Abstract
Purpose
The purpose of this study was to identify predictors of repeated Papanicolaou (Pap) smears in women older than 30 years being offered free national cervical cancer screening.
Methods
Data were collected using self-administered questionnaires from October 15 to November 30, 2012. Data were analyzed using t-test, chi-square test and multiple logistic regression. This study was to investigate the association of general factors, health status, risk factors of cervical cancer, and health beliefs associated with repeated Pap smeasr.
Results
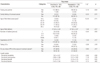
The rate of repeated Pap smear was 23.5%. Factors that influence repeated Pap smear included breast cancer screening (OR=2.16, 95% CI=1.037-4.491) and perceived sensitivity (OR=1.49, 95% CI=1.008-2.192).
Conclusion
The results of this study suggest that to increase the rate of repeated Pap smear tests, education and promotion should be carried out together, considering the relationship between cervical and breast cancer. Also, health education should emphasize perceptivity and sensibility for the incidence of cervical cancer.
Figures and Tables
References
1. Benedet JL, Anderson GH, Matisic JP. A comprehensive program for cervical cancer detection and management. Am J Obstet Gynecol. 1992. 166:1254–1259.

2. National Cancer Information Center. 2011 Prevention. Screening. Accessed October 8, 2012. http://ncc.re.kr.
3. National Cancer Center. 2012 A survey on cancer screening method. Accessed October 15, 2012. http://www.cancer.go.kr.
4. National Cancer Information Center. 2011 Cancer Statistics. Accessed October 14, 2012. http://www.cancer.go.kr.
5. American Cancer Society. Cervical cancer. Accessed October 14, 2012. http://www.cancer.org/Cancer.
6. Kim SY, Choi SY. Pap smear screening participation behavior and related factors in married immigrant women. Korean J Women Health Nurs. 2010. 16:255–265.

7. Shin HC. Social and behavioral predictors of cervical cancer screening practices among korean women. J Korean Acad Fam Med. 2001. 22:1823–1837.
8. Lee SR. Factors to put restrictions on cervical cancer screening. Korean Public Health Res. 2002. 28:1–9.
9. Jeong IS, Ju HO, Bae ES. Related factors to screening or repeat screening for cervical and breast cancer among women. Korean J Women Health Nurs. 2004. 10:150–161.

10. Centers for Disease Control and Prevention. Cervical cancer screening. Accessed December 1, 2012. http://www.cdc.gov.
11. Kim YB, Lee WC, Kim M, Chung CK. The Predictive factors to participation in cervical cancer screening program. Korean J Prev Med. 2001. 34:237–243.
12. Kim HL, Kim HS. A study of pap smear screening for cervical cancer prevention of women and follow-up strategies for recall in Cheju city. Korean Public Health Res. 2000. 26(3):276–281.
13. Oh EJ, Lee YE, Lee SO. Cervical cancer screening behavior and related factors among married women. J Korean Soc Matern Child Health. 2010. 14:12–23.

14. Grangé G, Malvy D, Lançon F, Gaudin AF, El Hasnaoui A. Factors associated with regular cervical cancer screening. Int J Gynaecol Obstet. 2008. 102:28–33.

15. Jalilian F, Emdadi S. Factors related to regular undergoing pap-smear: application of theory of planned behavior. JRHS. 2011. 11:103–108.
16. Abdullah F, Aziz NA, Su TT. Factors related to poor practice of pap smear screening among secondary school teachers in Malaysia. Asian Pac J Cancer Prev. 2011. 12:1347–1352.
17. Lee HJ, Lee SH, Jung SH, Shin HR, Oh DK. Analysis of behavioral stage in pap testing by using trans theoretical model. J Prev Med Public Health. 2005. 38:82–92.
18. Choi KS, Lee DH, Jung KY, Son JE, Jang TW, Kim YK, et al. Factors associated with cervical cancer screening in Busan, Korea. J Prev Med Public Health. 2004. 37:166–173.
19. Choi KA, Kim JH, Lee KS, Oh JK, Liu SN, Shin HR. Knowledge of human papillomavirus infection and acceptability of vaccination among adult women in Korea. Korean J Obstet Gynecol. 2008. 51:617–623.
20. Park SM. Factors related to continuous participation in the pap smear screening among Korean women: using a structural model. J Korean Acad Nurs. 2000. 30:160–170.

21. Cho IS, Park YS. A study on regular cervical cancer screening behavior among middle-aged women. J Korean Acad Nurs. 2004. 34:141–149.

22. Kaiser State Halth Facts. Pap smear rate. Accessed December 3, 2012. http://www.statehealthfacts.org.
23. American Society for Colposcopy and Cervical Pathology. Accessed December 1, 2012. http://www.asccp.org.
24. Park EH, Cho YH, Kim WJ. Influence of health beliefs on preventive health behaviors for cancer among middle-aged women. Health Welf. 2009. 11:17–42.

25. Jang SN, Cho SI, Hwang SS, Jung-Choi KH, Im SY, Lee JA, et al. Trend of socioeconomic inequality in participation in cervical cancer screening among Korean women. J Prev Med Public Health. 2007. 40:505–511.

26. Lantz PM, Weigers ME, House JS SH. Education and income differentials in breast and cervical cancer screening. Med Care. 1997. 35:219–236.

27. Kang SM. Cervical cancer guidebook. 2007. Seoul: GukIl Publishers.
28. Jung EC, Jin CH. Breast and cervical cancer communication channels and screening intention. Korean J Commun Stud. 2011. 19:139–162.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download