Abstract
Purpose
This study was conducted to test whether sleep disturbance mediates the effect of pain on fatigue, whether fatigue mediates the effect of pain on depression, and whether fatigue mediates the effect of sleep disturbance on depression.
Methods
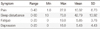
This study was conducted from September 12th to December 20th, 2011. One hundred eighty-eight breast cancer patients were recruited from D city and S city in Korea. The instruments used in this study were the pain, sleep disturbance, fatigue, and depression scales. Data were analyzed using descriptive statistics, Pearson correlation coefficients, and mediation pathway with the SPSS 12.0 and AMOS 20.0 programs.
Results
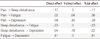
There was correlation among pain, fatigue, sleep disturbance, and depression. Mediation analyses indicated that pain influences fatigue. sleep disturbance, and depression directly as well as indirectly. Sleep disturbance influences fatigue and depression directly, also fatigue influences depression directly. But sleep disturbance had no direct effect on depression.
Conclusion
Significant correlations among the four symptoms supported the existence of the symptom cluster. Effects of pain on fatigue was partially mediated by sleep disturbance, also effects of pain on depression was partially mediated by fatigue. However, the effects of sleep disturbance on depression was fully mediated by fatigue.
Figures and Tables
References
2. Byar KL, Berger AM, Bakken SL, Cetak MA. Impact of adjuvant breast cancer chemotherapy on fatigue, other symptoms, and quality of life. Oncol Nurs Forum. 2006. 33:E18–E26.

4. Fan G, Filipczak L, Chow E. Symptom cluster in cancer patients: A review of the literature. Curr Oncol. 2007. 14:173–179.
5. Beck SL, Dudley WN, Barsevick A. Pain, sleep disturbance, and fatigue in patients with cancer: Using a mediation model to test a symptom cluster. Oncol Nurs Forum. 2005. 32:542.

6. Kirkova J, Walsh D, Aktas A, Davis MP. Cancer symptom cluster: Old concept but new data. Am J Hosp Palliat Care. 2010. 27:282–288.
7. Kim GD, Kim KH. Symptom cluster and quality of life with breast cancer undergoing chemotherapy. Korean J Adult Nurs. 2011. 23:434–445.
8. Stevens PE, Dibble SL, Miaskowski C. Prevalence, characteristics, and impact of postmastectomy pain syndrome: an investigation of women experience. Pain. 1995. 61:61–68.

9. Jung BF, Hermann D, Griggs J, Oaklander LA, Dworkin RH. Neuropathic pain associated with non-surgical treatment of breast cancer. Pain. 2005. 118:10–14.

10. Kim HJ, Barsevick AM, Tulman L, McDermott PA. Treatment-related symptom clusters in breast cancer: A secondary analysis. J Pain Symptom Manage. 2008. 36:468–479.

11. Fiorentino L, Rissling M, Liu L, Ancoli-Israel S. The symptom cluster of sleep, fatigue and depressive symptoms in breast cancer patients: severity of the problem and treatment options. Drug Discov Today Dis Models. 2011. 8:167–173.

12. Park YM. A structural model for quality of life in breast cancer patients. 2005. Seoul: Kyunghee Univ.;[dissertation].
13. Lis CG, Gupta D, Grutsch JF. The relationship between insomnia and patient satisfaction with quality of life in cancer. Support Care Cancer. 2008. 16:261–266.

14. Park JH, Lee SJ, Gwak JI, Shim JY, Lee JK. Sleep quality of breast cancer patients receiving chemotherapy in the outpatients setting. Korean J Fam Med. 2010. 31:778–785.

16. Miaskowski C, Cooper BA, Paul SM, Dodd M, Lee K, Aouizerat BE, et al. Subgroups of patients with cancer with different symptom experiences and quality-of-life outcomes: A cluster analysis. Oncol Nurs Forum. 2006. 33:E79–E89.

17. Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, Mcgregor BA, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry. 2008. 30:112–126.

18. Pud D, Ben Ami S, Cooper BA, Aouizerat BE, Cohen D, Radiano R, et al. The symptom experience of oncology outpatients has a different impact on quality-of life outcomes. J Pain Symptom Manage. 2008. 35:162–170.

19. Dodd MJ, Cho MH, Cooper BA, Miaskowski C. The effect of symptom cluster on functional status and quality of life in women with breast cancer. Eur J Oncol Nurs. 2010. 14:101–110.

20. Bower JE, Meyerowitz BE, Desmond KA, Benaards CA, Rowaland JH, Ganz PA. Perception of positive meaning and vulnerability following breast cancer: Predictor and outcomes among long-term breast cancer survivors. Ann Behav Med. 2005. 29:236–245.

21. Daut RL, Cleeland CS, Flanery RC. Developmant of the Wisconsin Brief Pain Questionnaire to assess pain in cancer and other diseases. Pain. 1983. 17:197–210.

22. Kang JY. The effect of preparatory audiovisual information with videotape influencing on sleep and anxiety of abdominal surgical patients [dissertation]. 1992. Seoul: Seoul National Univ..
23. Yeun EJ, Shin-Park KK. Verification of the profile of mood states-brief: Cross-cultural analysis. J Clin Psychol. 2006. 62:1173–1180.

24. Hair JFJ, Anderson RE, Tatham RL, Black WC. Multivariate data analysis. 1998. 5th ed. New York: Prentice-Hall International.
25. Cheng KKF, Lee DTF. Effects of pain, fatigue, insomnia, and mood disturbance on functional status and quality of life of elderly patients with cancer. Crit Rev Oncol Hematol. 2011. 78:127–137.

26. So Winnie KW, Marsh G, Ling WM, Leung FY, Lo JCK, Yeung M, et al. The symptom cluster of fatigue, pain, anxiety, and depression and the effect on the quality of life of women receiving treatment for breast cancer: A multicenter study. Oncol Nurs Forum. 2009. 36:E205–E214.
27. Reuter K, Classen CC, Roscoe JA, Morrow GR, Kirshner JJ, Rosenbluth R. Association of coping style, pain, age, and depression with fatigue in women with primary breast cancer. Psychooncology. 2006. 15:772–779.

28. Hwang JR. Pain related factors, pain intensity and nature, and mood states in neuropathic pain patients [dissertation]. 2010. Seoul: Hanyang Univ..




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download