Abstract
Purpose
To assess the effectiveness of a care map for a fast-track discharge program after colorectal cancer surgery.
Methods
Ninety-nine patients who underwent colorectal surgery were retrospectively analyzed: 45 patients who were placed in a conventional program (January 3 to March 13, 2013) and 44 patients who were placed in a fast-track program using the care map (July 26 to September 24, 2014). Patients in the fast-track program started eating on postoperative day 1, while those in the conventional program started eating on post-operative day 2. complications, and pain were compared between the two groups.
Results
A slight decrease in the average duration of hospitalization was observed for the fast-track group (5.31±0.98 days) compared to the conventional group (5.38±2.80 days), although this difference was not statistically significant. All other outcomes for the fast-track group were scored as 0. Furthermore, there was no statistically significant differences between pain, narcotics administration, and non-narcotic analgesics (aside from patient-controlled analgesia).
As interest in cost reduction and early discharge has grown, due to increased medical costs and the introduction of the Diagnosis-Related Group system, the concept of a fast-track program has emerged in an effort to reduce the duration of hospital stays. Fast-track discharge, which is also known as "enhanced recovery after surgery," can easily be misunderstood as simply meaning early oral intake and early discharge. However, the fast-track discharge concept includes a wide variety of factors, such as reduced surgical stress responses, increased recovery speed, reduced complication rates, and cost reduction without compromising patient safety.1) The concept also encompasses various strategies to enhance patient status and recovery, in an effort to achieve faster discharge while reducing the likelihood of surgical complications or readmission.2) Regarding the specific steps, fast-track discharge consists of pre-operative education, a meal after surgery, and pain control. The pre-operative education increases the patients' commitment to recovery by reducing their fears and enhancing their understanding of the surgery, as the nurses and doctors describe the processes from admission to discharge. Another feature of fast-track discharge is minimizing the fasting period before and after surgery, which is based on the theory that resuming meals early after surgery hastens the recovery of physical rhythms.
In this context, communication should involve the sharing of information regarding the overall process with the nursing team, and effective post-surgical explanations for the patients; these steps can increase the rate of postoperative recovery and facilitate the patient's return to everyday life. With the introduction of a fast-track program at our institution, our surgical team has developed a care map that covers the entire fast-track process, from personalized pre-operative education to postoperative care and education. In our institution, surgical nurses are responsible for various tasks, including pre- and post-operative care, drug administration and intravenous administration management, transfusion care, oxygen therapy, communicating with patients and caregivers, and telephone counseling. Therefore, we aimed to increase their work efficiency by developing and applying a planned and standardized care map for fast-track patients. Care maps (also known as critical pathways) have tremendous appeal, owing to their multidisciplinary methods, focus on processes, and attention to patient outcomes; these maps have been adopted by many large hospitals worldwide.3) Therefore, we hypothesized that if a standardized fast-track program was created for our nurses, via a customized and structured description of the course of treatment and nursing requirements, adherence to patient treatment could be increased. The aim of this study was to establish a care map for the fast-track discharge of patients who were admitted for treatment of colon diseases, and to compare outcomes between the care map intervention group and patients who underwent the conventional treatment.
The fast-track concept was used in most elective colon resections, which were either open or laparoscopic procedures. This concept included the following steps: verbal and written pre-operative information, no bowel preparation, pre-operative oral hydration, oral intake as soon as possible post-operatively, patient mobilization for at least 2 hours on the day of surgery, and further mobilization on the first full postoperative day, as previously reported.1) Prior to the operation, the operative methods and recovery program were explained to the patient, and consent was obtained.
The patients were hospitalized 2 days before the operation, and underwent intestinal irrigation, pre-operation treatment administration, and nasogastric tube insertion to reduce.
Exercise was encouraged as much as possible, starting on the operation day, and the urinary catheter was removed immediately after the operation in the operating room. Preventive antibiotics were administered for 2 days, and every patient received intravenous patient-control anesthesia. In cases where the patient complained of severe pain, narcotic or non-narcotic analgesics were selected, according to the patient's state.
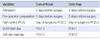
