Abstract
Purpose
The purpose of this study was to determine the prevalence of distress and to investigate the related problems in breast cancer patients at the end of primary treatment.
Methods
A sample of 118 participants was recruited among outpatients who had successfully completed primary treatment of breast cancer. Data were collected between July, 2013 and October, 2014 using the Distress Thermometer (DT) scale and problem lists. Descriptive statistics and logistic regression analysis were used to analyze data.
Results
Among the 118 patients that participated in this study, 34 patients (28.8%) suffered from elevated distress using the previously validated cut point ≥4 for the DT. Problems most frequently encountered were fatigue (68.8%), worry (59.3%), appearance (51.7%) and memory/concentration (48.3%). Multivariate logistic regression analysis revealed that depression (OR=9.55), worry (OR=8.34), fatigue (OR=8.19) and age (OR=1.14) were independent predictors for elevated distress scores.
Figures and Tables
Table 1
Demographic and Treatment-Related Factors of Patients in Mild Distress Group and Moderate-Severe Distress Group
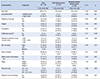
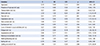
Table 2
Problem Lists in Mild Distress Group and Moderate-Severe Distress Group

Table 3
Influencing Factors of Moderate-Severe Distress (N=118)
References
1. Korean breast cancer society. Accessed May 15, 2014. http://www.kbcs.or.kr.
2. Alfano CM, Rowland JH. Recovery issues in cancer survivorship: a new challenge for supportive care. Cancer J. 2006; 12(5):432–443.
3. National Comprehensive Cancer Network. Distress Thermometer for Patients (v.1.2013). Accessed July 26, 2013. http://www.nccn.org/international/international_adaptations.aspx.
4. Costanzo ES, Lutgendorf SK, Mattes ML, Trehan S, Robinson CB, Tewfik F, et al. Adjusting to life after treatment: distress and quality of life following treatment for breast cancer. Br J Cancer. 2007; 97(12):1625–1631.

5. Jeong K, Heo J, Tae Y. Relationships among distress, family support, and health promotion behavior in breast cancer survivors. Asian Oncol Nurs. 2014; 14(3):146–154.

6. Hansen JA, Feuerstein M, Calvio LC, Olsen CH. Breast cancer survivors at work. J Occup Environ Med. 2008; 50(7):777–784.

7. Shapiro CL, Recht A. Side effects of adjuvant treatment of breast cancer. N Engl J Med. 2001; 344(26):1997–2008.

8. Thewes B, Butow P, Girgis A, Pendlebury S. The psychosocial needs of breast cancer survivors: a qualitative study of the shared and unique needs of younger versus older survivors. Psychooncology. 2004; 13(3):177–189.

9. VanHoose L, Black LL, Doty K, Sabata D, Twumasi-Ankrah P, Taylor S, et al. An analysis of the distress thermometer problem list and distress in patients with cancer. Support Care Cancer. 2015; 23(5):1225–1232.

10. Arndt V, Stegmaier C, Ziegler H, Brenner H. A population-based study of the impact of specific symptoms on quality of life in women with breast cancer 1 year after diagnosis. Cancer. 2006; 107(10):2496–2503.

11. Deimling GT, Bowman KF, Wagner LJ. The effects of cancer-related pain and fatigue on functioning of older adult, long-term cancer survivors. Cancer Nurs. 2007; 30(6):421–433.

12. Lam WW, Shing YT, Bonanno GA, Mancini AD, Fielding R. Distress trajectories at the first year diagnosis of breast cancer in relation to 6 years survivorship. Psychooncology. 2012; 21(1):90–99.

13. Ploos van Amstel FK, Berg SW, Laarhoven HW, Gielissen MF, Prins JB, Ottevanger PB. Distress screening remains important during follow-up after primary breast cancer treatment. Support Care Cancer. 2013; 21(8):2107–2115.

14. Stanton AL. What happens now? Psychosocial care for cancer survivors after medical treatment completion. J Clin Oncol. 2012; 30(11):1215–1220.

15. Head BA, Schapmire TJ, Keeney CE, Deck SM, Studts JL, Hermann CP, et al. Use of the distress thermometer to discern clinically relevant quality of life differences in women with breast cancer. Qual Life Res. 2012; 21(2):215–223.

16. Hegel MT, Moore CP, Collins ED, Kearing S, Gillock KL, Riggs RL, et al. Distress, psychiatric syndromes, and impairment of function in women with newly diagnosed breast cancer. Cancer. 2006; 107(12):2924–2931.

17. Liu JE, Wang HY, Wang ML, Su YL, Wang PL. Posttraumatic growth and psychological distress in Chinese early-stage breast cancer survivors: a longitudinal study. Psychooncology. 2014; 23(4):437–443.

18. Kwon EJ, Yi M. Distress and quality of life in breast cancer survivors in Korea. Asian Oncol Nurs. 2012; 12(4):289–296.

19. Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry. 2008; 30(2):112–126.

20. Lester J, Crosthwaite K, Stout R, Jones RN, Holloman C, Shapiro C, et al. Women with breast cancer: self-reported distress in early survivorship. Oncol Nurs Forum. 2015; 42(1):E17–E23.

21. Fiszer C, Dolbeault S, Sultan S, Brédart A. Prevalence, intensity, and predictors of the supportive care needs of women diagnosed with breast cancer: a systematic review. Psychooncology. 2014; 23(4):361–374.

22. Park JS, Lee HR. Comparison of distress and body Image according to the stages of cancer survivorship in gynecological cancer patients. Asian Oncol Nurs. 2014; 14(1):15–22.

23. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009; 41(4):1149–1160.

24. Wang GL, Hsu SH, Feng AC, Chiu CY, Shen JF, Lin YJ, et al. The HADS and the DT for screening psychosocial distress of cancer patients in Taiwan. Psychooncology. 2011; 20(6):639–646.

25. Shim EJ, Shin YW, Jeon HJ, Hahm BJ. Distress and its correlates in Korean cancer patients: pilot use of the distress thermometer and the problem list. Psychooncology. 2008; 17(6):548–555.

26. Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer. 2009; 115(22):5349–5361.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download