Abstract
Purpose
The purpose of this study was to identify the levels of distress and quality of life in cancer patients receiving chemotherapy and to identify the relationship between distress and quality of life.
Methods
Data were collected during 2013 from 128 cancer patients receiving chemotherapy at a hospital located in Seoul, South Korea. Distress thermometer and problem list were used to measure distress, and the Functional Assessment Cancer Therapy-general questionnaire was used to measure quality of life. Descriptive statistics, t-tests, one-way ANOVA, the post-hoc Scheffé test, and Pearson's correlation coefficients were used to analyze the data.
Results
Among the 128 participants, 68 (53.1%) were male and the mean age was 52.55 years. Forty two (32.8%) were diagnosed with stage 4 and 73 (57.0%) were having recurrence or metastasis. The mean score for distress was 4.01 out of 10. Seventy four (57.8%) participants had a score of 4 or higher, indicating clinically significant distress. Emotional problems had the highest item mean among five domains. The mean score for quality of life was 68.51 ± 14.22 out of 108. Distress and quality of life were negatively correlated (r= -.52, p<.001).
Figures and Tables
Table 1
Difference in Distress and Quality of Life by Sociodemographic and Illness-related Characteristics (N=128)

Table 2
Levels of Distress (N=128)
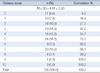
Table 3
Comparison of Problem List by Distress Group (N=128)

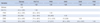
Table 4
Comparison of Quality of Life By Distress Group (N=128)
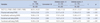
Table 5
Correlation between Distress and Quality of Life (N=128)
References
1. Statistics Korea. Cause of Death Statistics in 2011. Accessed January 19, 2015. http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1012.
2. National Cancer Information Center. 2012 National Cancer statistics. Accessed January 19, 2014. http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_040302000000.
3. Kyngäs H, Mikkonen R, Nousiainen EM, Rytilahti M, Seppänen P, Vaattovaara R, et al. Coping with the onset of cancer: coping strategies and resources of young people with cancer. Eur J Cancer Care. 2008; 10:6–11.

4. Zabora J, Brintzenhofeszoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001; 10:19–28.

5. National Comprehensive Cancer Network. Distress Management. Accessed December 20, 2014. http://www.nccn.org/professionals/physician_gls/pdf/distress.pdf.
6. Brown KW, Levy AR, Rosberger Z, Edgar L. Psychological distress and cancer survival: a follow-up 10 years after diagnosis. Psychosom Med. 2003; 65:636–643.
7. Carlson LE, Bultz BD. Efficacy and medical cost offset of psychosocial interventions in cancer care: making the case for economic analyses. Psychooncology. 2004; 13:837–849.

8. Strasser F, Sweeney C, Willey J, Benisch-Tolley S, Palmer JL, Bruera E. Impact of a half-day multidisciplinary symptom control and palliative care outpatient clinic in a comprehensive cancer center on recommendations, symptom intensity, and patient satisfaction: A retrospective descriptive study. J Pain Symptom Manage. 2004; 27:481–491.

9. Kvale EA, Murthy R, Taylor R, Lee JY, Nabors L. Distress and quality of life in primary high-grade brain tumor patients. Support Care Cancer. 2009; 17:793–799.

10. Kwon EJ, Yi MS. Distress and quality of Life in breast cancer survivors in Korea. Asian Oncol Nurs. 2012; 12:289–294.

11. Shim EJ, Shin JW, Jeon HJ, Hahm BJ. Distress and its correlates in Korean cancer patients: Pilot use of the distress thermometer and the problem list. Psychooncology. 2008; 17:548–555.

12. Bultz BD, Carlson LE. Emotional distress: the sixth vital sign in cancer care. J Clin Oncol. 2005; 23:6440–6441.

13. Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, Holland JC. Rapid screening for psychologic distress in men with prostate carcinoma. Cancer. 1998; 82:1904–1908.

14. Dabrowski M, Boucher K, Ward JH, Lovell MM, Sandre A, Bloch J, et al. Clinical experience with the NCCN distress thermometer in breast cancer patients. J Natl Compr Canc Netw. 2007; 5:104–111.

15. Jeong K, Heo JE, Tae YS. Relationship among distress, family support, and health promotion Behavior in breast cancer survivors. Asian Oncol Nurs. 2014; 14:146–154.

16. National Cancer Information Center. 2012 National Cancer statistics. Accessed January 19. 2015. http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_020403010000.
17. National Cancer Information Center. 2012 National Cancer statistics. Accessed January 19. 2015. http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_020403020000.
18. Kim SG. Managements of chemotherapy induced nausea and vomiting. Korean J Clin Oncol. 2012; 8:23–29.

19. Yang YH. Anorexia, nausea and vomiting, and food intake patterns in patients on chemotherapy. J Korean Acad Fundam Nurs. 2004; 11:177–185.
20. Kim GD, Jang HJ. Effects of pain, sleep disturbance, and fatigue on the quality of life in patients with pancreatic cancer undergoing chemotherapy. Asian Oncol Nurs. 2012; 2:117–124.

21. Youn HJ, Jung SH. Review Article: Care for alopecia during chemotherapy of cancer patients. Korean J Clin Oncol. 2011; 7:34–39.

22. Chung C, Kim MJ, Rhee MH, Do HG. Functional status and psychosocial adjustment in gynecologic cnacer patients receiving chemotherapy. Korean J Women Health Nurs. 2005; 11:58–66.

23. An HJ, Tae YS, Han YI. The relationship between spiritual health and uncertainty in cancer patients having chemotherapy. J Korean Oncol Nur. 2007; 7:107–118.
24. LEE JY, Choi S. Quality of life in gynecological cancer patients during chemotherapy. Korean J Women Health Nurs. 2007; 13:290–298.

25. Cella DF, Tulsky DS. Quality of life in cancer: definition, purpose, and method of measurement. Cancer Invest. 1993; 11:327–336.

26. Kim H, Yoo HJ, Kim YJ, Han OS, Lee KH, Lee JH, et al. Development and validation of Korean Functional Assessment Cancer Therapy-General (FACT-G). Korean J Clin Psychol. 2003; 22:215–229.
27. Janelsins MC, Kohli S, Mohile SG, Usuki K, Ahles TA, Morrow GR. An update on cancer-and chemotherapy-related cognitive dysfunction: Current status. Semin Oncol. 2011; 38:431–438.

28. Ahles TA, Saykin AJ, Furstenberg CT, Cole B, Mott LA, Skalla K, et al. Neuropsychologic impact of standard-dose systemic chemotherapy in long-term survivors of breast cancer and lymphoma. J Clin Oncol. 2002; 20:485–493.

29. Do YS. The relationships between self-care behavior and quality of life among female patients under the chemotherapy [master's thesis]. Seoul: Ewha Womans Univ.;2007.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download