The care map was specifically designed to focus on each patient's motivation and their prerequisites for rehabilitation and was collaboratively developed by an experienced multidisciplinary team that included surgeons and nurses. Each patient's entire hospitalization process could be determined by a glance at the care map, which included information on care and treatment, medication, diet, activity, laboratory tests, and the patient education that was to be provided on the day of admission, before surgery, on the day of surgery, after surgery, and on the day of discharge (Table 1).
The subjects for this study were extracted via convenience sampling from an accessible population of patients who underwent colorectal cancer surgery at a university hospital (Seoul, South Korea) from January 2013 to September 2014. Among this population, 173 patients were not placed in the fast-track program (January to March, 2013), and 230 patients were placed in the fast-track program (July to September, 2014). The fast-track patients were selected 3 months after receiving ethical approval from our institutional review board, and their medical records were retrospectively examined. This study was designed to compared the averages of two independent samples, and a minimum sample size of 30 cases was required (based on the assumption of normal distribution).4)
The exclusion criteria were patients with complicated disease; patients who underwent re-operation; cases with complications related to an existing surgical site; patients with fever, pneumonia, or intestinal obstruction; and cases that were transferred to general surgery wards from non-general surgery wards. Based on these criteria, 45 of the 173 non-fast-track patients and 44 of the 230 fast-track patients were selected.
Gastrointestinal activity was defined as activity that occurred as a digestive process of intestines until the digested food had passed into the large intestine. In this study, we evaluated the recovery of gastrointestinal activity using the emptying time of feces and gas, which was considered to indicate gastrointestinal activity recovery after general anesthesia.
The gas emptying time referred to the time at which the patient subjectively perceived the first episode of flatulence after the operation, and emptying time referred to the time at which feces were first excreted after the operation.
Despite the evidence regarding the benefits of epidural catheter use, various factors make their use unpopular at some centers; therefore, alternative postoperative pain control methods are used. For example, intravenous narcotics delivered via patient-controlled analgesia (PCA) devices have gained widespread acceptance. In this context, PCA use for fast-track colon surgery has generally focused on reducing the patient's pain and the related effects on ileus when using a minimally invasive approach.5)
Various adverse effects are associated with colorectal surgery, including nausea, vomiting, enteroplagia, infection, changes in the immune system, decreased cardio-pulmonary function, coagulopathy, changes in fluid control, sleep disorders, and fatigue. Postoperative ileus was defined disruption of the normal ability of the gastrointestinal tract or the need for a nasogastric tube (L-tube) reinsertion after starting oral diet, in the absence of mechanical bowel obstruction. Postoperative hospital stay during the primary admission was defined as the number of days spent in the hospital after surgery. In addition, rehospitalization was defined as a subsequent hospitalization (within 30 days of discharge) for treatment of the complications stated above.
Patients were discharged after they did not experience discomfort during the postoperative meal and emptying occurred, when pain could be controlled using oral pain medication, when fever was confirmed to be absent, and when direct communication with the hospital was possible after the discharge. We also directed the patients to contact or visit the hospital immediately if they experienced an evacuation disorder, stomachache, or fever after discharge.
The data were analyzed using SPSS 17.0 for Windows (SPSS, Chicago, IL) and reported using descriptive statistics, including the percentage, mean, and standard deviation and t-test. Clinical and pathologic variables were analyzed using the t-test, χ2 test, or the Wilcoxon rank-sum test, depending on the distribution of the variables.
This study's design was reviewed and approved (prior to the study initiation) by the institutional review board of the Seoul National University College of Medicine/Seoul National University Hospital, Seoul, Korea (1410-069-618). In addition, to protect the patients' right to privacy, all data were anonymized by removing identifying information (e.g., name, address, phone number, and disease code) from the case report forms, which were identified using serial numbers.
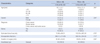
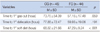
The subjects' demographic characteristics and clinical data are shown inTable 2. The average age of the 45 subjects in the conventional group was 62.1 years (range, 36~79 years), and that of the 44 subjects in the fast-track group was 59.9 years (range, 34~85 years). In the control group, 33 (73.3%) were men, and 12 (26.7%) patients were women, compared to 27 (61.4%) men and 17 (38.6%) women in the fast-track group. The time to soft diet intake was shorter in the fast-track group compared to that in the conventional care group (Table 3), although no differences were observed in the time to flatulence and first defecation.
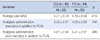
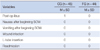
