Abstract
Purpose
The purpose of this study was to identify the relationship of stress, perception of occurrence risk of cancer and cancer preventive health behavior in three-shift nurses.
Methods
The participants of this study were 252 three shifts nurses working at three medium and small sized hospitals with 100 to 300 beds. Data were collected through a structured questionnaire from September to October 2014.
Results
The mean score for stress was 24.35±7.93. The mean score of perception for occurrence risk of cancer was 12.63±4.12 and cancer preventive health behavior was 58.07±8.87. Stress had a positive relationship with the perception of occurrence risk of cancer (r=.40, p<.001); the perception of occurrence risk of cancer had a positive relationship with the preventive health behavior against it (r=.31, p<.001); and stress had a positive relationship with preventive health behavior against it (r=.33, p<.001).
Conclusion
The findings show that participants stress levels were high and degrees of perceptions of occurrence risk and cancer preventive health behaviors were low. Significant correlations were found among these variables. On the basis of these findings, development of intervention is required to reduce stress and enhance the perception of occurrence risk of cancer and cancer preventive health behavior among three shifts nurses.
Figures and Tables
Table 1
Differences of Stress, Perception of Occurrence Risk of Cancer, and Cancer Preventive Health Behavior in General Characteristics of Subjects (N=254)
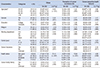
Table 2
The Degree of Stress, Perception of Occurrence Risk of Cancer, and Cancer Preventive Health Behavior of the Subjects (N=254)
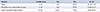
Table 3
Correlation between the Degree of Stress, Perception of Occurrence Risk of Cancer, and Cancer Preventive Health Behavior (N=254)

References
1. National Cancer Information Center. Cancer incidence. Accessed October 2, 2014. http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_040104000000.
2. International Agency for Research on Cancer. World Cancer Report 2013. Accessed July 10, 2014. http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_010101020000.
3. Srinivasan V, Maestroni GJM, Cardinali DP, Esquifino AI, Pandi-Perumal SR, Miller SC. Melatonin, immune function and aging. Immune Ageing. 2005; 2:17.

4. Schwartzbaum J, Ahlbom A, Feychting M. Cohort study of cancer risk among male and female shift workers. Scand J Work Environ Health. 2007; 33:336–343.

5. Viswanathan AN, Schernhammer ES. Circulating melatonin and the risk of breast and endometrial cancer in women. Cancer Letter. 2009; 281:1–7.

6. Schernhammer ES, Kroenke CH, Laden F, Hankinson SE. Night work and risk of breast cancer. Epidemiology. 2006; 17:108–111.

7. Kirkcaldy BD, Martin T. Job stress and satisfaction among nurses: individual differences. Stress Med. 2000; 16:77–89.

8. Kim MJ, Han SS. Comparison of job satisfaction, commitment to organization, nursing organization culture and job experience between national/public hospital nurses and private hospital nurses. J East West Nurs Res. 2007; 13(1):22–30.
10. Kim CH. Stress mainly caused inflammation and cancer development: optimal condition to reduce stress. J Korean Acad Nurs. 2004; 43(2):10–11.
11. Kim JH, Hyun MY, Kim YS, Kim JS, Nam SO, Song MS, et al. Psychosocial well-being, health perception and behavior among clinical nurses. J Korean Acad Nurs Adm. 2010; 16(1):26–36.

12. Rosenstock JM. The health belief model: explaining health behavior thought expectance. In health behavior & health education theory research & practice. San Francisco, CA: Jossey-Bass Publishers;1990.
13. Park EH. Influence of health beliefs on preventive health behaviors for cancer among middle aged women [Master's thesis]. Pusan: Inje Univ.;2009.
14. Chang SJ. Stress standardization of health statistics collection and measurement of health statistics data. Seoul: Korean Society for Preventive Medicine;2000.
15. Ryu EJ, Choi SY, Kang YS. Study of working women's psychosocial stress. J Korean Data Anal Soc. 2006; 8(5):1793–1806.
16. Yang YH. Relationships between knowledge about early detection, cancer risk perception and cancer screening tests in the general public aged 40 and over. Asian Oncol Nurs. 2012; 12(1):52–60.

17. Suh SR, Chung BY, So HS, Tae YS. A study to advance the development of educational programs for the early detection and prevention of the five major cancer in Korea. J Korean Acad Adult Nurs. 1998; 10:268–280.
18. Lee SH, Yoo IY. A study of psychosocial distress, intention to quit and nursing performance in general ward nurses. Korean J Occup Health Nurs. 2010; 19(2):236–245.
19. Han MA, Kim KS, Park J, Ryu SY, Kang MG. Psychosocial stress levels and related factors in some rural residents. J Agric Med Community Health. 2008; 33(1):46–58.

20. Lee JH, Cho WH, Chang SJ, Kim YH. The effects of work and psychosocial stress on job satisfaction, organizational commitment, and leaving intention in general hospital female office workers. Korean J Hosp Manage. 2012; 17(2):1–22.
21. Choi HS. A study on the relationship of shift work to stress in nurses [Master's thesis]. Suncheon: Suncheon Univ.;2008.
22. Kang JY. Spousal support and job satisfaction of married nurses' influence on their role conflict [Master's thesis]. Seoul: Sungkyunkwan Univ.;2013.
23. Ministry of Employment and Labor. Occupational safety and health act. Accessed July 26, 2014. http//www.moel.go.kr.
24. Ko KM. The impact of health campaigns on the public's awareness & behavior regarding cervical cancer. Seoul: Ewha Womans Univ.;2012.
25. Jeong BL, Byeon HS, Kim GH. Knowledge of cancer by female college student behaviour of cancer prevention. J Kyungpook Nurs Sci. 2010; 14(1):45–59.
26. Jun EM, Cho DS. The relationship of symptoms of stress, cancer prevention behavior and the quality of life in women. Korean J Women Health Nurs. 2005; 11(2):156–162.

27. Kim IJ, Kim SH. Relationships between knowledge, attitude and preventive health behavior about cancer in university students. Asian Oncol Nurs. 2012; 12(1):44–51.

28. Jeon EY, Choi SR, Han SS. Influencing factors on health-promotion lifestyle of nurses. J East West Nurs Res. 2007; 13(1):40–47.
29. Han AK, Joe DS. A study on physiological parameters, health perception, and health behavior of adults in kyungi province area. J Korean Acad Nurs. 2001; 31(4):631–640.

30. Noh HS. Impact of family cancer history on preventive health behaviors [master's thesis]. Seoul: Seoul National Univ.;2007.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download