Abstract
This case report illustrates the successful treatment of a patient with skeletal Class II malocclusion and an unesthetic smile involving excessive gingival display and large buccal corridors. By applying dual buccal interradicular miniscrews, total intrusion of the maxillary dentition along with distalization was induced to improve both the occlusion and smile esthetics. In addition to the conventional cephalometric superimposition, three-dimensional superimposition was performed and evaluated to validate the treatment outcome.
The improvement of smile esthetics is a top priority in contemporary adult orthodontic treatment. In addition to ideal occlusion, adequate gingival display with a harmonious gingival line, balanced smile arc, and ideal buccal corridor are key factors for an esthetic smile and facial attractiveness.12
Excessive gingival display, also known as “gummy smile,” is characterized by excessive exposure of the maxillary gingiva while smiling. Gingival display of more than 2 mm while smiling is considered excessive and unattractive.34 Gummy smile is caused by skeletal disharmony, such as vertical and horizontal excess of the maxilla or the maxillary dentition, which, in many cases, accompanies a functional imbalance of soft tissues, such as the upper lip or elevating muscles.56 Thus, in general, various intrusion or surgical mechanics are applied to reduce the vertical dimension of the maxillary arch or maxilla based on the etiology and severity of the malocclusion.7 However, changes in the vertical