Abstract
Purpose
The objective of this study was to analyze effect size of the intervention studies for posttraumatic growth in patients with cancer.
Methods
A total of 871 studies published between 2000 and 2014 were identified by searching Ovid-Medline, CINAHL, PubMed, Scopus, PsycARTICLES, Cochrane library, RISS, and KISS. 15 studies were selected for inclusion in the meta-analysis. Data were analyzed using the Comprehensive Meta-Analysis (CMA) Ver. 3 program and the effect sizes were shown using Hedges's g score.
Results
Intervention studies included 5 studies on Cognitive Behavioral Stress Management (CBSM), 4 studies for Mindfulness-Based Stress Reduction (MBSR), 2 studies for couple-based intervention, and 1 study each for health coaching, building resilience, yoga and painting intervention. The overall controlled effect size was 0.335 (95% CI=0.231, 0.438), using a fixed effects model. The most effective intervention was the couple-based intervention (0.368, 95% CI=-0.146, 0.883), followed by MBSR (0.340, 95% CI=0.172, 0.508) and CBSM (0.314, 95% CI=0.139, 0.490).
Conclusion
Cancer is one of the most significant traumatic events that affect patients' lives, a few cancer patients have been known to have posttraumatic growth. Therefore it is necessary to consider nursing interventions to increase posttraumatic growth for cancer patients such as couple-based intervention, MBSR and CBSM.
Figures and Tables
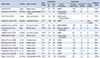
Table 1
General Characteristics of Included Study (N=15)

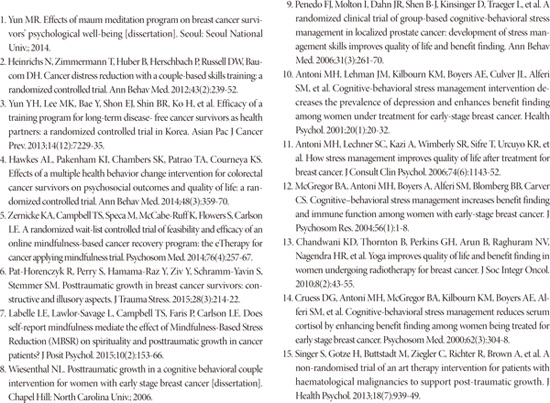
Table 2
Characteristics of PTG Intervention for Cancer Patients (N=15)
References
1. National Cancer Information Center. Accessed December 23, 2015. http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_040101000000.
2. Lee IJ. The effects of stress on quality of life in cancer patients: focusing on the moderating effects of post-traumatic growth. Health Soc Welf Rev. 2012; 32(3):522–557.

3. Ohnishi H. Mental distress in cancer patients. Masui. 2011; 60(9):1024–1031.
4. Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J Trauma Stress. 1996; 9(3):455–471.

5. Shand LK, Brooker JE, Burney S, Fletcher J, Ricciardelli LA. Symptoms of posttraumatic stress in Australian women with ovarian cancer. Psychooncology. 2015; 24(2):190–196.

6. Yang SK, Kim ES. The relationship among the coping style, social support, and post-traumatic stress disorder in breast cancer patients treated with chemotherapy. Korean J Hosp Palliat Care. 2015; 18(1):35–41.

7. Jim HS, Jacobsen PB. Posttraumatic stress and posttraumatic growth in cancer survivorship: a review. Cancer Journal. 2008; 14(6):414–419.

8. Jang SH, Lee HR, Yeu HN, Choi SO. The effects of posttraumatic growth and meaning in life on health promotion behavior in cancer patients. Asian Oncol Nurs. 2014; 14(2):100–108.

9. Jeon SW, Han CS, Choi JH, Pae CU, Chae JH, Ko YH, et al. Postraumatic growth and resilience: assessment and clinical implications. J Korean Neuropsychiatr Assoc. 2015; 54(1):32–39.

10. Kim JK, Jang HA. Research on posttraumatic growth in Korea: Trends and future directions. Cognitive Behav Ther Korea. 2014; 14(2):239–265.
11. Lee IJ. A systematic review of posttraumatic growth in cancer. Soc Work Pract Res. 2009; 6:81–113.
12. Choi SM, Kim YJ, Kwon JH. Effects of cognitive and behavioral coping and social supports on post traumatic growth : depending on PTSD symptom severity. Cognitive Behav Ther Korea. 2013; 13(2):307–328.
13. Carlson L, Speca M, Segal Z. Mindfulness-based cancer recovery: a step by step MBSR approach to help you cope with treatment and reclaim your life. Oakville, CA: New Harbinger;2010.
14. Casellas-Grau A, Font A, Vives J. Positive psychology interventions in breast cancer; a systematic review. PsychoOncology. 2014; 23:9–19.

15. Lee YJ, Chung NW. A review of posttraumatic growth researches: focused on relation with adjustment and clinical application. Korean J Health Psychol. 2008; 13(1):1–23.
16. Roepke AM. Psycholsocial intervention and posttraumatic growth: a meta-analysis. J Consult Clin Psychol. 2015; 83(1):129–142.
17. Kim SY, Park JE, Seo HJ, Lee YJ, Son HJ, Jang BH, et al. NECA's guidance for undertaking systematic reviews and meta-analyses for intervention. Seoul: National Evidence-based Health care Clooaborating Agency;2011.
18. Prati G, Pietrantoni L. Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: a meta-analysis. J Loss Trauma. 2009; 14:364–388.

19. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. NJ: Lawrence Earlbaum Associates;1988.
20. Fann JR, Thomasn-Rich AM, Katon WJ, Cowley D, Pepping M, Mcgregor BA, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry. 2008; 30:112–126.

21. Yi MS, Cha JE. Changes of self-efficacy, depression, and posttraumatic growth in survivors with breast cancer participating breast cancer prevention volunteering. J Korea Contents Assoc. 2014; 14(4):256–266.

22. Davidson K, Schwatz AR, Sheffield D, Moord RS, Lepore SJ, Gerin W. Expressive writing and blood pressure. In : Lepore SJ, Smyth J, editors. The writing cure. Washington DC: American Psychological Association;2003. p. 17–30.
23. Knaevelsrud C, Liedl A, Maercker A. Posttraumatic growth, optimism and openness as outcomes of a cognitive-behavioural intervention for posttraumatic stress reaction. J Health Psychol. 2010; 15(7):1030–1038.

24. Kolokotroni P, Anagnostopoulos F, Tsikkinis A. Psychosocial factors related to posttraumatic growth in breast cancer survivors: a review. Women Health. 2014; 54(6):569–592.

25. Stanfford L, Foley E, Judd F, Gibson P, Kiropulos L, Couper J. Mindfulness-based cognitive group therapy for women with breast and gynecologic cancer: a pilot study to determine effectiveness and feasibility. Support Care Cancer. 2013; 21:3009–3019.

26. Hasson-Ohayon I, Tuval-Mashiach R, Goldzweig G, Levi R, Pizem N, Kaufman B. The need for friendships and information: dimensions of social support and posttraumatic growth among women with breast cancer. Palliat Support Care. 2015; 14:1–6.

27. Kim HJ, Kwon JH, Kim JN, Lee R, Lee KS. Posttraumatic growth and related factor in breast cancer survivors. Korean J Health Psychol. 2008; 13(3):781–799.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download