Abstract
Purpose
This descriptive study was to identify predictors of follow-up screening among Korean women with low-grade abnormal Papanicolaou smears.
Methods
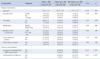
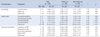
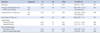
This study was conducted among 158 eligible women with atypical squamous cells of undetermined significance (ASC-US) or low-grade squamous intraepithelial lesion (LSIL) on Pap smear tests from the out-patient department at an academic hospital. Data were collected on self-report questionnaires including demographics, beliefs, knowledge and psychosocial distress. Multivariate logistic regression was used to identify independent factors association with follow-up.
Results
Of the 158 women with abnormal Pap smear results, 60.8% completed the recommended follow-up within 6months, and 39.2% did not. In multivariate analysis, attendance of follow-up was significantly increased with good explanation from health care providers (OR=4.89, 95% CI=1.96-12.13), having intention to follow-up (OR=7.96, 95% CI=1.88-33.65), increasing perceived benefit (OR=1.91, 95% CI=1.21-2.99) and decreasing perceived barriers (OR=1.41, 95% C I=1.13-1.74).
Conclusion
Despite increasing rates of cervical cancer screening, pervasive problems in the adherence of follow-up of abnormal findings continue. We suggest more intensive interventions including good explanations by health care providers, educational programs for follow-up care and individualized implementations depending on barriers.
Figures and Tables
References
1. National Cancer Information Center. Cancer statistics 2013. Accessed November 13, 2013. http://www.cancer.go.kr/mbs/cancer/jsp/album/gallery.jsp.
3. Saslow D, Solomon D, Lawson HW, Killackey M, Kukasingam SL, Cain JM, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology and American Society for clinical pathology screening guidelines for the prevention and early detection of cervical cancer. J Low Genit Tract Dis. 2012; 16(3):175–204.

4. Hong EK, Nam JH, Park MH. The Bethedsa system 2001 workshop report. Korean J Cytopathol. 2001; 12(1):1–15.
5. Apgar BS, Zoschnick L, Wright TC. The 2001 Bethesda system terminology. Am Fam Physician. 2003; 68(10):1992–1998.
6. Bentley J, Halifax NS. Colposcopic management of abnormal cervical cytology and histology. J Obstet Gynaecol Can. 2012; 34(12):1188–1202.

7. Kaplan C, Bastani R, Belin T, Marcus A, Nasseri K, Hu M. Improving follow-up after an abnormal Pap smear: results from a quasi-experimental intervention study. J Womens Health Gend Based Med. 2000; 9(7):779–790.

8. Yabroff K, Washington K, Leader A, Mandelblatt J. Is the promise of cancer-screening programs being compromised? Quality of follow-up care after abnormal screening results. Med Care Res Rev. 2003; 60(3):294–331.

9. El-Hammasi K, Samir O, Kettaneh S, Al-Fadli A, Thalib L. Use of and attitudes and knowledge about Pap smears among women in Kuwait. J Womens Health (Larchmt). 2009; 18(11):1825–1832.

10. Urritia MT. Development and testing of a questionnaire: beliefs about cervical cancer and pap test in Chilean women [dissertation]. Miami Univ.;2009.
11. Lee Mortensen G, Adeler A. Qualitative study of women's anxiety and information needs after a diagnosis of cervical dysplasia. Z Gesundh Wiss. 2010; 18(5):473–482.

12. Bertram C, Magnussen L. Informational needs and the experiences of women with abnormal papanicolaou smears. J Am Acad Nurse Pract. 2008; 20(9):455–462.

13. Percac-Lima S, Aldrich L, Gamba G, bearse A, Atlas SJ. Barriers to follow-up of abnormal pap smear in Latina women referred for colposcopy. J Gen Intern Med. 2010; 25(11):1198–1204.

14. Lee EJ, Park JS. Predictors associated withr repeated papanicolaou smear for cervical cancer screening. Asian Oncol Nurs. 2013; 13(1):28–36.

15. Cho IS, Park YS. A study on regular cervical cancer screening behavior among middle-aged women. J Korean Acad Nurs. 2004; 34(1):141–149.

16. Jeong IS, Kim SH, Kim YS. Relataed factors with cervical cancer screening and repeated screening. J Korean Soc Matern Child Health. 2004; 8(2):185–198.
17. Rojas C, Zhou MK, Khamis HJ, Amesse L. Analysis of patterns of patient compliance after an abnormal pap smear result: the Influence of demographic characteristics on patient compliance. J Low Genit Tract Dis. 2013; 17(3):298–302. [accessed on 13 May 2013].

18. Elit L, Saskin R, Raut R, Elliott L, Murphy J, Marrett L. Sociodemgraphic factors associated with cervical cancer screening coverage and follow-up of high grade abnormal results in a population-based cohort. Gynecol Oncol. 2013; 128:95–100.

19. Sharp L, Cotton S, Thornton A, Gray N, Cruickshank M, Whynes D, et al. Who defaults from colposcopy? A multi-centre, population-base prospective cohort study of predictors of non-attendance for follow-up among women with low-grade abnormal cervical cytology. Eur J Obstet Gynecol Reprod Biol. 2012; 165(2):318–325.

20. Monsonego J, Cortes J, Silva DP, Jorge AF, Klein P. Psychological impact, support and information needs for women with an abnormal pap smear: comparative results of a questionnaire in three European countries. BMC Womens Health. 2011; 11:18.

21. Lee EJ, Park JS. Knowledge about cervical cancer, health beliefs and human papillomavirus vaccination rate in female university students. J Korean Oncol Nurs. 2011; 11(1):65–73.

22. National Cancer Center. National cancer screening findings and standard recommendation. Accessed May 6, 2013. http://www.cancer.go.kr.
23. Bennetts A, lrwig L, Oldenburg B, Simpson JM, Mock P, Allison B, et al. PEAPS-Q: a questionnaire to measure the psychosocial effects of having an abnormal pap smear. J Clin Epidemiol. 1995; 48(10):1235–1243.

24. Jang JH, Kim SH, Jang SH, An TS, Won JC, Jeong GU, et al. PAP Smear: analysis of 10 years results (1992-2001). Obstet Gynecol Sci. 2003; 46(9):1714–1719.
25. Oh EJ, Lee YE, Lee SO. Cervical cancer screening behavior and related factors among married women. J Korean Soc Matern Child Health. 2010; 14(1):12–23.

26. Bednarczyk RA, Butsashvili M, Kamkamidze G, Kajaia M, McNutt LA. Attitudes and knowledge of Georgian physicians regarding cervical cancer prevention 2010. Int J Gynaecol Obstet. 2013; 121(3):224–228.

27. Oranratanaphan S, Amatyakul P, Iramaneerat K, Srithipayawan S. Knowledge, attitudes and practices about the pap smear among medical workers in Naresuan university Hospital, Thailand. Asian Pac J Cancer Prev. 2010; 11(6):1727–1730.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download