Abstract
Purpose
The purpose of this study was to examine the effect of post-operative exercise on body composition, psychological factors, time to flatus and length of hospital stay in stage 1~3 colorectal cancer patients.
Methods
A total of 35 post surgery patients were recruited and randomly assigned to the exercise or controlled group. Participants in the exercise group exercised twice a day while participants in the control group followed the clinical pathways (CP).
Results
A total of 25 participants completed the trial. Post-operative exercise resulted in a clinically meaningful, but statistically insignificant reduction in body weight (Exercise: -1.10±1.63 kg vs. CP: -0.63±1.16 kg; p=.111), fat mass (Exercise: -1.43±0.95 kg vs. CP: 0.64±4.29 kg; p=.100). When participants' body composition were compared to their baseline values at the baseline, only the exercise group experienced a significant reduction in body weight, body mass index (BMI) and fat mass. In addition, post-operative exercise significantly improved health related quality of life (Exercise: 2.27±2.08 vs CP: -12.82±22.47; p=.008). However, there was no difference in time to flatus and the length of hospital stay between groups.
Figures and Tables
Table 1
Characteristics of the Sample (N=25)
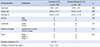
Table 2
Comparison of Physical Factors between Exercise Group and Control Group (N=25)
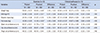
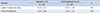
Table 3
Comparison of Psychological Factors between Exercise Group and Control Group (N=25)

References
2. Jung KW, Won YJ, Oh CM, Kong HJ, Cho H, Lee JK, et al. Prediction of cancer incidence and mortality in Korea, 2016. Cancer Res Treat. 2016; 48:451–457.

3. Jung HJ, Choi M, Kim SS, Kim NK, Lee KY. The effects and variances of the critical pathway of laparoscopic colon resection in colon cancer patients. Asian Oncol Nurs. 2012; 12:204–212.

4. Brown SR, Mathew R, Keding A, Marshall HC, Brown JM, Jayne DG. The impact of postoperative complications on long-term quality of life after curative colorectal cancer surgery. Ann Surg. 2014; 259:916–923.

5. Lawrence DP, Kupelnick B, Miller K, Devine D, Lau J. Evidence report on the occurrence, assessment, and treatment of fatigue in cancer patients. J Natl Cancer Inst Monogr. 2004; 40–50.

6. Li C, Carli F, Lee L, Charlebois P, Stein B, Liberman AS, et al. Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc. 2013; 27:1072–1082.

7. Lockefeer JP, De Vries J. What is the relationship between trait anxiety and depressive symptoms, fatigue, and low sleep quality following breast cancer surgery? Psychooncology. 2013; 22:1127–1133.

8. Biagi JJ, Raphael MJ, Mackillop WJ, Kong W, King WD, Booth CM. Association between time to initiation of adjuvant chemotherapy and survival in colorectal cancer: a systematic review and meta-analysis. JAMA. 2011; 305:2335–2342.

9. Esteban F, Cerdan FJ, Garcia-Alonso M, Sanz-Lopez R, Arroyo A, Ramirez JM, et al. A multicentre comparison of a fast track or conventional postoperative protocol following laparoscopic or open elective surgery for colorectal cancer surgery. Colorectal Dis. 2014; 16:134–140.

10. Khan SA, Ullah S, Ahmed J, Wilson TR, McNaught C, Hartley J, et al. Influence of enhanced recovery after surgery pathways and laparoscopic surgery on health-related quality of life. Colorectal Dis. 2013; 15:900–907.

11. Wang Q, Suo J, Jiang J, Wang C, Zhao YQ, Cao X. Effectiveness of fast-track rehabilitation vs conventional care in laparoscopic colorectal resection for elderly patients: a randomized trial. Colorectal Dis. 2012; 14:1009–1013.

12. Ahn KY, Hur H, Kim DH, Min J, Jeong DH, Chu SH, et al. The effects of inpatient exercise therapy on the length of hospital stay in stages I-III colon cancer patients: randomized controlled trial. Int J Colorectal Dis. 2013; 28:643–651.
13. Hung SL, Lin YH, Yang HY, Kao CC, Tung HY, Wei LH. Pelvic floor muscle exercise for fecal incontinence quality of life after coloanal anastomosis. J Clin Nurs. 2016; 25:2658–2668.

14. Yun YH, Park YS, Lee ES, Bang SM, Heo DS, Park SY, et al. Validation of the Korean version of the EORTC QLQ-C30. Qual Life Res. 2004; 13:863–868.

15. Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans: a comparison of normal, depressed and anxious groups. J Korean Neuropsychiatr Assoc. 1999; 38:289–296.
16. Kim GD, Kim KH. Symptom cluster and quality of life in patients with breast cancer undergoing chemotherapy. Korean J Adult Nurs. 2011; 23:434–445.
17. Min JH. Developing of evidence based exercise program for postoperative colorectal cancer patients: pilot study [dissertation]. Seoul: Yonsei Univ.;2014.
18. Brown JC, Huedo-Medina TB, Pescatello LS, Pescatello SM, Ferrer RA, Johnson BT. Efficacy of exercise interventions in modulating cancer-related fatigue among adult cancer survivors: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2011; 20:123–133.

19. Vashistha V, Singh B, Kaur S, Prokop LJ, Kaushik D. The effects of exercise on fatigue, quality of life, and psychological function for men with prostate cancer: systematic review and meta-analyses. Eur Urol Focus. 2016; 2:284–295.

20. Buffart LM, De Backer IC, Schep G, Vreugdenhil A, Brug J, Chinapaw MJ. Fatigue mediates the relationship between physical fitness and quality of life in cancer survivors. J Sci Med Sport. 2013; 16:99–104.

21. Kim SH, Son BH, Hwang SY, Han W, Yang JH, Lee S, et al. Fatigue and depression in disease-free breast cancer survivors: prevalence, correlates, and association with quality of life. J Pain Symptom Manage. 2008; 35:644–655.

22. Travier N, Guillamo E, Oviedo GR, Valls J, Buckland G, Fonseca-Nunes A, et al. Is quality of life related to cardiorespiratory fitness in overweight and obese breast cancer survivors? Women Health. 2015; 55:505–524.

23. Mock V, Pickett M, Ropka ME, Muscari Lin E, Stewart KJ, Rhodes VA, et al. Fatigue and quality of life outcomes of exercise during cancer treatment. Cancer Pract. 2001; 9:119–127.

24. Ahn KY. The effect of colorectal cancer exercise program in colorectal cancer patient after surgery [dissertation]. Seoul: Yonsei Univ.;2011.
25. Ravussin E, Lillioja S, Knowler WC, Christin L, Freymond D, Abbott WG, et al. Reduced rate of energy expenditure as a risk factor for bodyweight gain. N Engl J Med. 1988; 318:467–472.

26. Stiegler P, Cunliffe A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med. 2006; 36:239–262.

27. Kroenke CH, Neugebauer R, Meyerhardt J, Prado CM, Weltzien E, Kwan ML, et al. Analysis of body mass index and mortality in patients with colorectal cancer using causal diagrams. JAMA Oncol. 2016; 2:1137–1145.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download