Abstract
Purpose
This study aimed to find the relationships between quality of sleep, symptoms, depression, and anxiety in patients with colorectal cancer.
Methods
A cross-sectional correlation study was used. Participants were 138 colorectal cancer patients undergoing chemotherapy. Measurements included the self-reported Pittsburgh Sleep Quality Index (PSQI), the Hospital Anxiety Depression Scale (HADS), the M. D. Anderson Symptom Inventory (MDASI-GI) and the patients' medical history.
Results
87.0% of subjects were assessed as poor sleepers. The most severe symptoms reported were feeling bloated, followed by fatigue, and sadness. The prevalence of anxiety and depression were 68.2%, and 77.5% respectively. According to the result of multiple regression analysis, symptoms, depression, cancer severity, and comorbidity of chronic illness were significant predictors of quality of sleep scores (Adj. R2=.392, p<.001)
Figures and Tables
Table 1
Differences in Quality of Sleep by Characteristics (N=138)

Table 2
Pittsburgh Sleep Quality Index (PSQI) Global Scores and Component Means (N=138)
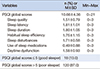
Table 3
Symptom Reported by Respondents
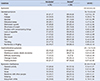
Table 4
Hospital Anxiety-Depression Reported by Respondents
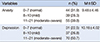
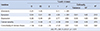
Table 5
Contributing Factors to Quality of Sleep (N=138)
References
1. Korea Central Cancer Resistry. National Cancer Center. Annual report of cancer statistics in Korea in 2011. Ministry of Health and Welfare;Accessed September 10, 2013. http://ncc.re.kr/manage/manage03_033_list.jsp.
2. Park JA, Choi KS. Experience of colorectal cancer survival journeys: born again after going through an altered self image. Asian Oncol Nurs. 2013; 13(3):163–173.

3. Harrison's Manual of Medicine, 18e> Chap 78: tumors of the gastrointestinal tract. Accessed June 25, 2016. http://accessmedicine.mhmedical.com/content.aspx?sectionid=63499554&bookid=1140&jumpsectionID=63499602&Resultclick=2.
4. Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh sleep quality index. J Psychosom Res. 1998; 45(1):5–13.

5. Sohn SK. Relationship between fatigue and sleep quality in patients with cancer. J Korean Acad Adult Nurs. 2002; 14(3):378–389.
6. Berger AM, Treat Marunda HA, Agrawal S. Influence of menopausal status on sleep and hot flashes throughout breast cancer adjuvant chemotherapy. J Obstet Gynecol Neonatal Nurs. 2009; 38(3):353–366.

7. Kim K, Park DH, Park DL, Ryu EJ. Effects of symptom severity and symptom interference on sleep disturbance in cancer patients. Asian Oncol Nurs. 2012; 12(4):339–346.

8. Monas L, Suzanne C, Michal K, Ruthie Z, Yossi FD, Catherine F. The relationship of sleep disturbance and symptom severity, symptom interference, and hospitalization among Israeli inpatients with cancer. Oncol Nurs Forum. 2012; 39(4):E361–E372.

9. Simon AE, Thompson M, Flashman K, Wardle J. Disease stage and psychosocial outcomes in colorectal cancer. Colorectal Dis. 2009; 11(1):19–25.

10. Vena C, Parker K, Cunningham M, Clark J, McMillan S. Sleep-wake disturbances in people with cancer part I: an overview of sleep, sleep regulation, and effects of disease and treatment. Oncol Nurs Forum. 2004; 31:735–746.

11. Kwak MJ. A study on the relationship of pain, anxiety, and sleep in the cancer patients [master's thesis]. Seoul: Ewha Womans Univ.;2000.
12. Son HG. Relationship between quality of sleep and fatigue in patients with hemato-malignancy in receiving chemotherapy [master's thesis]. Busan: Kosin Univ.;2007.
13. Jung JE. The comparison of the perceived nursing needs between hospitalized cancer patients, and nurses. J Korean Clin Nurs Res. 2003; 8(2):91–105.
14. Park JH. Sleep quality of breast cancer patients receiving chemotherapy in the outpatients setting [master's thesis]. Seoul: Yonsei Univ.;2011.
15. Otte JL, Carpenter JS, Russell KM, Bigatti S, Champion VL. Prevalence, severity, and correlates of sleep-wake disturbances in long-term breast cancer survivors. J Pain Symptom Manage. 2010; 39(3):535–547.

16. Berger AM, Grem JL, Visovsky C, Marunda HA, Yurkovich JM. Fatigue and other variables during adjuvant chemotherapy for colon and rectal cancer. Oncol Nurs Forum. 2010; 37(6):E359–E369.

17. Buysse DJ, Reynolds III CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2):193–213.

18. Cho YW, Lee H, Lee JH, Han SY, Lee MY. Sleep disorders in maintenance dialysis patients with end-stage renal disease. J Korean Neurol Assoc. 2003; 21(5):492–497.
19. Cleeland CS, Mendoza TR, Wang XS, Chou C, Harle MT, Morrissey M, et al. Assessing symptom distress in cancer patients. Cancer. 2000; 89(7):1634–1646.

20. Wang XS, Williams LA, Eng C, Mendoza TR, Shah NA, Kirkendoll KJ, et al. Validation and application of a module of the MD Anderson Symptom Inventory for measuring multiple symptoms in patients with gastrointestinal cancer(the MDASI-GI). Cancer. 2010; 116(8):2053–2063.

21. Baek YA. The Correlation among symptoms, anxiety, depression and quality of life in patients with colorectal cancer undergoing chemotherapy [master's thesis]. Seoul: Seoul National Univ.;2013.
22. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67(6):361–370.

23. Baldacchino DR, Bowman GS, Buhagiar A. Reliability testing of the hospital anxiety and depression (HAD) scale in the English, Maltese and back-translation versions. Int J Nurs Stud. 2002; 39:207–214.

24. Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. "Sleep disparity" in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. 2010; 11(10):475. DOI: 10.1186/1471-2458-10-475.

25. Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE, et al. Association of usual sleep duration with hypertension: the sleep heart health study. Sleep. 2006; 29(8):1009–1014.

26. Anderson KO, Getto CJ, Mendoza TR, Palmer SN, Wang XS, Reyes-Gibby CC, et al. Fatigue and sleep disturbance in patients with cancer, patients with clinical depression, and community-dwelling adults. J Pain Symptom Manage. 2003; 25(4):307–318.

27. Sela RA, Watanabe S, Nekolaichuk CL. Sleep disturbances in palliative cancer patients attending a pain and symptom control clinic. Palliat Support Care. 2005; 3(1):23–31.

28. Engstrom PF, Arnoletti JP, Benson AB 3rd, Chen YJ, Choti MA, Cooper HS, et al. NCCN clinical practice guidelines in oncology: rectal cancer. J Natl Compr Canc Netw. 2009; 7(8):838–881.
29. Jung AR, Yi M. Predictive factors of supportive care needs in patients with hematologic malignancy. Korean J Adult Nurs. 2011; 23(5):460–471.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download