exposure of the maxillary anterior teeth may also influence the smile arc esthetics in the transverse dimension. From a clinical perspective, excessive intrusion of the maxillary anterior teeth produces a flat or reverse smile arc, which is considered unattractive and less esthetic than is a consonant smile arc.8
Among the various intrusion mechanics applied during orthodontic treatment, the application of temporary anchorage devices (TADs) is well known for its effectiveness in the intrusion of the anterior or posterior teeth.9101112 In addition to selective regional intrusion, a biomechanical approach has been proposed in order to achieve full-arch intrusion along with distalization in the maxillary dentition by applying multiple interdental miniscrews (i.e., 2 miniscrews on each side). Dual force vectors allow the line of action to pass through the center of resistance (CR) of the entire maxillary arch and facilitate the retraction and intrusion of the entire dentition without changes in the occlusal plane.13
Herein, we report the treatment outcome with follow-up results of an adult patient with skeletal Class II malocclusion who was concerned about her unesthetic smile. After a thorough evaluation of smile esthetics, we applied total maxillary intrusion combined with distalization to establish ideal occlusion and to improve the smile esthetics as well as soft-tissue profile.
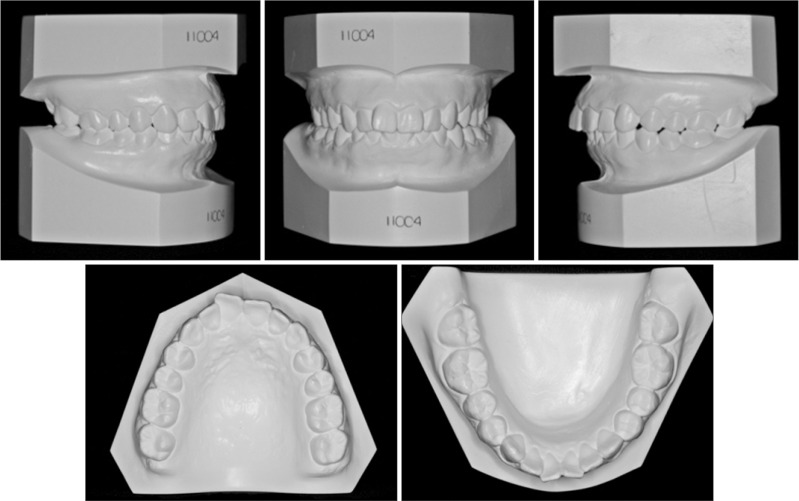
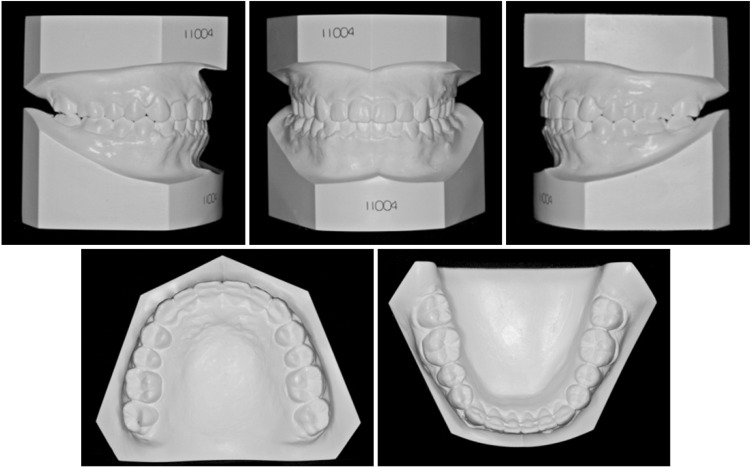
