Abstract
Purpose
The purpose of this study was to examine factors influencing resilience in breast cancer patients.
Methods
The data were collected using structured questionnaires from 106 breast cancer patients who are members of a self-help group. The data were analyzed using descriptive statistics, a t-test, ANOVA, Pearson correlation coefficients and stepwise multiple regression in SPSS WIN version 21.0.
Results
Resilience was significantly negatively correlated to depression and positively correlated to hope and family support. However, resilience was not significantly correlated to anxiety. In the regression analysis, factors influencing resilience were reported as hope, religion, lymph node metastasis, surgery side, and time since surgery, which explained 34.1% of the variation.
Conclusion
The resilience scores of women with breast cancer were higher when depression was lower, hope was higher, and greater family support. This means that reducing depression and increasing hope and family support are necessary when developing and implementing nursing interventions. The results of this study also show the importance of hope in explaining resilience in patients with breast cancer. Therefore, nurses should focus on encouraging hope when they develop programs in order to implement more effective interventions to improve breast cancer patients' resilience.
Figures and Tables
Table 1
Differences in Resilience by Participant Characteristics (N =106)

Table 2
Levels of Resilience, Anxiety, Depression, Hope, and Family Support in Participants (N =106)
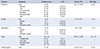
Table 3
Correlations among Resilience, Anxiety, Depression, Hope, and Family Support (N =106)
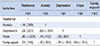
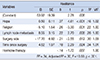
Table 4
Factors affecting Resilience (N =106)
References
1. GLOBOCAN 2012. Estimated cancer incidence, mortality and prevalence worldwide in 2012. Lyon: International Agency for Research on Cancer;Accessed September 1, 2014. http://globocan.iarc.fr/Pages/fact_sheets_cancer.
2. Korea Breast Cancer Society. Breast cancer factors & figures in Korea. Seoul: Korea Breast Cancer Society;2014. Accessed October, 2014. http://www.kbcs.or.kr/journal/file/2014_Breast_Cancer_Facts_and_Figures_updated.pdf.
3. Brem S, Kumar NB. Management of treatment-related symptoms in patients with breast cancer: current strategies and future directions. Clin J Oncol Nurs. 2011; 15:63–71.
4. Ryu YM, Yi MS. The factors influencing quality of life in women with breast cancer. Asian Oncol Nurs. 2013; 13(3):121–127.

5. Ahn JY. The influence of symptoms, uncertainty, family support on resilience in patients with breast cancer receiving chemotherapy [master's thesis]. Seoul: Seoul National Univ.;2014.
6. Kim JH. Resilience. Seoul: Seoul Wisdom house;2011.
7. Ha BY. Effects of resilience, post-traumatic stress disorder on the quality of life in patients with breast cancer [master's thesis]. Jinju: Gyeongsang National Univ.;2014.
8. Imm SJ. The factors influencing the resilience in stroke patients at home [master's thesis]. Seoul: Seoul National Univ.;2013.
9. Kwak SY, Byeon YS. Factors influencing resilience of patients with hematologic malignancy. Korean J Adult Nurs. 2013; 25(1):95–104.

12. Kim SR, Chung SJ, Shin NM, Shin HW, Kim MS, Lee SJ. Resilience in patients with parkinson's disease. J Korean Acad Adult Nurs. 2010; 22(1):60–69.
13. Kim JI, Byeon YS. A study on the factors affecting resilience in patients with colon cancer. Asian Oncol Nurs. 2013; 13(4):256–264.

14. Lee EK. A study on factors affeting cancer patients. J Korean Acad Soc Nurs Edu. 2007; 13(1):52–58.
15. Kim JY. The effect of hope and family support of depressed patients to their resilience [master's thesis]. Seoul: Ewha Women Univ.;2010.
16. Yang KS. The structural equation model on resilience of breast cancer patients receiving chemotherapy [dissertation]. Seoul: Ewha Women Univ.;2014.
17. Wagnild GM, Young HM. Development and psychometric evaluation of the resilience scale. J Nurs Meas. 1993; 1(2):165–178.
18. Wagnild GM. The Resilience Scale user's guide for the US English version of the Resilience Scale and the 14-Item Resilinece Scale (RS-14). Worden, MT: The Resilience Center;2010.
19. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67:361–370.

20. Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans: a comparison of normal, depressed and anxious groups. J Korean Neuropsychiatr Assoc. 1999; 38(2):289–296.
21. Nowotny ML. Assessment of hope in patient with cancer: Development of an instrument. Oncol Nurs Forum. 1989; 16:57–61.
22. Choi SS. A correlational study on spiritual wellbeing, hope and perceived health status of urban adults [dissertation]. Seoul: Yonsei Univ.;1990.
23. Cobb S. Social support as a moderator of life stress. Psychosomatic Medicine. 1976; 38(5):300–314.

24. Kang HS. An experimental study of the effects of reinforcement education for rehabilitation on hemiplegia patients' self-care activities [dissertation]. Seoul: Yonsei Univ.;1984.
25. Cho EA, Oh HE. Effects of laughter therapy on depression, quality of life, resilience and immune responses in breast cancer survivors. J Korean Acad Nurs. 2011; 41(3):285–293.

26. Kim HJ, Kim SH, Lee HK, Oh SE. Factors affecting symptom experiences of breast cancer patients: based on the theory of unpleasant symptoms. Asian Oncol Nurs. 2014; 14(1):7–14.

27. Tae YS, Kwon SH, Choi JH, Lee AR. Predictive factors for depression in breast cancer survivors. Asian Oncol Nurs. 2013; 13(3):113–120.

28. Tae YS, Kim MY. Influencing factors on hope among patients with breast cancer. Asian Oncol Nurs. 2009; 9(2):86–94.
29. Tae YS, Kim MY. Relationship betweem family support, perceived health status, and self-esteem in Korean women with breast cancer. Asian Oncol Nurs. 2011; 11(1):41–48.

30. Lee HS. A study of the influence of perceived family support by breast cancer patients in breast cancer treatment groups [master's thesis]. Daejeon: Chungnam National Univ.;2009.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download