Abstract
Purpose
The purpose of this study was to examine the relationships among sleep disturbance, depression, and quality of life in ovarian cancer during chemotherapy and to identify the influencing effect on quality of life.
Methods
A cross-sectional survey was conducted to measure sleep disturbance, depression and quality of life of 152 ovarian cancer patients between May and July, 2015. The data were analyzed with t-tests, ANOVA, post-hoc comparison (Scheffé), Pearson's correlation coefficients, and multiple regression analysis.
Results
The mean age of the participants was 54.2, and most of them were married. 61.8% of the patients were recurrent, and 50.0% had a performance status of ≤1. The prevalence of poor sleepers was 63.8%, and depression among patients was 52.6%. Sleep disturbance and depression were significantly negatively correlated with quality of life. As a result of stepwise multiple regression analysis, depression, sleep disturbance, monthly income and recurrence were discovered to account for 52.0% of variance. Depression and sleep disturbance were the most important influential factors.
Figures and Tables
Table 1
Demographic, Clinical, Psychological Characteristics in Patients with Ovarian Cancer (N =152)

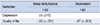
Table 2
Descriptive Statistics for Sleep Disturbance, Depression and Quality of Life (N =152)
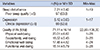
Table 3
Comparison of Sleep Disturbance, Depression, and Quality of Life according to Patients Characteristics (N =152)

Table 4
Correlation between Sleep Disturbance, Depression and Quality of Life (N =152)
| Variables | Sleep disturbance | Depression |
|---|---|---|
| r (p) | r (p) | |
| Depression | .19 (.017) | |
| Quality of life | - .33 (< .001) | - .67 (< .001) |
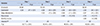
Table 5
Influencing Factors on Quality of Life
References
1. Sankaranarayanan R, Ferlay J. Worldwide burden of gynaecological cancer: the size of the problem. Best Pract Res Clin Obstet Gynaecol. 2006; 20(2):207–225.

2. Su Z, Graybill WS, Zhu Y. Detection and monitoring of ovarian cancer. Clin Chim Acta. 2013; 415:341–345.

3. American Cancer Society. Cancer facts & figures 2010. Adanca, GA: American Cancer Society;2010.
4. Gil KM, Gibbons HE, Jenison EL, Hopkins MP, von Gruenigen VE. Baseline characteristics influencing quality of life in women undergoing gynecologic oncology surgery. Health Qual Life Outcomes. 2007; 5:25.

5. Sela RA, Watanabe S, Nekolaichuk CL. Sleep disturbances in palliative cancer patients attending a pain and symptom control clinic. Palliat Support Care. 2005; 3(1):23–31.

6. Lindley C, Vasa S, Sawyer WT, Winer EP. Quality of life and preferences for treatment following systemic adjuvant therapy for early-stage breast cancer. J Clin Oncol. 1998; 16(4):1380–1387.

7. Clevenger L, Schrepf A, Degeest K, Bender D, Goodheart M, Ahmed A, et al. Sleep disturbance, distress, and quality of life in ovarian cancer patients during the first year after diagnosis. Cancer. 2013; 119(17):3234–3241.

8. Sandadi S, Frasure HE, Broderick MJ, Waggoner SE, Miller JA, von Gruenigen VE. The effect of sleep disturbance on quality of life in women with ovarian cancer. Gynecol Oncol. 2011; 123(2):351–355.

9. Palesh OG, Collie K, Batiuchok D, Tilston J, Koopman C, Perlis ML, et al. A longitudinal study of depression, pain, and stress as predictors of sleep disturbance among women with metastatic breast cancer. Biol Psychol. 2007; 75(1):37–44.

10. Porenoy RK, Thaler HT, Kornblith AB, Lepore M, Frledlander-Klar H, Coyle N, et al. Symptom prevalence, characteristics and distress in a cancer population. Qual Life Res. 1994; 3:183–189.

11. Nho JH, Kim SR, Kang GS, Kwon YS. Relationships among malnutrition, depression and quality of life in patients with gynecologic cancer receiving chemotherapy. Korean J Women Health Nurs. 2014; 20(2):117–125.

12. Suzuki N, Ninomiya M, Maruta S, Hosonuma S, Nishigaya Y, Kobayashi Y, et al. Psychological characteristics of Japanese gynecologic cancer patients after learning the diagnosis according to the hospital anxiety and depression scale. J Obstet Gynaecol Res. 2011; 37(7):800–808.

13. Lueboonthavatchai P. Prevalence and psychosocial factors of anxiety and depression in breast cancer patients. J Med Assoc Thai. 2007; 90(10):2164–2174.
14. Wenzel L, Huang HQ, Monk BJ, Rose PG, Cella D. Quality-of-life comparisons in a randomized trial of interval secondary cytoreduction in advanced ovarian carcinoma: a gynecologic oncology group study. J Clin Oncol. 2005; 23(24):5605–5612.

15. Fox SW, Lyon D. Symptom cluster and quality of life survivors of ovarian cancer. Cancer Nurs. 2007; 30:354–361.
16. von Gruenigen VE, Huang HQ, Gil KM, Gibbons HE, Monk BJ, Rose PG, et al. A comparison of quality-of-life domains and clinical factors inovarian cancer patients: a gynecologic oncology group study. J Pain Symptom Manage. 2010; 39(5):839–846.

17. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2):193–213.

18. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67(6):361–370.

19. Snaith RP. The Hospital Anxiety And Depression Scale. Health Qual Life Outcomes. 2003; 1:29.
20. Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993; 11(3):570–579.

21. Chen ML, Yu CT, Yang CH. Sleep disturbances and qualtiy of life in lung cancer patients undergoing chemotherapy. Lung Cancer. 2008; 62(3):391–400.

22. Manber R, Chambers AS. Insomnia and depression: a multifaceted interplay. Curr Psychiatry Rep. 2009; 11(6):437–442.

23. Barnes NM, Sharp T. A review of central 5-HT receptors and their function. Neuropharmacology. 1999; 38(8):1083–1152.

24. Kalueff AV, Nutt DJ. Role of GABA in anxiety and depression. Depress Anxiety. 2007; 24(7):495–517.

25. Lutgendorf SK, Weinrib AZ, Penedo F, Russell D, DeGeest K, Costanzo ES, et al. Interleukin-6, cortisol, and depressive symptoms in ovarian cancer patients. J Clin Oncol. 2008; 26(29):4820–4827.

26. Oh S, Heflin L, Meyerowitz BE, Desmond KA, Rowland JH, Ganz PA. Quality of life of breast cancer survivors after a recurrence: a follow-up study. Breast Cancer Res Treat. 2004; 87(1):45–47.

27. Price MA, Bell ML, Sommeijer DW, Friedlander M, Stockler MR, Defazio A, et al. Physical symptoms, coping styles and qualtiy of life in recurrent ovarian cancer: a prospective population-based study over the last year of life. Gynecol Oncol. 2013; 130(1):162–168.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download