A 25-year-old woman visited the clinic with the chief complaint of an unattractive and awkward smile and lip protrusion. The pretreatment frontal facial photographs indicated a symmetric face with relatively harmonious facial proportions. However, excessive gingival display, crowding, and relatively large buccal corridors were noted at full smile. She also had a retrognathic mandible with protrusive upper and lower lips. An intraoral examination indicated deep overbite (4 mm) and Class II canine and molar relationship. The arch length discrepancy was −1.5 mm in both the arches. The maxillary arch form was narrow and tapered with a decreased intercanine width of 31.4 mm compared to the normal width of 33.7 mm.14 The mandibular arch showed a deep curve of Spee (Figures 1 and 2).
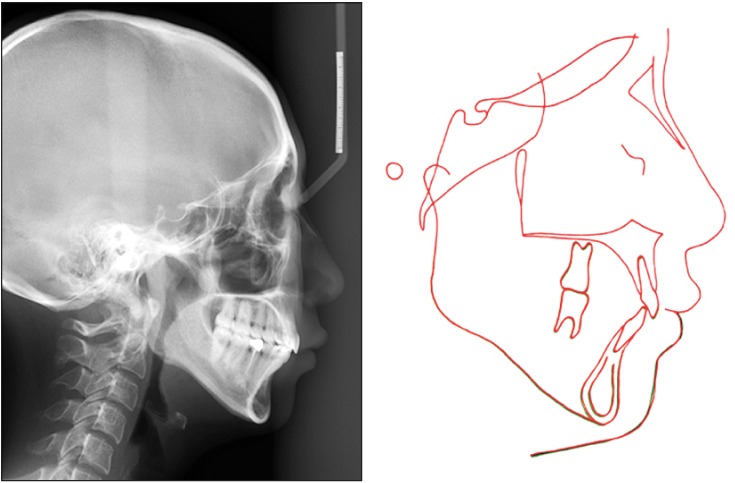
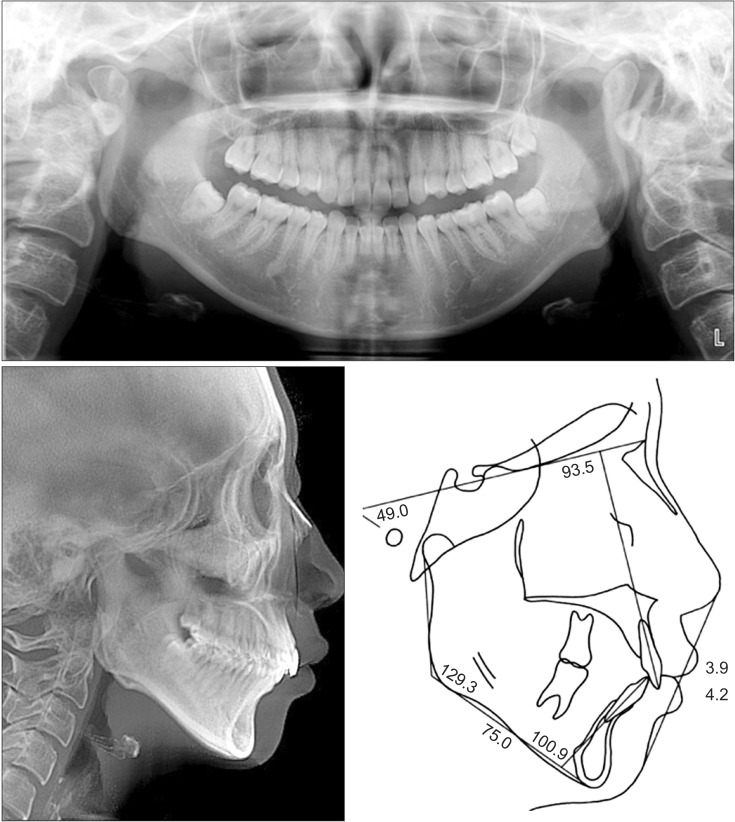
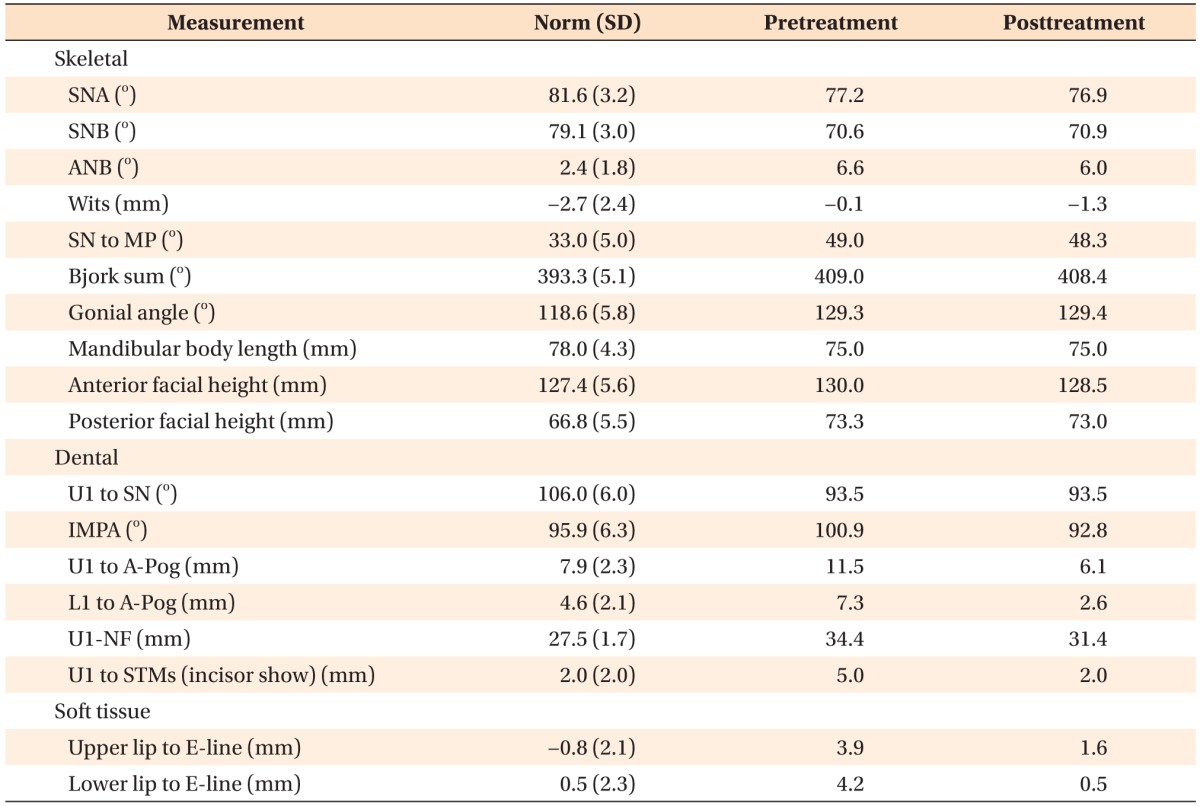
The initial radiographic evaluation indicated mild flattening of both the condyles with relatively short ramal height. However, no dental or skeletal midline deviation was observed. The cephalometric analysis showed a skeletal Class II relationship with a retrognathic mandible (sella-nasion-A point [SNA], 77.2°; sellanasion-B point [SNB], 70.6°; A point-nasion-B point [ANB], 6.6°) and a hyperdivergent profile (mandibular plane angle, 49.0°). Because of the retrusive mandible, the upper and lower lips protruded 3.9 and 4.2 mm, respectively, to the E-line. The maxillary incisors were retroclined (U1 to SN, 93.5°) and the mandibular incisors were proclined (IMPA, 100.9°) (Figure 3).
