Abstract
Purpose
The purpose of this study was to identify changes of supportive care needs and relationship to quality of life (QOL) in patients with breast cancer.
Methods
117 patients with breast cancer were administered the Supportive Care Needs Survey-Short form 34 and the Functional Assessment of Cancer Therapy-Breast before adjuvant therapy after mastectomy (T1), at the end of completing adjuvant therapy (T2), as well as 6 months after the completion of adjuvant therapy (T3). Data were analyzed using SPSS/Win 21.0.
Results
The highest unmet supportive care needs were observed in the health system and information domain and the psychological domain at each time point. The health system and information (F=22.49, p<.001) and physical and daily living needs (F=5.72, p=.004) were higher at T1 and T2 than T3. The psychological (F=7.43, p=.001) and patient care and support needs were higher at T1 than T2 and T3. Multiple regression analysis showed that breast cancer patients with greater physical and daily living and psychological needs were significantly associated with poorer QOL at all times.
Figures and Tables
Table 1
Demographic and Clinical Characteristics of the Participants (N=117)

Table 2
Prevalence of Top 10 Unmet Supportive Care Needs (N=117)

Table 3
Change in Supportive Care Needs Over Time (N=117)
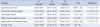
Table 4
Regression Model with Quality of life as the Dependent Variable (N=117)

References
1. National Cancer Information Center. Accessed October 15, 2016. http://www.cancer.go.kr.
2. Korean breast cancer society. Accessed October 15, 2016. http://www.kbcs.or.kr.
3. Ham YH. Supportive care needs of patients with advanced lung cancer [Master's thesis]. Seoul: Sungkyunkwan Univ.;2009.
4. Park BW, Hwang SY. Unmet needs of breast cancer patients relative to survival duration. Yonsei Med J. 2012; 53(1):118–125.

5. So WK, Chow KM, Chan HY, Choi KC, Wan RW, Mak SS, et al. Quality of life and most prevalent unmet needs of Chinese breast cancer survivors at one year after cancer treatment. Eur J Oncol Nurs. 2014; 18(3):323–328.

6. So WK, Chan CW, Choi K, Wan RW, Mak SS. Perceived unmet needs and health-related quality of life of Chinese cancer survivors at 1 year after treatment. Cancer Nurs. 2013; 36(3):E23–E32.

7. Edib Z, Kumarasamy V, Binti Abdullah N, Rizal A, Al-Dubai SA. Most prevalent unmet supportive care needs and quality of life of breast cancer patients in a tertiary hospital in Malaysia. Health Qual Life Outcomes. 2016; 14(1):26.

8. Lam WW, Tsang J, Yeo W, Suen J, Ho WM, Yau TK, et al. The evolution of supportive care needs trajectories in women with advanced breast cancer during the 12 months following diagnosis. Support Care Cancer. 2014; 22(3):635–644.

9. Boyes AW, Girgis A, D'Este C, Zucca AC. Prevalence and correlates of cancer survivors' supportive care needs 6 months after diagnosis: a population-based cross-sectional study. BMC Cancer. 2012; 12:150.
10. Liao MN, Chen SC, Chen SC, Lin YC, Hsu YH, Hung HC, et al. Changes and predictors of unmet supportive care needs in Taiwanese women with newly diagnosed breast cancer. Oncol Nurs Forum. 2012; 39(5):E380–E389.

11. Uchida M, Akechi T, Okuyama T, Sagawa R, Nakaguchi T, Endo C, et al. Patients' supportive care needs and psychological distress in advanced breast cancer patients in Japan. Jpn J Clin Oncol. 2011; 41(4):530–536.

12. Akechi T, Okuyama T, Endo C, Sagawa R, Uchida M, Nakaguchi T, et al. Patient's perceived need and psychological distress and/or quality of life in ambulatory breast cancer patients in Japan. Psychooncology. 2011; 20(5):497–505.

