Abstract
Purpose
The purpose of this study was to evaluate the effect of diet intervention in breast cancer patients through meta-analysis.
Methods
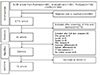
For the study purpose, 18 studies were selected using PubMed, ScienceDirect, ProQuest and CINAHL. Meta-analysis was performed using a random effects model, and the effect size on outcome variables in breast cancer were calculated.
Results
The effect size for body mass index, body weight, energy intake from fat (%), and energy intake of diet intervention was −0.75 (95% CI:−1.22~−0.27), −0.93 (95% CI:−1.58~−0.28), −0.82 (95% CI:−1.11~−0.52), and −1.10 (95% CI:−1.85~−0.34). For heterogeneity, moderator analysis was performed using intervention type and intervention duration. As a result of the moderator analysis, BMI, body weight, energy intake from fat (%), and energy intake were not statistically significant on intervention type and intervention duration. But, only BMI had a significant difference on intervention duration (p=.013).
Figures and Tables
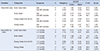
Table 1
General Characteristics of Studies Included in Meta-analysis

Exp.= Experimental group; Cont.= Control group; T= Total; RCT= Randomized Controlled Trial; NRCT= Non-Randomized Controlled Trial; BC= Breast cance; PC= Prostatic cancer; BMI= Body mass index; TG= Plasma triglycerides; Chol= Plasma cholesterol; HDL= HDL cholesterol; LDL= LDL cholesterol; QOL= Quality of life; PA= Physical activity; CA= Calcium-rich diet; EX= Exercise; FVLF= High fruit and vegetable and low-fat diet; WW= Weight Watchers; IC= Individualized counseling.
Table 2
Risk of Bias for RCT and NRCT

Table 3
Subgroup Analysis by Intervention Type and Intervention Duration
References
1. National Cancer Center (KR). Cancer facts & figures 2016 in the Republic of Korea [Internet]. Accessed January 20, 2017. Available from: http://www.cancer.go.kr/mbs/cancer/jsp/album/gallery.jsp?boardType=02&boardId=31817&listType=02&mcategoryId=&id=cancer_050207000000&addCancerTitle.
2. Christifano DN, Fazzino TL, Sullivan DK, Befort CA. Diet quality of breast cancer survivors after a six-month weight management intervention: improvements and association with weight loss. Nutr Cancer. 2016; 68:1301–1308.

3. Kroenke CH, Kwan ML, Sweeney C, Castillo A, Caan BJ. High- and low-fat dairy intake, recurrence, and mortality after breast cancer diagnosis. J Natl Cancer Inst. 2013; 105:616–623.

4. Rock CL, Demark-Wahnefried W. Nutrition and survival after the diagnosis of breast cancer: a review of the evidence. J Clin Oncol. 2002; 20:3302–3316.

5. Beasley JM, Newcomb PA, Trentham-Dietz A, Hampton JM, Bersch AJ, Passarelli MN, et al. Post-diagnosis dietary factors and survival after invasive breast cancer. Breast Cancer Res Treat. 2011; 128:229–236.

6. Ewertz M, Jensen MB, Gunnarsdóttir KÁ, Højris I, Jakobsen EH, Nielsen D, et al. Effect of obesity on prognosis after early-stage breast cancer. J Clin Oncol. 2011; 29:25–31.

7. Chan DS, Vieira AR, Aune D, Bandera EV, Greenwood DC, McTiernan A, et al. Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol. 2014; 25:1901–1914.

8. Campbell KL, Van Patten CL, Neil SE, Kirkham AA, Gotay CC, Gelmon KA, et al. Feasibility of a lifestyle intervention on body weight and serum biomarkers in breast cancer survivors with overweight and obesity. J Acad Nutr Diet. 2012; 112:559–567.

9. Kellen E, Vansant G, Christiaens MR, Neven P, Van Limbergen E. Lifestyle changes and breast cancer prognosis: a review. Breast Cancer Res Treat. 2009; 114:13–22.

10. Cho SW, Kim JH, Lee SM, Lee SM, Choi EJ, Jeong J, et al. Effect of 8-week nutrition counseling to increase phytochemical rich fruit and vegetable consumption in Korean breast cancer patients: a randomized controlled trial. Clin Nutr Res. 2014; 3:39–47.

