Abstract
Purpose
The purpose of this study was to investigate the severity of subjective sleep quality and factors related to sleep disturbances in breast and gynecologic cancer patients undergoing radiotherapy.
Methods
Ninety four women (68 breast cancer and 26 gynecologic cancer) undergoing radiotherapy were recruited and asked to complete the Pittsburg Sleep Quality Index (PSQI), Piper Fatigue Scale, and Hospital Anxiety Depression Scale. The data were analyzed using χ2-test, t-test, ANOVA and logistic regression.
Results
The average global PSQI score was 8.34± 4.41 and 70.2% of the patients reported poor sleep quality (PSQI> 5). There were significant differences between the poor sleepers and the good sleepers in concurrent chemo-radiotherapy (p= .022), number of radiation treatments (p=.013), total amount of radiation dosage (p=.048), sleeping pills (p=.030), fatigue (p< .001), anxiety (p<.001), and depression (p=.024). Logistic regression showed that significant predictors for poor sleep quality were fatigue and concurrent chemo-radiotherapy.
Conclusion
These findings suggest that sleep disturbance was a significant health problem in patients with breast and gynecologic cancer who were receiving radiotherapy. Also that fatigue and concurrent chemo-radiotherapy were highly associated with sleep disturbance. However, limited evidence was found for the role of radiotherapy in the sleep disturbance of these patients.
Figures and Tables
 | Fig. 1Mean scores of the PSQI components. Higher scores indicate greater sleep disturbance (PSQI=Pittsburgh Sleep Quality Index). |
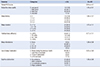
Table 1
Differences in General and Clinical Characteristics according to Sleep Quality (N=94)
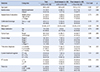
Table 2
Differences in the Levels of Fatigue, Anxiety and Depression according to Sleep Quality (N=94)

Table 3
PSQI Component Scores of Participants (N=94)
References
1. Baskar R, Lee KA, Yeo R, Yeoh KW. Cancer and radiation therapy: current advances and future directions. Int J Med Sci. 2012; 9(3):193–199.

2. Matthews EE, Schmiege SJ, Cook PF, Sousa KH. Breast cancer and symptom clusters during radiotherapy. Cancer Nurs. 2012; 35(2):E1–E11.

3. Van Onselen C, Dunn LB, Lee K, Dodd M, Koetters T, West C, et al. Relationship between mood disturbance and sleep quality in oncology outpatients at the initiation of radiation therapy. Eur J Oncol Nurs. 2010; 14(5):373–379.

4. Miaskowski C, Lee K, Dunn L, Dodd M, Aouizerat BE, West C, et al. Sleep-wake circadian activity rhythm parameters and fatigue in oncology patients before the initiation of radiation therapy. Cancer Nurs. 2011; 34(4):255–268.

5. Knobf MT, Sun Y. A longitudinal study of symptoms and self-care activities in women treated with primary radiotherapy for breast cancer. Cancer Nurs. 2005; 28(3):210–218.

6. Roscoe JA, Kaufman ME, Matteson-Rusby SE, Palesh OG, Ryan JL, Kohli S, et al. Cancer-related fatigue and sleep disorders. Oncologist. 2007; 12:Suppl 1. 35–42.

7. Stiegelis HE, Ranchor AV, Sanderman R. Psychological functioning in cancer patients treated with radiotherapy. Patient Educ Couns. 2004; 52(2):131–141.

8. Jeong JY, So HS, Hong JE, Chea MJ, Han G. Related factors to quality of life among hospitalized cancer patients undergoing chemotherapy. Asian Oncol Nurs. 2012; 12(1):84–91.

9. Sohn SK. Relationship between fatigue and sleep quality in patients with cancer. Korean J Adult Nurs. 2002; 14(3):378–389.
10. Fenlon DR, Corner JL, Haviland J. Menopausal hot flushes after breast cancer. Eur J Cancer Care (Engl). 2009; 18(2):140–148.

11. Berger AM, Treat Marunda HA, Agrawal S. Influence of menopausal status on sleep and hot flashes throughout breast cancer adjuvant chemotherapy. J Obstet Gynecol Neonatal Nurs. 2009; 38(3):353–366.

12. Kirkova J, Rybicki L, Walsh D, Aktas A. Symptom prevalence in advanced cancer: age, gender, and performance status interactions. Am J Hosp Palliat Care. 2012; 29(2):139–145.
13. Park J, Bang Y, Ha S, Jeong S, Oh D, Chie E. Oncology. Seoul: Ilchokak;2012.
14. Huh SJ. Present status and future aspects of radiation oncology in Korea. Radiat Oncol J. 2006; 24(4):211–216.
15. Sohn SI, Kim do H, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012; 16(3):803–812.

16. Lee EH. Fatigue in people with cancer - concept analysis. J Korean Acad Nurs. 1999; 29(4):755–765.
17. Oh SM, Min KJ, Park DB. A comparison of normal, depressed and anxious groups=A Study on the standardization of the hospital anxiety and depressed scale for Koreans. J Korean Neuropsychiatr Assoc. 1999; 38(2):289–296.
18. Mo YL, Li L, Qin L, Zhu XD, Qu S, Liang X, et al. Cognitive function, mood, and sleep quality in patients treated with intensity-modulated radiation therapy for nasopharyngeal cancer: a prospective study. Psychooncology. 2014; 23(10):1185–1191.

19. Garrett K, Dhruva A, Koetters T, West C, Paul SM, Dunn LB, et al. Differences in sleep disturbance and fatigue between patients with breast and prostate cancer at the initiation of radiation therapy. J Pain Symptom Manage. 2011; 42(2):239–250.

20. Yi H. Sleep quality and its associated factors in adults. J Korean Public Health Nurs. 2013; 27(1):76–88.

21. MOHW and KCDC. Korea Health Statistics 2010: Korean National Health and Nutrition Examination Survey. Seoul: Korea Center for Disease Control and Prevention;2011.
22. Otte JL, Rand KL, Carpenter JS, Russell KM, Champion VL. Factor analysis of the Pittsburgh Sleep Quality Index in breast cancer survivors. J Pain Symptom Manage. 2013; 45(3):620–627.

23. Hofso K, Miaskowski C, Bjordal K, Cooper BA, Rustoen T. Previous chemotherapy influences the symptom experience and quality of life of women with breast cancer prior to radiation therapy. Cancer Nurs. 2012; 35(3):167–177.

24. Park KS. Changes in side effects and fatigue of cancer patients receiving radiation therapy. J Korean Oncol Nurs. 2002; 2(1):72–82.
25. Park JH. Patterns and related factors of fatigue during radiotherapy in patients with breast cancer. J Korean Acad Adult Nurs. 2003; 15(1):33–44.
26. Park JH. Sleep quality of breast cancer patients receiving chemotherapy in the outpatients setting. Seoul: Yonsei Univ;2011.
27. Kim YH, Lee JH. Relationships between side effects, depression and quality of sleep in gynecological cancer patients undergoing chemotherapy. Korean J Women Health Nurs. 2010; 16(3):276–287.

28. Kim L. Stress, sleep physiology, and related insomnia disorders. J Korean Med Assoc. 2010; 53(8):707–716.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download