Since the patient’s chief complaint was focused on the unattractive smile, we additionally evaluated the smile esthetics. At full smile, she had excessive gingival display (> 3.5 mm), but the smile arc was consonant to the lower lip. The overall vertical proportion of the middle 1/3 of the face (G-Sn/Sn-Me’) and the maxilla (N-ANS/ANS-Me) were within normal boundaries at 1.2 and 0.8, respectively, whereas the distance from the maxillary incisor tip to the nasal floor (U1 to nasal floor) and maxillary incisor show (U1 to STMs) were high at 34.4 and 5.0 mm, respectively. These findings indicated that the main cause of excessive gingival display was the overeruption of the maxillary incisors rather than the vertical growth of the maxilla.15 Periodontal analysis revealed no specific sign of gingival hyperplasia, and the probing depth was within normal range (< 3 mm). The patient displayed a thick flat biotype, with a crown width/length ratio of 1.0, indicating a shorter crown height than crown width.
The buccal corridor ratio (calculated as the difference between the visible maxillary dentition width and the inner commissure width divided by the inner commissure width) was 25%, which was relatively large compared to the esthetic normal ratio of 10–15%.16 Along with the tapered arch form, the lingual crown torque of the maxillary canines and premolars was excessive at −9° and −12°, respectively, when compared to the normal torque of −0.8° and −6.3°, respectively, for Koreans.17 The excessive lingual crown torque of the canines and premolars negatively affects smile esthetics.18
On the basis of these findings, the patient was diagnosed with a hyperdivergent skeletal Class II malocclusion and an unesthetic smile.
The treatment objectives were (1) to improve the smile esthetics by reducing excessive gingival display and buccal corridors while maintaining an ideal smile arc; (2) to improve facial esthetics; and (3) to establish functional occlusion.
Since the malocclusion and associated lip protrusion were mainly caused by the retrusive mandible/chin with a steep mandibular plane angle, the first treatment option was to combine orthognathic surgery for advancing the mandible with the extraction of the mandibular premolars. Along with mandibular advancement, maxillary impaction can be considered to reduce the excessive gingival display and to ensure stability. These surgical approaches may improve the overall facial profile and the gummy smile per se.19 However, the main cause of the unesthetic smile had a dentoalveolar origin rather than a skeletal origin, and the expected final occlusion after surgery would be a Class III molar relationship.
The main objective of the camouflage treatment would be to reduce lip protrusion (sagittal) and to improve the smile esthetics (vertical and transverse). According to the visualized treatment objective, an approximately 3-mm retraction of the incisors was needed to ensure an ideal incisor position against the A-Pog line and facial plane (Table 1). Conventionally, the extraction of 4 premolars has been an effective option to control the sagittal and vertical problems. However, considering the small arch length discrepancy, over 4 mm of anchorage loss was expected after premolar extractions. In addition, in the transverse dimension, it was necessary to upright the canines and premolars which showed excessive lingual crown torque in order to increase the width of the smile and to decrease the buccal corridors.18 However, if this treatment option were selected, the changes in the arch form would eventually have resulted in more residual space.
The third option was to distalize both the arches to improve lip protrusion along with vertical control by using skeletal anchorage.20 The anatomic space available at the maxillary tuberosity distal to the maxillary second molars (3.6 mm on the right, and 8.9 mm on the left) as well as the distance to the anterior border of the ramus (4.3 mm on the right, and 7.2 mm on the left) and that to the inner lingual cortex from the mandibular second molars (3.0 mm on the right, and 1.7 mm on the left) were sufficient to withhold the amount of necessary distalization with the extraction of the third molars (Figure 4).21 In addition, the use of buccal interradicular miniscrews during distalization biomechanically results in buccal uprighting of the canines and premolars with mild arch expansion.10 Since the patient’s smile arc was consonant to the mandibular lip line, maxillary anterior intrusion alone may flatten the smile arc, which would make the patient look older and drastically reduce the smile attractiveness ratings.8 Thus, to specifically maintain the consonant smile arc, total intrusion of the maxillary dentition without changing the occlusal plane was planned with the use of multiple miniscrews.13 This plan would improve the lip protrusion and smile esthetics without affecting the ideal smile arc. It would also produce a total impaction-like effect on the maxilla, which may be advantageous to the profile because of the counterclockwise rotation of the mandible.
The three treatment options were discussed with the patient. Since the frontal smile esthetics and lip protrusion were the main concerns of the patient, option 3 was selected as the final orthodontic treatment option.
