39:433–445.

23. Choi SE, Park HR, Ban JY. Anxiety in patient undergone hematopoietic stem cell transplantation. J Korean Oncol Nurs. 2006; 6:37–46.
24. Kim CJ, Hur HK, Kang DH, Kim BH. The effects of psychosocial interventions to improve stress and coping in patients with breast cancer. J Korean Acad Nurs. 2006; 36:169–178.

25. Yi M, Kim JH, Park EY, Kim JN, Yu ES. Focus group study on psychosocial distress of cancer patients. J Korean Acad Adult Nurs. 2010; 22:19–30.
26. Suh SR, Lee WK. The effect of psychoeducational intervention for symptom management of home cancer patient. J Korean Oncol Nurs. 2003; 3:56–65.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download