11. Harrigan M, Cartmel B, Loftfield E, Sanft T, Chagpar AB, Zhou Y, et al. Randomized trial comparing telephone versus in-person weight loss counseling on body composition and circulating biomarkers in women treated for breast cancer: the lifestyle, exercise, and nutrition (LEAN) study. J Clin Oncol. 2016; 34:669–676.

12. Rock CL, Flatt SW, Byers TE, Colditz GA, Demark-Wahnefried W, Ganz PA, et al. Results of the exercise and nutrition to enhance recovery and good health for you (ENERGY) trial: a behavioral weight loss intervention in overweight or obese breast cancer survivors. J Clin Oncol. 2015; 33:3169–3176.

13. Sheppard VB, Hicks J, Makambi K, Hurtado-de-Mendoza A, Demark-Wahnefried W, Adams-Campbell L. The feasibility and acceptability of a diet and exercise trial in overweight and obese black breast cancer survivors: the Stepping STONE study. Contemp Clin Trials. 2016; 46:106–113.

14. Shaw C, Mortimer P, Judd PA. Randomized controlled trial comparing a low-fat diet with a weight-reduction diet in breast cancer-related lymphedema. Cancer. 2007; 109:1949–1956.

15. Hoy MK, Winters BL, Chlebowski RT, Papoutsakis C, Shapiro A, Lubin MP, et al. Implementing a low-fat eating plan in the women's intervention nutrition study. J Am Diet Assoc. 2009; 109:688–696.

16. Mefferd K, Nichols JF, Pakiz B, Rock CL. A cognitive behavioral therapy intervention to promote weight loss improves body composition and blood lipid profiles among overweight breast cancer survivors. Breast Cancer Res Treat. 2007; 104:145–152.

17. Hauner D, Janni W, Rack B, Hauner H. The effect of overweight and nutrition on prognosis in breast cancer. Dtsch Arztebl Int. 2011; 108:795–801.

18. Playdon MC, Bracken MB, Sanft TB, Ligibel JA, Harrigan M, Irwin ML. Weight gain after breast cancer diagnosis and all-cause mortality: systematic review and meta-analysis. J Natl Cancer Inst. 2015; 107:djv275.

19. Spark LC, Reeves MM, Fjeldsoe BS, Eakin EG. Physical activity and/or dietary interventions in breast cancer survivors: a systematic review of the maintenance of outcomes. J Cancer Surviv. 2013; 7:74–82.

20. Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions: version 5.1.0 [Internet]. Accessed June 6, 2016. Available from: http://handbook.cochrane.org.
21. PRISMA. Preferred reporting items for systematic reviews and metaanalyses (PRISMA) [Internet]. Accessed June 6, 2016. Available from: http://www.prismastatement.org.
22. Kim SY, Park JE, Seo HJ, Seo HS, Son HJ, Shin CM, et al. NECA's guidance for undertaking systematic reviews and meta-analyses for intervention. Seoul: National Evidence-based Healthcare Collaborating Agency;2011.
23. Hedges LV, Olkin I. Statistical methods for meta-analysis. San Diego, CA: Academic Press;1985.
24. Littell JH, Corcoran J, Pillai V. Systematic reviews and meta-analysis. New York, NY: Oxford University Press;2008.
25. Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to meta-analysis. West Sussex: John Wiley & Sons;2009.
26. Demark-Wahnefried W, Case LD, Blackwell K, Marcom PK, Kraus W, Aziz N, et al. Results of a diet/exercise feasibility trial to prevent adverse body composition change in breast cancer patients on adjuvant chemotherapy. Clin Breast Cancer. 2008; 8:70–79.

References
Reference in Meta-analysis
Reference in Meta-analysis
1. Reference in Meta-analysis. Christy SM, Mosher CE, Sloane R, Snyder DC, Lobach DF, Demark-Wahnefried W. Long-term dietary outcomes of the FRESH START intervention for breast and prostate cancer survivors. J Am Diet Assoc. 2011; 111:1844–1851.

2. Reference in Meta-analysis. Demark-Wahnefried W, Clipp EC, Morey MC, Pieper CF, Sloane R, Snyder DC, et al. Lifestyle intervention development study to improve physical function in older adults with cancer: outcomes from Project LEAD. J Clin Oncol. 2006; 24:3465–3473.