13. Pathy NB, Yip CH, Taib NA, Hartman M, Saxena N, Iau P, et al. Breast cancer in a multi-ethnic Asian setting: results from the Singapore-Malaysia hospital-based breast cancer registry. Breast. 2011; 20:S75–S80.
14. Zebrack BJ, Corbett V, Embry L, Aguilar C, Meeske KA, Hayes-Lattin B, et al. Psychological distress and unsatisfied need for psychosocial support in adolescent and young adult cancer patients during the first year following diagnosis. Psychooncology. 2014; 23(11):1267–1275.

15. Minstrell M, Winzenberg T, Rankin N, Hughes C, Walker J. Supportive care of rural women with breast cancer in Tasmania, Australia: changing needs over time. Psychooncology. 2008; 17(1):58–65.

16. Schmid-Büchi S, Halfens RJ, Müller M, Dassen T, van den Borne B. Factors associated with supportive care needs of patients under treatment for breast cancer. Eur J Oncol Nurs. 2013; 17(1):22–29.

17. Willems RA, Bolman CA, Mesters I, Kanera IM, Beaulen AA, Lechner L. Cancer survivors in the first year after treatment: the prevalence and correlates of unmet needs in different domains. Psychooncology. 2016; 25(1):51–57.

18. Brennan ME, Boyle FM, Butow PN, Spillane AJ. Evaluation of a survivorship care plan: long-term use, care coordination and quality of life in breast cancer survivors. Breast Cancer. 2015; 4(3):145–157.

19. Cheng KK, Devi RD, Wong W, Koh C. Perceived symptoms and the supportive care needs of breast cancer survivors six months to five years post-treatment period. Eur J Oncol Nurs. 2014; 18(1):3–9.

20. Armes J, Crowe M, Colbourne L, Morgan H, Murrells T, Oakley C, et al. Patients' supportive care needs beyond the end of cancer treatment: a prospective, longitudinal survey. J Clin Oncol. 2009; 27(36):6172–6179.

21. Brédart A, Merdy O, Sigal-Zafrani B, Fiszer C, Dolbeault S, Hardouin JB. Identifying trajectory clusters in breast cancer survivors' supportive care needs, psychosocial difficulties, and resources from the completion of primary treatment to 8 months later. Support Care Cancer. 2016; 24(1):357–366.

22. Burris JL, Armeson K, Sterba KR. A closer look at unmet needs at the end of primary treatment for breast cancer: a longitudinal pilot study. Behav Med. 2015; 41(2):69–76.

23. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New Jersey: Lawrence Elbaum Associates;1988.
24. Boyes A, Girgis A, Lecathelinais C. Brief assessment of adult cancer patients' perceived needs: development and validation of the 34-item Supportive Care Needs Survey (SCNS-SF34). J Eval Clin Pract. 2009; 15(4):602–606.

25. Brady MJ, Cella DF, Mo F, Bonomi AE, Tulsky DS, Lloyd SR, et al. Reliability and validity of the functional assessment of cancer therapy-breast quality-of-life instrument. J Clin Oncol. 1997; 15(3):974–986.

26. Yoo HJ, Ahn SH, Eremenco S, Kim H, Kim WK, Kim SB, et al. Korean translation and validation of the functional assessment of cancer therapy-breast (FACT-B) scale version 4. Qual Life Res. 2005; 14(6):1627–1632.

27. Hwang E, Yi M. Factors influencing quality of life in patients with breast cancer on hormone therapy. J Korean Acad Nurs. 2014; 44(1):108–117.

28. Miyashita M, Ohno S, Kataoka A, Tokunaga E, Masuda N, Shien T, et al. Unmet information needs and quality of life in young breast cancer survivors in Japan. Cancer Nurs. 2015; 38(6):E1–E11.

29. Akechi T, Momino K, Miyashita M, Sakamoto N, Yamashita H, Toyama T. Anxiety in disease-free breast cancer patients might be alleviated by provision of psychological support, not of information. Jpn J Clin Oncol. 2015; 45(10):929–933.

30. Kim HY, So HS, Chae MJ, Kim KM. Comparisons of quality of life, sexual function, and depression in sexually active or inactive groups of women with mastectomy. J Korean Oncol Nurs. 2008; 8(2):77–85.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download