Abstract
Purpose
To identify the recognition of patients, families, nurses, and physicians about clinical decision-making and biomedical ethics.
Methods
Data were collected from October 23 to 30, 2012 using the structured questionnaires. A total of 200 data were analyzed using SPSS 20.0 version.
Results
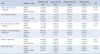
Response about 'who should receive the first notice of a cancer diagnosis?' was significant difference statistically. Cancer patients had preferences to be notified their diagnosis first. Patients responded the person who made decision of treatment options would be physician first and then themselves. Families, nurses, and physicians answered that decision-maker would be both of patient and family. All four groups answered that the person who made decision about care-giver after discharge was patient and their family. Nurses and physicians who didn't aware of the advanced directive were over 30.0%, and patients and family who didn't aware of that were over 60.0%. Lastly, the rate of positive answer about making attempt of advanced directive after legalization was over 80.0%.
References
1. Suh WS, Lee CK. Impact of shared-decision making on patient satisfaction. J Prev Med Public Health. 2010; 43(1):26–34.

2. Lee HJ. The practical model of medical decision making: interaction with three main forces (Patient-Doctor-Society). Korean J Med Ethics. 2013; 16(1):59–76.

3. Johnston B, Smith N. Nurses and patients perceptoins of expert palliative nursing care. J Adv Nurs. 2006; 54(6):700–709.

4. Kwon I, Koh YS, Yun YH, Heo DS, Seo SY, Kim HC, et al. A study of the attitudes of patients, family members, and physicians toward the withdrawal of medical treatment for terminal patients in korea. Korean J Med Ethics. 2010; 13(1):1–16.

5. Ahn SH, Kim YS, Yoo MS, Bang KS. A patient's right to know and self-determination. Korean J Med Ethics. 2009; 12(2):153–164.

6. Lee SM, Kim SH, Lee HS. The process of medical decision-making for cancer patients. Korean J Med Ethics. 2009; 12(1):1–14.

7. Kim JK. Shared decision-making as a model of medical decision-making. Korean J Med Ethics Educ. 2008; 11(2):105–118.

8. Jo KH, An GJ, Kim GM. Future changes and directions for the construction of medical decision-making system in Korea: focused on delphi surveys. Korean J Med Ethics. 2011; 14(2):131–144.
9. Yun YH, Lee CG, Kim SY, Lee SW, Heo DS, Kim JS, et al. The attitudes of cancer patients and their families toward the disclosure of terminal illness. J Clin Oncol. 2004; 22(2):307–314.

10. Baile WF, Lenzi R, Parker PA, Buckman R, Cohen L. Oncologists' attitudes toward and practices in giving bad news: an exploratory study. J Clin Oncol. 2002; 20(8):2189–2196.

11. Jo KH. Nurse's conflict experience toward end-of-life medical decision-making. J Korean Acad Adult Nurs. 2010; 22(5):488–498.
12. Lee HK, Shin JS. Relationships among ethical dilemma experienced by nurses, burnout and coping. Korean J Med Ethics. 2012; 15(3):339–354.

13. Lee SM. Patient and family determination in medical decision-making. Korean J Med Ethics. 2009; 12(4):323–334.

14. Jo KH, An GJ, Kim GM. A factor analysis of the impediments to end-stage medical decision-making as perceived by nurses and physicians in south Korea. Korean J Med Ethics. 2011; 14(4):427–442.

15. Jo KH, An GJ, Kim GM. Development of korean shared medical decision-making model for dignified dying based on king's theory. Korean J Med Ethics. 2012; 15(2):184–205.

16. Han SS. The nature of ethical dilemmas and decision making in hospital nursing practice. Seoul: Seoul National Univ.;1992. [dissertation].
17. Reem JS. Biomedical ethics and ethical theory. Korean J Med Ethics Educ. 1998; 1(1):1–20.
18. Shin YT, Lee IH, Kim SH, Lee HI. An analysis of attitudes toward advance directives among judicial apprentices and medical trainees. Korean J Med Ethics Educ. 2008; 11(1):23–36.

19. Chun IH, Park K. Patient's cognition toward the disclosure of cancer diagnosis. Asian Oncol Nurs. 2013; 13(2):59–66.

20. Tuckett AG. Truth-telling in clinical practice and the arguments for and against: a review of the literature. Nurs Ethics. 2004; 11(5):500–513.

21. Loh A, Simon D, Wills CE, Kriston L, Niebling W, Harter M. The effects of a shared decision-making intervention in primary care of depression: a cluster-randomized controlled trial. Patient Educ Couns. 2007; 67(3):324–332.

23. Briggs L, Colvin E. The nurse's role in end-of-life decision-making for patients and families. Geriatr Nurs. 2002; 23(6):302–310.

24. Royak-Schaler R, Gadalla SM, Lemkau JP, Ross DD, Alexander C, Scott D, editors . Family perspectives on communication with healthcare providers during end-of-life cancer care. Oncol Nurs Forum. 2006; 33(4):753–760.

25. Surbone A. Telling the truth to patients with cancer: what is the truth? Lancet Oncol. 2006; 7(11):944–950.

26. Ham MY, Choi KS, Eun Y, Kwon IS, Ryu EJ. Demands of illness in cancer patients in outpatients settings. J Korean Oncol Nurs. 2001; 1(2):147–156.
27. Choi ES, Kim KS. Experiences of family caregivers of patients with terminal cancer. J Korean Acad Nurs. 2012; 42(2):280–290.

28. Koh YS, Heo DS, Yun YH, Moon JL, Park HW, Choung JT, et al. Charactersitics and issues of guideline to withdrawal of a life-sustaining therapy. J Korean Med Assoc. 2011; 54(7):747–757.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download