In addition, no differences were observed in the postoperative pain scores (which were assessed using a visual analog scale), analgesic administration, or narcotic analgesic administration (via PCA) (Table 4). Furthermore, there were no differences in the complication rates for postoperative ileus, nausea, vomiting, wound infection, L-tube insertion, and 30-day readmission (Table 5). Postoperative ileus, nausea, vomiting, wound infection, and L-tube insertion did not occur in the fast-track group, and no readmissions were observed for either group during the 30 days after surgery.
Given the recent introduction of a fast-track program for colorectal surgery, this study used a care map to examine the importance of communication between doctors, nurses, and patients regarding the patients' information, care, and treatment. The important aspects of this study includes the successful implementation of a fast-track program during the recovery process after colorectal surgery; the coordinated approach of surgeons, nurses, and the corresponding care support units; and the care map that included information for patient education.
In this study, a care map was developed and implemented using a fast-track program for colorectal surgery patients. Interestingly, the outcomes were similar to those of the conventional surgery group, and similar results were observed in a previous study, where a care map ("critical pathway") was effective in reducing long-term complications and the duration of hospitalization.6)
Similar positive effects have been observed for critical care maps on the duration of hospitalization, medical costs, and patient satisfaction among cancer patients who are receiving chemotherapy.7,8)
Fast-track programs have generally been applied to relatively young patients, usually younger than 65 years of age,9,10) although readmission rates were reported to be higher in a fast-track study group above 70 years old compared to a group below 70 years old.11) However, patients who were>70 years old accounted for 22.7% of our total study population, yet there were no readmissions.
In addition, the average age of our patients in the conventional group (62.1 years) was higher than that of the fast-track group (59.9 years). Although many studies of fast-track programs have been conducted among patients who underwent laparoscopic colon surgery,8,12,13) the patients in this study underwent laparotomy.
The accepted understanding is that critical pathways can improve quality of care, facilitate cross-team collaboration, and provide patients with planned and standardized care. In addition, they can clearly and completely patient outcomes and improve the quality of the healthcare process.14) However, most critical pathways are only designed for use during the hospitalization period, while our care map also included pre-operative education. Inaddition, during the 2 weeks prior to their admission, the patients were given the opportunity to receive medical consultations over the phone.
In this study, no significant difference in bowel function recovery and pain was observed between the 2 groups. In addition, we recorded and analyzed amount of analgesics and the pain score (VAS) until discharge, and we did not identify any case where discharge was delayed because of pain. Furthermore, our results indicate that application of a fast-track program does not affect the successful recovery or incidence of complications after surgery, despite the shortened hospitalization period. In Spanjersberg et al.'s15) meta-analysis of early recovery programs after colorectal surgery, the incidence of complications was very low, and no difference was observed in the incidence of major complications; Gouvas et al.'s16) meta-analysis also reported no statistically significant differences.
Our results indicate that the use of a care map as a healthcare guide may facilitate better outcomes, compared to those obtained using a critical pathway.17,18) Therefore, the development of a care map could trigger. To successfully apply this program, active collaboration and repeated education between the operation room and wards is necessary, along with continuous evaluation of the program. Therefore, additional research is needed to validate the current fast-track program, which should be conducted via prospective studies.
Although this study was limited by a low patient number, we conclude that the fast-track program reduces recovery time after colorectal surgery, without increasing the incidence of complications. Our results indicate that the application of a fast-track program after colorectal surgery can maintain the quality, and improve the efficiency of medical service. As several university hospitals. First, additional large-scale, prospective randomized trials are needed to ensure that the fast-track program for colorectal surgery can be applied safely and effectively. Second, program validation and supplementation of the active standardization early recovery program should be performed using multi-disciplinary research.
This study has several limitations. First, it was not a prospective or randomized controlled study. Second, only a small number of patients were evaluated over a short study period. Finally, we did not assess the patients' satisfaction and acceptance of this program.
Figures and Tables
References
2. Kumar A, Scholefield JH, Andersen J, Armitage NC. Fast track surgery. In : Johnson C, Taylor I, editors. Recent Advances in Surgery. 2006. 29:p. 59–74.
3. Cheah J. Development and implementation of a clinical pathway programme in an acute care general hospital in Singapore. Int J Qual Health Care. 2000; 12:403–412.