After the extraction of the third molars, 0.018-slot self-ligation brackets (Clippy C; Tomy Inc., Tokyo, Japan) were bonded on both the arches, and sequential nickel-titanium wires were used for leveling and alignment.
In the maxilla, distalization and intrusion of the complete maxillary dentition was necessary. The distalizing force applied from a single miniscrew inserted at the level of the mucogingival junction between the first molar and second premolar to the retraction hook of a rigid maxillary archwire results in total distalization of the dentition. However, it may also result in mild clockwise rotation of the occlusal plane.13 Thus, to overcome this biomechanical issue and to induce a “total impaction-like effect” without changes in the occlusal plane, additional miniscrews were inserted between the premolars to create a line of force that passes near the CR of the maxillary arch (Figure 5A).13
The interradicular space between the premolars and the molar were 2.5 and 2.6 mm (right side), respectively, and 2.3 and 1.7 mm (left side), respectively, at the mucogingival junction, approximately 4 mm above the cementoenamel junction. Considering the possibility of root contact along with total arch distalization, the miniscrews were inserted at the midpoint between adjacent teeth at 45° angulation relative to the occlusal plane at the level of the mucogingival junction, as described in previous studies.22 Four tapered miniscrews 7.0 mm in length and 1.6 mm in coronal diameter (Orlus; Ortholution, Seoul, Korea) were inserted with two screws on each side. A 0.016 × 0.022-inch stainless-steel flat arch wire was engaged using crimpable hooks located between the maxillary lateral incisor and canine and between the canine and first premolar. A distal driving force of 200 g was applied using elastomeric chains from each miniscrew to the hook in order to deliver the intrusive and distalizing force vector passing near the estimated CR (Figure 5B and 5C).13 At 9 months, a mild curve of Spee was added to the main archwire to compensate for the mild torque changes over the following 3 months. In the mandible, a one-piece intrusion arch was applied to relieve the curve of Spee after initial alignment.
After 12 months of treatment, an interim evaluation of gingival display and lip protrusion was performed. Despite a great reduction in gingival display while smiling, without any changes in the ideal consonant smile arc, sagittal correction was necessary to improve lip protrusion. The miniscrews (Orlus) were also inserted between the mandibular second premolar and first molar with a 45° angulation relative to the occlusal plane. Full-arch distalization was continued for another 6 months in both the arches (Figure 5D and 5E).
The appliances were removed after 19 months of active treatment. Although her oral hygiene was ideal and the probing depth did not exceed 3 mm throughout the treatment period, the gingival margin of the maxillary incisors became uneven, and the crown width/length ratio slightly increased from 1.0 to 1.03 possibly due to the large amount of intrusion in the maxillary dentition. Therefore, gingivoplasty was performed on the maxillary incisors to recontour the gingival margins (Figures 5F and 5G). Fixed lingual retainers were bonded to the lingual surfaces of both the arches, and circumferential retainers were used full time for the first 6 months.
The facial and smile esthetics along with the lateral profile were improved with the treatment. An ideal gingival display while smiling was achieved and the consonant smile arc was maintained after treatment. The buccal corridor ratio was reduced to 15%. The occlusion was completed with a Class I canine and molar relationship along with ideal overjet and overbite. The height of the gingival margins was even, and the crown width/length ratio was reduced to 0.8. The patient was fully satisfied with the treatment outcome (Figures 6, 7, 8).
