Abstract
Purpose
The aim of this study is to develop a salivation stimulation method and to verify the effect of a salivation stimulation method on xerostomia in colon cancer patients after surgery.
Methods
This study targeted 21 in the experimental group and 22 in the control group, who were diagnosed with colon cancer and underwent surgery at A university hospital. The salivation stimulation method consists of tongue movement for stimulating minor salivary glands in mouth and a parotid gland and submandibular gland massage with hands. The method was applied four times a day for 2 days the next day after surgery.
Results
On the first postoperative day, the experimental group showed a significantly larger amount of salivation than the control group (p=.010). On the second postoperative day, the experimental group showed a significantly larger amount of salivation than the control group (p<.001). On the first postoperative day, the subjective xerostomia scores in the experimental group and control group were not statistically significant (p=.165). On the second postoperative day, the experimental group showed a significantly lower subjective xerostomia score than the control group (p=.001).
Figures and Tables
Table 1
Homogeneity Test of Demographic Characteristics and Oral-related Characteristics and Operational-related Characteristics (N=43)

Table 2
Homogeneity Test for Pre-operative Dependent Variables of between Two Groups (N=43)
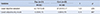
| Variables | Exp. (n=21) | Cont. (n=22) | t | p |
|---|---|---|---|---|
| M±SD | M±SD | |||
| Usual objective salivation | 42.71±13.43 | 37.91±12.17 | 1.23 | .226 |
| Usual subjective dry mouth | 0.33±0.73 | 0.36±0.79 | -0.13 | .897 |
Table 3
Mean difference in Post-operative Objective and Subjective Xerostomia between Two Groups (N=43)

References
1. Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015; 47(2):127–141.

2. Bang SY, Jung GJ, Jung HY, An SH. The effects of gum-chewing on the recovery of bowel movement and oral cavity discomfort after abdominal surgery. J Korean Clin Nurs Res. 2008; 14(3):15–25.
3. Kim MY, Doo MJ, Kang SK, Lim YH, Kim HM, Kim MK, et al. Postoperative patients' thirst and oral status by three oral care methods. J Korean Acad Soc Nurs Educ. 2012; 18(3):403–412.

4. Miranda-Rius J, Brunet-Llobet L, Lahor-Soler E, Farré M. Salivary secretory disorders, inducing drugs, and clinical management. Int J Med Sci. 2015; 12(10):811–824.

5. Song JA, Hur MH. Effects of A-solution on halitosis and oral status in preoperative NPO patients. J Korean Acad Nurs. 2012; 42(3):405–413.

6. Worster B, Holmes S. A phenomenological study of the postoperative experiences of patients undergoing surgery for colorectal cancer. Eur J Oncol Nurs. 2009; 13(5):315–322.

7. Robleda G, Roche-Campo F, Sánchez V, Gich I, Baños JE. Postoperative discomfort after abdominal surgery: an observational study. J Perianesth Nurs. 2015; 30(4):272–279.

8. Korean Academy of Orofacial Pain and Oral Medicine. Oral medicine Vol.Ⅲ. First ed. Seoul: Shinhung International;2010.
9. Greenspan D. Xerostomia: diagnosis and management. Oncology. 1996; 10(3):7–11.
10. Darby ML, Walsh M. Dental hygiene: Theory and practice. 4th ed. hiladelphia: Elsevier Health Sciences;2014.
11. Yoon SY, Min HS. The effects of cold water gargling on thirst, oral cavity condition, and sore throat in orthopedics surgery patients. Korean J Rehabil Nurs. 2011; 14(2):136–144.
12. Lee IS, Shim MS, Na EH, Kang JY, Kim JH, Hwang MY. The comparison of thirst care intervention between the wet gauze and the cold water gargling to the nasal surgery patients. J Korean Clin Nurs Res. 2006; 11(2):21–33.
13. Cho EB. Impact of oral function improving exercise on the oral function and quality of life in the elderly [dissertation]. Daejeon: Chungnam National Univ.;2009.
14. Jang KA, Hwang IC. Objective effects and satisfaction of mouth gymnastics program. J Korea Contents Assoc. 2011; 11(10):388–395.

15. Kim YJ, Choi YH, Kim JY, Lee HK. The effect of orophysical exercise for the elderly on oral function and nutrient intake. J Korean Acad Oral Health. 2011; 35(4):414–422.
16. Kim DY. Effect of a mouth exercise program on improvement of functions and quality of life related to oral health in the elderly [dissertation]. GimHae: Inje Univ.;2012.
17. Ibayashi H, Fujino Y, Pham TM, Matsuda S. Intervention study of exercise program for oral function in healthy elderly people. Tohoku J Exp Med. 2008; 215(3):237–245.

18. Thomson WM, Chalmers JM, Spencer AJ, Williams SM. The Xerostomia Inventory: a multi-item approach to measuring dry mouth. Community Dent Health. 1999; 16(1):12–17.
19. Fox PC, Busch KA, Baum BJ. Subjective reports of xerostomia and objective measures of salivary gland performance. J Am Dent Assoc. 1987; 115(4):581–584.

20. Eilers J, Berger AM, Petersen MC. Development, testing, and application of the oral assessment guide. Oncol Nurs Forum. 1988; 15(3):325–330.
21. Chu HR, Kim CH, Lee JS, Park SK, Koh ES, Rho YS. Diagnosis of salivary gland function using oral schirmer test. Korean J Otorhinolaryngol-Head Neck Surg. 2008; 51(2):153–156.
22. Humphrey SP, Williamson RT. A review of saliva: normal composition, flow, and function. J Prosthet Dent. 2001; 85(2):162–169.

23. Yarbro CH, Wujcik D, Gobel BH. Cancer symptom management. 4th ed. Burlington: Jones & Bartlett Learning;2013.
24. National Cancer Information Center. Dry mouth. October 19, 2015. http://www.cancer.
go.kr /mbs/cancer/subview.jsp?id=cancer_030202020200.
25. National Cancer Institute. Managing oral complications during and after chemotherapy or radiation Therapy. September 28, 2015. http://www.cancer.gov/aboutcancer/treatment/side-effects/mouth-throat/oral-complicationspdq#section/_9.
27. Kang H, Yeon K, Han ST. A review on the use of effect size in nursing research. J Korean Acad Nurs. 2015; 45(5):641–649.

28. Guggenheimer J, Moore PA. Xerostomia: Etiology, recognition and treatment. J Am Dent Assoc. 2003; 134(1):61–69.
29. Kim SS, Youn HJ. Associated factors of self-reported dry mouth in adults. J Korean Soc Dent Hyg. 2015; 15(1):55–62.

30. Park HR. A study on the status of practical application of oral hygiene devices: with labor of the D heavy industries. J Dent Hyg Sci. 2006; 6(2):93–99.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download