4. Lee EO, Im NY, Park HY, Lee IS, Kim JI, Bae JE, et al. Nursing research and statistical analysis. Seoul: Soomoon-sa;2009.
5. Woodhouse A, Hobbes AFT, Mather LE, Gibson M. A comparison of morphine, pethidine and fentanyl in the postsurgical patient-controlled analgesia (PCA) environment. Pain. 1996; 64:115–121.

6. Zhu L, Li J, Li XK, Feng JQ, Gao J. Impact of a clinical pathway on hospital costs, length of stay and early outcomes after hepatectomy for hepatocellular carcinoma. Asian Pac J Cancer Prev. 2014; 15:5389–5393.

7. Kim EO. Effects of a standardized critical pathway in gastrectomy patients [dissertation]. Seoul: Seoul National Univ.;2004.
8. Wang Q, Suo J, Jiang J, Wang C, Zhao YQ, Cao X. Effectiveness of fast-track rehabilitation vs conventional care in laparoscopic colorectal resection for elderly patients: a randomized trial. Colorectal Dis. 2012; 14:1009–1013.

9. Muller S, Zalunardo MP, Hubner M, Clavien PA, Demartines N. A fast-track program reduces complications and length of hospital stay after open colonic surgery. Gastroenterology. 2009; 136:842–847.

10. Delaney CP, Zutshi M, Senagore AJ, Remzi FH, Hammel J, Fazio VW. Prospective, randomized, controlled trial between a pathway of controlled rehabilitation with early ambulation and diet and traditional postoperative care after laparotomy and intestinal resection. Dis Colon Rectum. 2003; 46:851–859.

11. Baek SJ, Kim SH, Kim SY, Shin JW, Kwak JM, Kim J. The safety of a "fast-track" program after laparoscopic colorectal surgery is comparable in older patients as in younger patients. Surg Endosc. 2013; 27:1225–1232.

12. Mari GM, Costanzi A, Maggioni D, Origi M, Giovanni C, De Martini P, et al. Fast-track versus standard care in laparoscopic high anterior resection: a prospective randomized-controlled trial. Surg Laparosc Endosc Percutan Tech. 2014; 24(2):118–121.
13. Van Bree SH, Vlug MS, Bemelman WA, Hollmann M, Ubbink D, Zwinderman K, et al. Faster recovery of gastrointestinal transit after laparoscopy and fasttrack care in patients undergoing colonic surgery. Gastroenterology. 2011; 141:872–880.

14. Beazley S, Brady AM. Integrated care pathways in orthopaedics: a literature review. J Orthop Nurs. 2006; 10:171–178.

15. Spanjersberg WR, Reurings J, Keus F, van Laarhoven CJ. Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Syst Rev. 2011; 16(2):CD007635.

16. Gouvas N, Tan E, Windsor A, Xynos E, Tekkis PP. Fast-track vs standard care in colorectal surgery: a meta-analysis update. Int J Colorectal Dis. 2009; 24:1119–1131.

17. Wennstrom B, Stomberg MW, Modin M, Skullman S. Patient symptoms after colonic surgery in the era of enhanced recovery-a long-term follow-up. J Clin Nurs. 2010; 19:666–672.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download