Abstract
Purpose
Cancer survivors have experienced a specific and unique situation. Diet plays an important role in cancer risk and it is important influences on health. The purpose of this study was to explore the impact of social cognitive constructs, which is defined in Bandura's social cognitive theory, on dietary behaviors in breast cancer survivors.
Methods
A cross-sectional correlational design was used. Social cognitive constructs included nutritional self-efficacy, dietary goal-setting, outcome expectations for nutrition, negative impact of cancer, and social support. Stepwise multiple regression was applied to examine the impact of social cognitive constructs on dietary behaviors.
Results
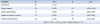
One hundred and fifty-one breast cancer survivors completed the questionnaire. Stepwise regression analyses revealed that 19.9% of the variance in dietary behaviors was explained by these social cognitive variables. Family support, dietary goal-setting, negative impact of cancer, and nutritional self-efficacy were significant predictors of dietary behaviors.
Conclusion
A lack of social cognitive understanding about cancer survivors could result in less than adequate care for their health due to inadequate advice on their lifestyle choices, which may impede their opportunities to live healthy lives after overcoming the cancer. The knowledge from this study will help guide the development of social cognitive interventions.
Figures and Tables
Table 1
The Scores of Dietary Behaviors and Social Cognitive Determinants (N=151)
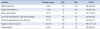
Table 2
Correlations among Dietary Behaviors and Social Cognitive Determinants (N=151)
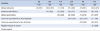
Table 3
Differences of Dietary Behaviors by Characteristics (N=151)
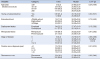
Table 4
Predictors for Dietary Behaviors (N=151)
References
1. National Cancer Information Center. National cancer statistics. Accessed December 23, 2015. http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_040101000000.
2. National Cancer Institute. SEER Cancer Statistics Review, 1975-2013. Accessed September 12, 2016. http://seer.cancer.gov/statfacts/html/breast.html.
3. E Lyon D, Mohanraj L, Kelly DL, Elswick R Jr. Health promoting lifestyle behaviors and systemic inflammation in African American and Caucasian women prior to chemotherapy for breast cancer. Health Promot Perspect. 2014; 4(1):18–26.
4. Jeong K, Heo JE, Tae YS. Relationships among distress, family support, and health promotion behavior in breast cancer survivors. Asian Oncol Nurs. 2014; 14(3):146–154.

5. Kim IS. Dietary therapy among breast cancer patients. In : Annual Spring Congress of Korean Surgical Society; 2007 May 10-11; Jeju, Korea. Dbpia;5:p. 75–76.
6. Bandura A. Social cognitive theory in cultural context. Appl Psychol Int Rev. 2002; 51(2):269–290.

8. Stacey FG, James EL, Chapman K, Courneya KS, Lubans DR. A systematic review and meta-analysis of social cognitive theory-based physical activity and/or nutrition behavior change interventions for cancer survivors. J Cancer Surviv. 2015; 9(2):305–338.

9. National Coalition for Cancer Survivorship. Defining cancer survivorship. Accessed July 24, 2014. https://www.canceradvocacy.org/news/defining-cancer-survivorship.
10. Schwarzer R, Renner B. Health-specific self-efficacy scales. 2009. Accessed March 11, 2015. http://userpage.fu-berlin.de/health/healself.pdf.
11. Rovniak LS, Anderson ES, Winett RA, Stephens RS. Social cognitive determinants of physical activity in young adults: a prospective structural equation analysis. Ann Behav Med. 2002; 24:149–156.

12. Doerksen S, McAuley E. Social cognitive determinants of dietary behavior change in university employers. Front Public Health. 2014; 2(23):1–7.
13. Baranowski T, Davis M, Resnicow K, Baranowski J, Doyle C, Lin LS, et al. Gimme 5 fruit, juice and vegetables for fun and health: Outcome Evaluation. Health Educ Behav. 2000; 27(1):96–111.

14. Tae YS. A study on the correlation between perceived social support and depression of the cancer patients [master's thesis]. Seoul: Ewha Univ.;1986.
15. Crespi CM, Ganz PA, Petersen L, Castillo A, Caan B. Refinement and psychometric evaluation of the impact of cancer scale. J Natl Cancer Inst. 2008; 100:1530–1541.

16. Smith SK, Crespi CM, Petersen L, Zimmerman S, Ganz PA. The impact of cancer and quality of life for post-treatment non-Hodgkin lymphoma survivors. Psychooncology. 2010; 19(12):1259–1267.

17. Walker SN, Sechrist KR, Pender NJ. The health-promoting lifestyle profile: development and psychometric characteristics. Nurs Res. 1987; 36:76–81.
18. Acton GJ, Malathum P. Basic need status and health-promoting selfcare behavior in adults. West J Nurs Res. 2000; 22(7):796–811.

19. Lee EJ. Family support, Self-esteem and health promotion behavior in uterine cancer patients [master's thesis]. Seoul: Chungang Univ.;2012.
20. Seo MH, Lim KH. The effect of fatigue and distress on self-efficacy among breast cancer survivors. J Korean Acad Adult Nurs. 2016; 28(4):378–387.

21. Jeong HO. A study on developing korean food brands. J Korean Stud. 2006; 8:161–191.
22. Drost FM, Mols F, Kaal SE, Stevens WB, van der Graaf WT, Prins JB, et al. Psychological impact of lymphoma on adolescents and young adults: not a matter of black or white. J Cancer Surviv. 2016; 10(4):726–735.

23. Cho HM. Effects of psychological acceptance and social support on posttraumatic growth in stomach cancer patients [master's thesis]. Seoul: Ewha Univ.;2015.
24. Kim JH, Lee EH, Hyun HJ, Gil JH, Kim JS, Park YS, et al. A Study of the Affecting Factors on the Health Promoting Behaviors of the Clinical Nurses. J Korean Biol Nurs Sci. 2009; 11(2):143–148.
25. Kang CH. Effects of support of family, self-efficacy, health literacy and perceived health status on health-promoting behavior among married immigrant women [master's thesis]. Gyeongju: Dongkuk Univ.;2016.
26. Nothwehr F, Yang J. Goal setting frequency and the use of behavioral strategies related to diet and physical activity. Health Educ Res. 2007; 22(4):532–538.

27. White SM, Wojcicki TR, McAuley E. Social cognitive influences on physical activity behavior in middle-aged and older adults. J Gerontol B Psychol Sci Soc Sci. 2011; 67B(1):18–26.

28. Lee JR, Lee KW, Jin EK, Park BN, Son Y. Relationship among resilience, family support and health promotion of hospitalized cancer patients in an advanced general hospital. J Korea Inst Orient Med Inf. 2015; 21(2):35–45.
29. Kim EK, Park YS. Health promotion, stress and quality of life in patients with genital neoplasms. Korean J Rehabil Nurs. 2010; 13(2):114–122.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download