Abstract
Purpose
This is the methodological study to develop the cognitive function scale for breast cancer patients.
Methods
Study was consisted with 1st and 2nd items developing and testify for reliability and validity of them. 94 breast cancer patients in 2 university hospitals and 1 general hospitals responded to a questionnaire that assessed cognitive function scale. Collected data were analysed using the program SPSS/PC Win 21.0. Structural validity was determined factor analysis and convergent validity. This method yielded Cronbach's α value as an internal consistency for the reliability.
Results
Factor analysis resulted in six factors and 24 items accounted for 76.31% of the variance. Cronbach's α of scale developed was high as a .95.
Conclusion
The developed cognitive function scale in breast cancer patients scale has reliability and validity as linear analogue scale witch quantitatively measure the subjectivity. Over these results, providing the way on an assessment in cognitive function in effect for breast cancer patients, it is supposed to contribute the development of nursing knowledge about the cognitive function in breast cancer patients.
Figures and Tables
Table 1
Experiences of Cognitive Function Disorder after Chemotherapy in Breast Cancer

Table 2
Characteristics of Subjects (N=94)

Table 3
Inter-subscale Correlations and Reliability Coefficients of Each Scale
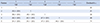
Table 4
Reliability of Each Subscale

Table 5
Factor Loadings and Accumulative Variance in the Items (N=94)

TVE= Total variance explained; Criteria of value of loading>.50.
aKaiser-Meyer-Olkin (KMO)= .86, Bartlette's test of sphericity= 4,616.31, p<.001; bKaiser-Meyer-Olkin (KMO)= .86, Bartlette's test of sphericity= 2,418.54, p<.001; cKaiser-Meyer-Olkin (KMO)= .87, Bartlette's test of sphericity= 1,966.96, p<.001; dKaiser-Meyer-Olkin (KMO)= .86, Bartlette's test of sphericity= 1,905.17, p<.001.
References
1. Statistics Korea. Cancer registration statistics: 24 cancers [Internet]. Accessed January 20, 2017. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=DT_117N_A00023.
2. Lee JR, Oh PJ. Cognitive decline and quality of life among patients with breast cancer undergoing chemotherapy: the mediating effect of health promotion behavior. Korean J Adult Nurs. 2016; 28:202–212.

3. Jansen CE, Cooper BA, Dodd MJ, Miaskowski CA. A prospective longitudinal study of chemotherapy-induced cognitive changes in breast cancer patients. Support Care Cancer. 2011; 19:1647–1656.

4. Collins B, Mackenzie J, Kyeremanteng C. Study of the cognitive effects of chemotherapy: considerations in selection of a control group. J Clin Exp Neuropsychol. 2013; 35:435–444.

5. Tager FA, McKinley PS, Schnabel FR, El-Tamer M, Cheung YK, Fang Y, et al. The cognitive effects of chemotherapy in post-menopausal breast cancer patients: a controlled longitudinal study. Breast Cancer Res Treat. 2010; 123:25–34.

6. Shockney LD. Breast cancer survivorship care: a resource for nurses. Sudbury, MA: Jones and Bartlett;2011.
7. Quesnel C, Savard J, Ivers H. Cognitive impairments associated with breast cancer treatments: results from a longitudinal study. Breast Cancer Res Treat. 2009; 116:113–123.

8. Wefel JS, Saleeba AK, Buzdar AU, Meyers CA. Acute and late onset cognitive dysfunction associated with chemotherapy in women with breast cancer. Cancer. 2010; 116:3348–3356.

9. Brezden CB, Phillips KA, Abdolell M, Bunston T, Tannock IF. Cognitive function in breast cancer patients receiving adjuvant chemotherapy. J Clin Oncol. 2000; 18:2695–2701.

10. Bender CM. Chemotherapy may have small to moderate negative effects on cognitive functioning. Cancer Treat Rev. 2006; 32:316–319.

11. Calvio L, Peugeot M, Bruns GL, Todd BL, Feuerstein M. Measures of cognitive function and work in occupationally active breast cancer survivors. J Occup Environ Med. 2010; 52:219–227.

12. Oh PJ, Kim JH. Chemotherapy related cognitive impairment and quality of life in people with colon cancer: the mediating effect of psychological distress. J Korean Acad Nurs. 2016; 46:19–28.

13. Vardy J, Wong K, Yi QL, Park A, Maruff P, Wagner L, et al. Assessing cognitive function in cancer patients. Support Care Cancer. 2006; 14:1111–1118.

14. Yamada TH, Denburg NL, Beglinger LJ, Schultz SK. Neuropsychological outcomes of older breast cancer survivors: cognitive features ten or more years after chemotherapy. J Neuropsychiatry Clin Neurosci. 2010; 22:48–54.

15. Lejbak L, Vrbancic M, Crossley M. Endocrine therapy is associated with low performance on some estrogen-sensitive cognitive tasks in postmenopausal women with breast cancer. J Clin Exp Neuropsychol. 2010; 32:836–846.

16. Debess J, Riis JØ, Engebjerg MC, Ewertz M. Cognitive function after adjuvant treatment for early breast cancer: a population-based longitudinal study. Breast Cancer Res Treat. 2010; 121:91–100.

17. Freeman JR, Broshek DK. Assessing cognitive dysfunction in breast cancer: what are the tools? Clin Breast Cancer. 2002; 3:Suppl 3. S91–S99.

18. Jansen CE, Miaskowski CA, Dodd MJ, Dowling GA. A meta-analysis of the sensitivity of various neuropsychological tests used to detect chemotherapy-induced cognitive impairment in patients with breast cancer. Oncol Nurs Forum. 2007; 34:997–1005.

19. Cimprich B, So H, Ronis DL, Trask C. Pre-treatment factors related to cognitive functioning in women newly diagnosed with breast cancer. Psychooncology. 2005; 14:70–78.

20. Shilling V, Jenkins V. Self-reported cognitive problems in women receiving adjuvant therapy for breast cancer. Eur J Oncol Nurs. 2007; 11:6–15.

21. Wefel JS, Lenzi R, Theriault RL, Davis RN, Meyers CA. The cognitive sequelae of standard-dose adjuvant chemotherapy in women with breast carcinoma: results of a prospective, randomized, longitudinal trial. Cancer. 2004; 100:2292–2299.

22. Lee EO, Lim NY, Park HA, Lee IS, Kim JI, Bae JL, et al. Nursing research and statistical analysis. Paju: Soomoonsa;2009.
23. Harvan JR, Cotter V. An evaluation of dementia screening in the primary care setting. J Am Acad Nurse Pract. 2006; 18:351–360.

24. Shulman KI. Clock-drawing: is it the ideal cognitive screening test? Int J Geriatr Psychiatry. 2000; 15:548–561.

25. Chung BY. Development and application of cognitive function enhancement program for breast cancer patients receiving chemotherapy. Seoul: Ministry of Education, Science and Technology;2013.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download