Abstract
Purpose
The purpose of this study was to identify the factors affecting symptom experiences of breast cancer patients.
Methods
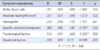
A cross-sectional descriptive study was conducted with based on the Unpleasant symptom Theory. Sixty breast cancer patients were recruited. We measured their symptom experiences, physiologic factors (immune system function and specific perceived symptoms), psychological factors (depression and anxiety), and situational factors (family support). After obtaining permission from the IRB, data were collected from self-report questionnaires and electronic medical records from a single cancer center. Descriptive statistics, t-test, one-way ANOVA, correlations and multiple regressions were used to analyze the data.
Results
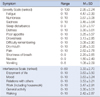
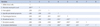
The most frequent and severe symptoms were fatigue (4.47±2.99), numbness or tingling (3.67±3.08) and sadness (3.45±3.64). Symptom experiences were significantly positively correlated with psychological factors (r=.603, p<.01) and physical symptoms (r=.384, p<.01). Symptom experiences and situational factors (r=.302, p<.05) were had a significantly negative correlation. The factor that had the most impact on symptom experiences were psychological factors, followed by perceived physical symptoms. The regression model explained 44.8% of the variances.
Figures and Tables
References
1. Statistical Korea, Korean Statistical Information Service. Accessed December 19, 2013. http://kosis.kr/statisticsList/statisticsList_01List.jsp?vwcd=MT_ZTITLE&parentId=D.
2. Kim JY. Risk factors affecting the onset of breast cancer [dissertation]. Seoul: Chung-ang Univ.;2008.
3. Badger T, Braden C, Mishel M. Depression burden, self-help interventions, and side effect experience in women receiving treatment for breast cancer. Oncol Nurs Forum. 2001; 28(3):567–574.
4. Dodd M, Janson S, Facione N, Faucett J, Froelicher ES, Humphreys J, et al. Advancing the science of symptom management. J Adv Nurs. 2001; 33(5):668–676.

5. Haworth SK, Dluhy NM. Holistic symptom management: modelling the interaction phase. J Adv Nurs. 2001; 36(2):302–310.

6. Larson PJ, Uchinuno A, Izumi S, Kawano A, Takemoto A, Shigeno M, et al. An integrated approach to symptom management. Nurs Health Sci. 1999; 1(4):203–210.

7. Teel CS, Meek P, McNamara AM, Watson L. Perspectives unifying symptom interpretation. Image J Nurs Sch. 1997; 29(2):175–181.

8. Lenz ER, Pugh LC, Milligan RA, Gift A, Suppe F. The middle-range theory of unpleasant symptoms: an update. ANS Adv Nurs Sci. 1997; 19(3):14–27.

9. Chung BY, Xu Y, Lee EH. Symptom experience, mood disturbance, & social support in breast cancer patients undergoing radiotherapy. J Korean Oncol Nurs. 2006; 6(2):172–180.
10. Lee EH, Yae CB, Park BH, Hong CK. Relationships of mood disturbance and social support to symptom experience in Korean women with breast cancer. J Pain Symptom Manage. 2004; 27(5):425–433.

11. Lee EH. Relationships of mood disturbance, symptom experience, and attentional function in women with breast cancer based upon the theory of unpleasant symptoms. J Korean Acad Nurs. 2005; 35(4):728–736.

12. So WK, Leung DY, Ho SS, Lai ET, Sit JW, Chan CW. Associations between social support, prevalent symptoms and health-related quality of life in Chinese women undergoing treatment for breast cancer: A cross-sectional study using structural equation modelling. Eur J Oncol Nurs. 2013; 17(4):442–448.

13. Cleeland CS, Mendoza TR, Wang XS, Chou C, Harle MT, Morrissey M, et al. Assessing symptom distress in cancer patients: the M.D. Anderson Symptom Inventory. Cancer. 2000; 89(7):1634–1646.
14. Yun YH, Mendoza TR, Kang IO, You CH, Roh JW, Lee CG, et al. Validation study of the korean version of the M.D. Anderson symptom inventory. J Pain Symptom Manage. 2006; 31(4):345–352.

15. Lee MH. An effect of rhythmic movement therapy for adaptation state in mastectomy patients. J Korean Acad Fundam Nurs. 1995; 2(1):67–85.
16. Yoo YS. Effects of aquatic exercise program on the shoulder joint function, physical symptom and quality of life in postmastectomy patients. J Korea Community Health Nurs Acad Soc. 1999; 13(2):101–114.
17. Lee JE. Symptom experiences according to chemotherapy cycle in patients with breast cancer [dissertation]. Seoul: Yonsei Univ.;2005.
18. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67(6):361–370.

19. Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans: a comparison of normal, depressed and anxious groups. J Korean Neuropsychiatr Assoc. 1999; 38(2):289–296.
21. Kang HS. (An)Experimental study of the effects of reinforcement education for rehabilitation on hemiplegia patients' self-care activities [dissertation]. Seoul: Yonsei Univ.;1984.
22. Terri SA, Ibrahima G, Tito RM, Jeffrey SW, Mark RG, Melissa LT, et al. Clinical utility of the MDASI-BT in patients with brain metastases. J Pain Symptom Manage. 2009; 37(3):331–340.

23. Prigozin A, Uziely B, Musgrave CF. The relationship between symptom severity and symptom interference, education, age, marital status, and type of chemotherapy treatment in Israeli women with early-stage breast cancer. Oncol Nurs Forum. 2010; 37(6):E411–E418.

24. Hwang HS. Shoulder joint function, lymphedema, physical symptoms and functional status after mastectomy : comparison of sentinel lymph node biopsy and axillary lymph node dissection [dissertation]. Seoul: Yonsei Univ.;2003.
25. Jang S. Effects of meditation program on power, anxiety, depression and quality of life in women with breast cancer. J Korean Acad Psychiatr Ment Health Nurs. 2013; 22(3):205–215.

26. Park EY. Development and effectiveness of expressive writing program for women with breast cancer in korea. J Korean Acad Nurs. 2012; 42(2):269–279.

27. Ho SS, So WK, Leung DY, Lai ET, Chan CW. Anxiety, depression and quality of life in Chinese women with breast cancer during and after treatment: a comparative evaluation. Eur J Oncol Nurs. 2013; 17(6):877–882.

28. Lee IS. The quality of life analysis in breast cancer patients by family support and depression extent [dissertation]. Seoul: Danguk Univ.;2000.
29. Park SY. (The) change of quality of life, depression and family support according to the process of treatment in breast cancer patients [dissertation]. Seoul: Chungnam Univ.;2004.
30. Choi YH, Kim NS, Byun YS. A study of womanhood and caring. Korean Nurse. 1991; 30(5):75–81.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download