Abstract
Purpose
The purpose of this study was to identify the effects of a standardized preoperative education program on self-care knowledge, performance, satisfaction, and physical recovery in the stomach cancer patients undergoing gastrectomy.
Methods
A nonequivalent control group non-synchronized design was utilized and 63 participants who underwent gastrectomy (31 for experimental group, 32 for control group) were recruited at a university hospital from May to August 2015.
Results
There were significant differences between the groups in self-care knowledge (F=17.63, p<.001), performance (F=-9.25, p<.001) and satisfaction (F=-6.91, p<.001). Although the pain levels (F=974.57, p<.001) showed significant differences in each group and 3 time intervals (F=18.26, p<.001), there was no interaction of group and time (F=0.09, p=.917). The highest body temperature at 48 hours after surgery (F=1.32, p=.192), as well as presence of atelectasis (F=2.23, p=.213) indicating a chance of pulmonary complications, and the time of first gas pass (F=-1.05, p=.299), presence of paralytic ileus (F=0.13, p=.719) were not significantly differ.
Figures and Tables
Table 1
Demographic and Disease-related Characteristics (N=63)
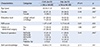
*Chi-square test; Cont.= Control group; Exp.= Experimental group; ASA score= American Society of Anesthesiologist Physical status classification score; RSTG Bl= Radical subtotal gastrectomy with billoth l; RSTG Bll= Radical subtotal gastrectomy with billoth ll; RSTG RY= Radical subtotal gastrectomy with roux-en Y Gastrojejunostomy; RTG= Radical total gastrectomy with Roux-en-Y esophagojejunostomy; Palliative GJ= Palliative gastrojejunostomy.
Table 2
Comparison of Self-care Knowledge, Self-care Performance, Patient Satisfaction between Control Group and Experi-mental Group (N=63)

Table 3
Comparison of Postoperative Physical Recovery between Control Group and Experimental Group (N=63)

References
1. National Cancer Center. Annual report of cancer statistics in Korea in 2012. Annual report. Seoul, Korea: National Cancer Center;2014.
2. Kim JE. A study of nutrition assessment and the analysis of the factors affecting malnutrition after subtotal gastrectomy of gastric cancer patients [master's thesis]. Seoul: Catholic Univ;2002.
3. Lee SS, Han SW, Jeong HY, Song JW, Chung HY, Yu W. Quality of life of long-term survivors after a subtotal or a total gastrectomy for gastric cancer. J Korean Gastric Cancer Assoc. 2010; 10(1):34–39.

4. Kim MS, Park JM, Choi YS, Cha SJ, Kim BG, Chi KC. Risk factors for complications following resection of gastric cancer. J Gastric Cancer. 2010; 10(3):118–125.

5. On~ate-Ocan~a LF, Corte´s-Ca´rdenas SA, Aiello-Crocifoglio V, Mondrago´n-Sa´nchez R, Ruiz-Molina JM. Preoperative multivariate prediction of morbidity after gastrectomy for adenocarcinoma. Ann Surg Oncol. 2000; 7(4):281–288.

6. Kim CJ, Park JW, Yun JS, Kim ON, Kwon YS, Lee HS. A study comparing the perception of patients, nurses, and doctors about the educational needs of cancer patients. Korean Nurse. 1989; 28(1):53–66.
7. Kim MO, Kim UK, Cho EY. The effects of Multimedia diet education on nutritional status in stomach neoplasms patient with gastrectomy. J Korean Clin Nurs Res. 2008; 14(1):45–59.
8. Cho EH, Hwang SY. Effects of the nurse-led discharge education on symptom experience and self-care compliance in patients with chronic obstructive pulmonary disease. Korean J Adult Nurs. 2011; 23(6):595–604.
9. Lee JA, Lee SH, Park JH, Park JH, Kim SG, Seo JH. Analysis of the factors related to the needs of patients with cancer. J Prev Med Public Health. 2010; 43(3):222–234.

10. Hur HK. Information needs of women with breast cancer. J Korean Acad Adult Nurs. 2000; 12(2):286–295.
11. Noh SH, Ryu CH. Can I live without the stomach. Seoul: Cultural History of Medicine;2003.
12. Ahn SH. The effects of individualized cardiac rehabilitation education on knowledge, self-efficacy and health behavior of patients with percutaneous coronary intervention(PCI) [master's thesis]. Seoul: Kyung-hee Univ;2013.
14. Kim HS, Suh EY, Lee HJ, Yang HK. The effects of patient participationbased dietary intervention on nutritional and functional status for patients with gastrectomy: a randomized controlled trial. Cancer Nurs. 2014; 37(2):E10–E20.
16. Hong YL. Effect of preoperative educational DVD on postoperative self care knowledge and performance in lung cancer patient [master's thesis]. Seoul: Han-yang Univ;2007.
17. Jeon MK. Development of self-care performance scale for patients with stomach cancer after gastrectomy [dissertation]. Busan: Ko-sin Univ;2014.
18. Hur HK. Nurses' attitudes toward postoperative pain control. Korean J Adult Nurs. 1994; 6(2):236–250.
19. Haines KJ, Skinner EH, Berney S. The Austin Health POST Study Investigators. Association of postoperative pulmonary complications with delayed mobilization following major abdominal surgery: an observational cohort study. Physiotherapy. 2013; 99:119–125.

20. Mattei P, Rombeau JL. Review of the pathophysiology and management of postoperative ileus. World J Surg. 2006; 30(8):1382–1391.

21. Choi HJ. Comparative study between the patients' satisfaction level of nursing service and revisit intention of the inpatients according to the ward type [master's thesis]. Seoul: Sahm-yook Univ;2014.
22. Kim MS, Park KH. Effects of preoperative nursing education for patient with general anesthetic surgery. J Korean Data Anal Soc. 2012; 14(4):1975–1986.
23. White J, Dixon S. Nurse led patient education programme for patients undergoing a lung resection for primary cancer. J Thorac Dis. 2015; 7(S2):S131–S137.
24. Holman H, Lorig K. Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 2004; 119(3):239–243.

25. Kim MY. Development and effects of a web-based self-efficacy promoting program on stomach cancer patients with gastrectomy [dissertation]. Seoul: Kosin Univ;2009.
26. Hermann F, Gunter FK, Andrea R, Paul P, Hubert A. Effectiveness of education for gastric cancer patients, a controlled prospective trial comparing interactive vs. lecture-based programs. Patient Educ Couns. 2009; 76(2009):91–98.
27. Na IJ, Lee BS. The effect of a telephone follow-up on the self-care and the satisfaction on nursing care in G-I surgical patients. J Korean Acad Nurs Adm. 1999; 5(2):355–368.
28. Park JS, Lee MH, Lee HR. Effects of preoperative pain management education on the control of postoperative pain, focused on the PCA used surgical patients with uterine tumor. J Korean Oncol Nurs. 2011; 11(2):108–115.

29. Kim SS, Sin JH. The effects of systemic pre-operative deep breathing & coughing education to post operative respiratory infection. J Korean Clin Nurs Res. 1997; 3(1):165–185.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download