3. Reference in Meta-analysis. Demark-Wahnefried W, Clipp EC, Lipkus IM, Lobach D, Snyder DC, Sloane R, et al. Main outcomes of the FRESH START trial: a sequentially tailored, diet and exercise mailed print intervention among breast and prostate cancer survivors. J Clin Oncol. 2007; 25:2709–2718.

4. Reference in Meta-analysis. Demark-Wahnefried W, Case LD, Blackwell K, Marcom PK, Kraus W, Aziz N, et al. Results of a diet/exercise feasibility trial to prevent adverse body composition change in breast cancer patients on adjuvant chemotherapy. Clin Breast Cancer. 2008; 8:70–79.

5. Reference in Meta-analysis. Demark-Wahnefried W, Jones LW, Snyder DC, Sloane RJ, Kimmick GG, Hughes DC, et al. Daughters and Mothers Against Breast Cancer (DAMES): main outcomes of a randomized controlled trial of weight loss in overweight mothers with breast cancer and their overweight daughters. Cancer. 2014; 120:2522–2534.

6. Reference in Meta-analysis. Djuric Z, DiLaura NM, Jenkins I, Darga L, Jen CK, Mood D, et al. Combining weight-loss counseling with the weight watchers plan for obese breast cancer survivors. Obes Res. 2002; 10:657–665.

7. Reference in Meta-analysis. Goodwin PJ, Segal RJ, Vallis M, Ligibel JA, Pond GR, Robidoux A, et al. Randomized trial of a telephone-based weight loss intervention in postmenopausal women with breast cancer receiving letrozole: the LISA trial. J Clin Oncol. 2014; 32:2231–2239.

8. Reference in Meta-analysis. Greenlee H, Gaffney AO, Aycinena AC, Koch P, Contento I, Karmally W, et al. ¡Cocinar para su salud!: randomized controlled trial of a culturally based dietary intervention among hispanic breast cancer survivors. J Acad Nutr Diet. 2015; 115:S42–S56.

9. Reference in Meta-analysis. Harrigan M, Cartmel B, Loftfield E, Sanft T, Chagpar AB, Zhou Y, et al. Randomized trial comparing telephone versus in-person weight loss counseling on body composition and circulating biomarkers in women treated for breast cancer: The lifestyle, exercise, and nutrition (LEAN) study. J Clin Oncol. 2016; 34:669–676.

10. Reference in Meta-analysis. Hebert JR, Ebbeling CB, Olendzki BC, Hurley TG, Ma Y, Saal N, et al. Change in women's diet and body mass following intensive intervention for early-stage breast cancer. J Am Diet Assoc. 2001; 101:421–431.

11. Reference in Meta-analysis. Hoy MK, Winters BL, Chlebowski RT, Papoutsakis C, Shapiro A, Lubin MP, et al. Implementing a low-fat eating plan in the Women's Intervention Nutrition Study. J Am Diet Assoc. 2009; 109:688–696.

12. Reference in Meta-analysis. Mefferd K, Nichols JF, Pakiz B, Rock CL. A cognitive behavioral therapy intervention to promote weight loss improves body composition and blood lipid profiles among overweight breast cancer survivors. Breast Cancer Res Treat. 2007; 104:145–152.

13. Reference in Meta-analysis. Pakiz B, Flatt SW, Bardwell WA, Rock CL, Mills PJ. Effects of a weight loss intervention on body mass, fitness, and inflammatory biomarkers in overweight or obese breast cancer survivors. Int J Behav Med. 2011; 18:333–341.

14. Reference in Meta-analysis. Schiavon CC, Vieira FG, Ceccatto V, de Liz S, Cardoso AL, Sabel C, et al. Nutrition education intervention for women with breast cancer: effect on nutritional factors and oxidative stress. J Nutr Educ Behav. 2015; 47:2–9.

15. Reference in Meta-analysis. Shaw C, Mortimer P, Judd PA. A randomized controlled trial of weight reduction as a treatment for breast cancer-related lymphedema. Cancer. 2007; 110:1868–1874.

16. Reference in Meta-analysis. Shaw C, Mortimer P, Judd PA. Randomized controlled trial comparing a low-fat diet with a weight-reduction diet in breast cancer-related lymphedema. Cancer. 2007; 109:1949–1956.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download