Abstract
Purpose
The aims of this study was to identify factors associated with nutritional status after radical gastrectomy in patients with gastric cancer at the post 1 month and the post 3-6 months independently.
Methods
Participants consisted of 107 patients at the post 1 month and 131 patients at the post 3-6 months after radical gastrectomy. Data were collected from October 1, 2013 to May 14, 2014 using a Patient-Generated Subjective Global Assessment (PG-SGA), the Hospital Anxiety and Depression Scale (HADS) and the Connor-Davidson Resilience Scale (CD-RISC).
Results
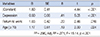
Stepwise multiple regression showed that factors associated with nutritional status at 1 month after radical gastrectomy were age (β=.55, p<.001), anxiety (β=.25, p=.007), and depression (β=.23, p=.017), which explained the 42.6% of total variance of nutritional status. However, factors associated with nutritional status at 3-6 months after radical gastrectomy were depression (β=.41, p=.017), return to work (β=.20, p<.001), and age (β=.29, p=.024), which explained 27.1% of the total variance of nutritional status.
Figures and Tables
Table 1
Continuous Variables after Radical Gastrectomy
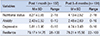
Table 2
Nutritional Status according to General and Clinical Characteristics of Participants at the 1 Month and 3~6 Months after Radical Gastrectomy

*Participants who they've had an occupation before operation; †Normal level of Hemglobin=Male≥13mg/dL, Female≥12mg/dL; ‡Normal level of Prealbumin= ≥20mg/dL; §Normal level of Transferrin = ≥200mg/dL; AJCC=The American joint committee on cancer; UICC =The Union for international cancer control; GD=Gastroduodenostomy; EJ=Esophagojejunostomy
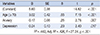
Table 3
Correlation between Psychological Variables and Nutritional Status at the 1 Month and 3~6 Months after Radical Gastrectomy
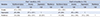
Table 4
Factors Associated with Nutritional Status on 1 Month after Radical Gastrectomy (N =107)
| Variables | B | SE | β | t | p |
|---|---|---|---|---|---|
| (Constant) | 5.60 | 0.38 | 14.82 | < .001 | |
| Age (≥ 70) | 3.02 | 0.42 | .55 | 7.15 | < .001 |
| Anxiety | 0.17 | 0.06 | .25 | 2.76 | .007 |
| Depression | 0.24 | 0.10 | .23 | 2.40 | .017 |
| R2=.442, Adj. R2=.426, F=27.24, p<.001 | |||||
References
1. National Cancer Information Center. Accessed September 23, 2015. http://www.ncc.re.kr.
2. Choi HS, Kim KO, Chun HJ, Keum B, Seo YS, Kim YS, et al. The efficacy of transdermal fentanyl for pain relief after endoscopic submucosal dissection: a prospective, randomised controlled trial. Dig Liver Dis. 2012; 44:925–929.

3. Rogers C. Postgastrectomy nutrition. Nutr Clin Pract. 2011; 26(2):126–136.
4. Zhuang CL, Wang SL, Huang DD, Pang WY, Lou N, Chen BC, et al. Risk factors for hospital readmission after radical gastrectomy for gastric cancer: a prospective study. PLoS ONE. 2015; 10(4):e0125572.

5. Terashima M, Tanabe K, Yoshida M, Kawahira H, Inada T, Okabe H, et al. Postgastrectomy syndrome assessment scale (PGSAS)-45 and changes in body weight are useful tools for evaluation of reconstruction methods following distal gastrectomy. Ann Surg Oncol. 2014; 21:S370–S3S8.

6. Kim JH, Choi JY. Postoperative changes in body weight, anxiety, depression, and quality of life after radical gastrectomy among patients with gastric cancer. Asian Oncol Nurs. 2014; 14(3):139–145.

7. Kong H, Oh KK, Yu W. Changes of quality of life after gastric cancer surgery. J Gastric Cancer. 2012; 12(3):194–200.

8. Yu EJ, Kang JH, Yoon S, Chung HK. Changes in nutritional status according to biochemical assay, body weight, and nutrient intake levels in gastrectomy patients. J Korean Diet Assoc. 2012; 18(1):16–29.

