Abstract
Purpose
This study aimed to identify the factors influencing human papillomavirus (HPV) vaccination adoption stages using the Precaution Adoption Process model.
Methods
A total of 173 female university students from B metropolitan city participated. Demographics, factors contributing to action, knowledge, health beliefs, and self-efficacy related to the HPV vaccination were measured. The collected data were analyzed using descriptive statistics and multiple logistic regression analysis using SPSS for Windows version 21.0.
Results
Factors that contributed to the transition from the unaware and unengaged stages to the undecided about action stage included age, economic status, experience of recommendation from doctors, perceived severity of cervical cancer, and perceived barriers. Factors that contributed to the transition from the undecided about action stage to the deciding to act stage were perceived benefit and self-efficacy of the HPV vaccination. Factors that contributed to the transition from the deciding to act stage to the acting and maintenance stages were experience of recommendation from doctors and perceived severity of cervical cancer.
Figures and Tables
Table 1
Demographics, Knowledge, Health Belief, and Self-efficacy Related to HPV Vaccination (N=173)

Table 2
Stage of HPV Vaccination (N=173)
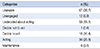
| Categories | n (%) |
|---|---|
| Unaware | 67 (38.7) |
| Unengaged | 12 (6.9) |
| Undecided about acting | 33 (19.1) |
| Decide not to act | 1 (0.6) |
| Decide to act | 18 (10.4) |
| Acting | 36 (20.8) |
| Maintenance | 6 (3.5) |
Table 3
Factors Affecting Stage of HPV Vaccination (Simple Logistic Regression) (N=172)
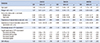
Table 4
Factors Affecting Stage of HPV Vaccination (Multiple Logistic Regression) (N=172)

References
1. Kim HW. Effects of prevention education on human papillomavirus linked to cervix cancer for unmarried female university students. J Korean Acad Nurs. 2009; 39(2):490–498.

2. World Health Organization Website. Assessed October 9, 2010. http://www.who.int/reproductivehealth/topics/cancers/en.
3. Dunne EF, Unger ER, Sternberg M, MeQuillan G, Swan DC, Patel SS, et al. Prevalence of HPV infection among females in the united states. JAMA. 2007; 297(8):813–819.

4. Choi KA, Kim JH, Lee KS, Oh JK, Liu SN, Shin HR. Knowledge of human papillomavirus infection and acceptability of vaccination among adult women in Korea. Obstet Gynecol Sci. 2008; 51(6):617–623.
5. Kim CJ, Kim BK, Kim SC, Kim YT, Kim YM, Park SY. Sexual behavior of Korean young women: preliminary study for the introducing of HPV prophylactic vaccine. J Gynecol Oncol. 2007; 18(3):209–218.

6. Goldie SJ, Kohli M, Grima D, Weinstein MC, Wright TC, Bosch FX, et al. Projected clinical benefits and cost-effectiveness of human papillomavirus 16/18 vaccine. J Natl Cancer Inst. 2004; 96:604–615.

7. Ho GY, Bierman R, Beardsley L, Chang CJ, Burk RD. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med. 1998; 338:423–428.

8. Kim CJ, Park TC, Park JS. Recent clinical review: efficacy of human papillomavirus vaccines including cross protection: a review of recent evidence. Obstet Gynecol Sci. 2010; 53(2):103–118.

9. Castellsagué X, Schneider A, Kaufmann AM, Bosch FX. HPV vaccination against cervical cancer in women above 25years of age: key considerations and current perspectives. Gynecol Oncol. 2009; 115:3 Suppl. S15–S23.
10. Lee EJ, Park JS. Knowledge about cervical cancer, health beliefs and human papillomavirus vaccination rate in female university students. Asian Oncol Nurs. 2011; 11(1):65–73.

11. Kim JH, Park MK. Study on the knowledge of cervical cancer and human papillomavirus and preventive behavior intention of female university students. J Korean Acad Soc Nurs Educ. 2009; 15(2):225–231.

12. Ko KM. The impact of health campaigns on the public's awareness & behavior regarding cervical cancer [master's thesis]. Seoul: Ehwa Womans Univ;2012.
13. Prochaska JO, Diclemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983; 51:390–395.

14. Blalock SJ, DeVellis RF, Giorgino KB, DeVellis BM. Osteoporosis prevention in premenopausal women: using a stage model approach to examine the predictors of behavior. Health Psychology. 1996; 15(2):84–93.

15. Choi SR. Factors associated with stages of adoption for breast cancer screening based on the PAPM [master's thesis]. Daejeon: Chungnam National Univ;2012.
17. Becker MH, Maiman LA, Kirscht JP, Haefner DP, Drachman RH. The health belief model and prediction of dietary compliance: a field experiment. J Health Soc Behav. 1977; 18(4):348–366.

18. Lee SH. Relationship between knowledge level and cancer-prevention performance in anti-cancer vaccine of human papilloma virus (HPV) and cervical cancer in women [master's thesis]. Seoul: Ewha Womans Univ.;2009.
19. Lipschitz JM, Fernandez AC, Larson HE, Blaney CL, Meier KS, Redding CA, et al. Validation of decisional balance and self-efficacy measures for HPV vaccination in college women. Am J Health Promot. 2012; 27(5):299–307.

20. Oh JW, Moon YS. Factors associated with stages of adoption for breast cancer screening: based on the Precaution Adoption Process Model-focusing on comparisons between nurses and general women-. J Korea Contents Assoc. 2012; 12(11):246–257.

21. Kye SY, Choi KS, Sung NY, Kwak MS, Park SH, Bang JY, et al. Using the PAPM to examine factors associated with stages of adoption for stomach cancer screening. Korean J Health Educ Promot. 2006; 23(4):29–45.
22. National Cancer Information Center Website. Assessed March 10, 2014. http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_040101000000.
23. Lee HJ, Lee SH, Jung SH, Shin HL, Oh DK. Analysis of behavioral stage in pap testing by using Transtheoretical Model. J Prev Med Public Health. 2005; 38(1):82–92.
24. Kim HW, Ahn HY. Study on the knowledge of human papillomavirus in female university students. Korean J Women Health Nurs. 2007; 13:13–20.

25. Kwon YE. Konwledge on cervical cancer & human papillomavirus infection of female university students and preventive behavior intention [master's thesis]. Busan: Kosin Univ;2014.
26. Lee KS. Prediction cervix cancer screening behavior using the theory of planned behavior [dessertation]. Seoul: Seoul National Univ;1999.
27. Kye SY. A prediction model for stages of change in cancer screening [dissertation]. Seoul: Ewha Womans Univ;2009.
28. Kang MJ, Lee MS. Integrating the Precaution Adoption Process Model and the Health Belief Model to assess cancer screening readiness among Korean adults. Korean J Health Educ Promot. 2011; 28(3):83–98.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download