9. Oh CA, Choi MG, Noh JH, Sohn TS, Oh SJ, Bae JM, et al. Changes of the preoperative and postoperative nutritional statuses in patients with gastric cancer and assessment of the nutritional factors that are correlated with short-term postoperative complications. J Korean Gastric Cancer Assoc. 2010; 10(1):5–12.

10. Kang SC, Oh ST. The weight changes after gastrectomy in gastric cancer patients. J Korean Surg Soc. 1994; 47(2):209–215.
11. Yu W, Chung HY. Nutritional status after curative surgery in patients with gastric cancer comparison of total versus subtotal gastrectomy. J Korean Surg Soc. 2001; 60(3):297–301.
12. Kim JY, Park MS, Lee YH, Cho SJ, Yang HK. A study of dietary intakes and nutritional status after total gastrectomy of early gastric cancer patients. J Korean Diet Assoc. 2001; 7(1):72–79.
13. Yoon KY, Ahn SM, Lee KS, Choi KH. Nutritional assessment in gastric carcinoma. J Korean Surg Soc. 2005; 68(3):185–193.
14. Park YO, Yoon SY, Kang SS, Han SM, Kang EH. Nutritional status and dietary change after gastrectomy of gastric cancer patients. Nutr Res Pract. 2012; 17(1):101–108.

15. Maeda T, Onuoha FN, Munakata T. The effect of postoperative symptom experience, and personality and psychosocial factors on depression among postgastrectomy patients in Japan. Gastroenterol Nurs. 2006; 29(6):437–444.

16. Lim HS, Cho GS, Park YH, Kim SK. Comparison of quality of life and nutritional status in gastric cancer patients undergoing gastrectomies. Clin Nutr Res. 2015; 4(3):153–159.

17. Min JA, Yoon S, Lee CU, Chae JH, Lee C, Song KY, et al. Psychological resilience contributes to low emotional distress in cancer patients. Support Care Cancer. 2013; 21(9):2469–2476.

18. Lee JS, Cho MR, Lee GJ. Validation of the developed nutritional screening tool for hospital patients. Korean J Nutr. 2010; 43(2):189–196.

19. Bauer J, Capra S, Ferguson M. Use of the scored patient-generated subjective global assessment (PG-SGA) as a nutritional assessment tool in patients with cancer. Eur J Clin Nutr. 2002; 56(8):779–785.

20. Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans. Psychiatry Investig. 1999; 38(2):289–295.
21. Baek HS, Lee KU, Joo EJ, Lee MY, Choi KS. Reliability and validity of the Korean version of the connor-davidson resilience scale. Psychiatry Investig. 2010; 7(2):109–115.

22. Li QW, Li GC, Wang YN, Long ZW, Liu XW, Zhang Z. Association of nutrition with treatment compliance and toxicities in patients undergoing chemoradiation after gastrectomy. Zhonghua Wei Chang Wai Ke Za Zhi. 2013; 16(6):529–533.
23. Guigoz Y, Lauque S, Vellas BJ. Identifying the elderly at risk for malnutrition. The mini nutritional assessment. Clin Geriatr Med. 2002; 18(4):737–757.
24. Li H, Han X, Su L, Zhu W, Xu W, Li K, et al. Laparoscopic radical gastrectomy versus traditional open surgery in elderly patients with gastric cancer: benefits and complications. Mol Clin Oncol. 2014; 2(4):530–534.

25. Yang H, Cui M, Xing J, Yao Z, Zhang C, Zhang N, et al. Clinical efficacy of laparoscopy-assisted radical gastrectomy in elderly patients with gastric cancer. Zhonghua Wei Chang Wai Ke Za Zhi. 2015; 18(1):21–25.
26. Britton B, Clover K, Bateman L, Odelli C, Wenham K, Zeman A, et al. Baseline depression predicts malnutrition in head and neck cancer patients undergoing radiotherapy. Support Care Cancer. 2012; 20(2):335–342.

27. Daudt HM, Cosby C, Dennis DL, Payeur N, Nurullah R. Nutritional and psychosocial status of colorectal cancer patients referred to an outpatient oncology clinic. Support Care Cancer. 2012; 20(7):1417–1423.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download