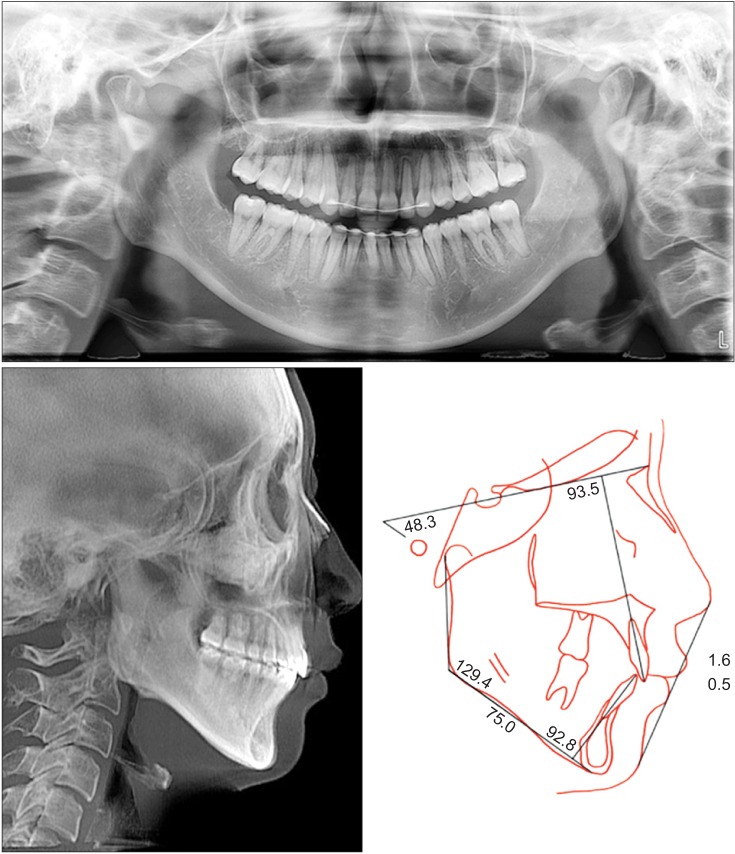
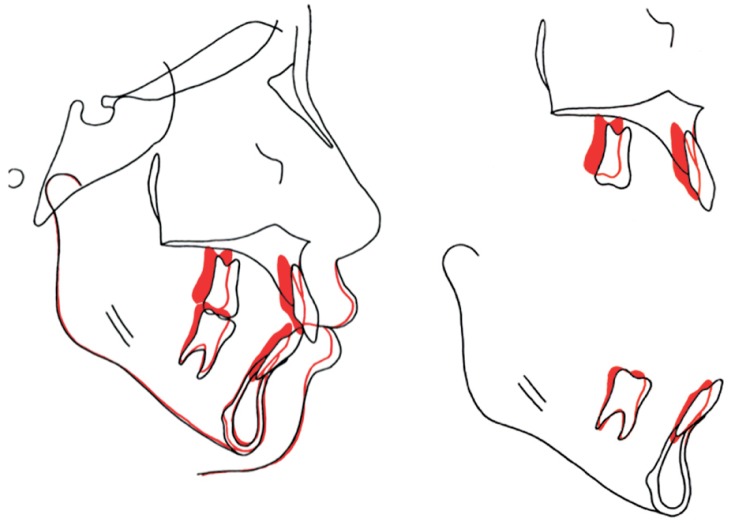
The cephalometric superimposition revealed significant total intrusion and distalization of the maxillary arch without changes in the occlusal plane. Counterclockwise rotation of the mandible could be induced, and it resulted in mild advancement of the pogonion and soft-tissue pogonion, as well as slight reduction of the anterior facial height. Lip prominence was reduced by 2.3 and 3.5 mm in the upper and lower lips, respectively, after full-arch distalization (Figure 9).
Cone-beam computed tomography (CBCT) images taken before and after treatment were superimposed on the cranial base. It indicated total impaction of the maxillary dentition along with counterclockwise rotation of the mandible. Specifically, the maxillary incisors were intruded 2.0 mm and distalized 3.0 mm from the initial position while maintaining the incisor torque, whereas the maxillary molars were intruded 2 mm and distalized 2.5 mm on the right side and 3.5 mm on the left side. In the mandible, the incisors were intruded 2.0 mm and uprighted 2.0 mm, whereas the molars were distalized and uprighted by 2.0 mm along with the distal tip of the mandibular second molars (Figrue 10). Along with tooth movement, changes in the arch form, including flattening of the anterior arch, were noted in both the arches (Figure 11). The position of both the condyles was maintained throughout the treatment (Figure 12). Mild root blunting was observed at the incisors after treatment. However, the overall position of the incisors was within the biological boundaries, and the torque was maintained (Figure 13).
The patient did not comply with the directions regarding the use of the removable retainers. Nevertheless, the occlusion and smile esthetics were stably maintained throughout the follow-up period. She maintained excellent oral hygiene, and her periodontal condition was ideal (Figure 14). Superimposition analyses performed at debonding and after 15 months of follow-up did not indicate any clinical significance (Figure 15).
When the intraoral aspects of the occlusion per se are evaluated, the patient in the present case may be considered as having a simple Class II deepbite malocclusion. However, the diagnosis based on the smile esthetics revealed problems in the vertical (excessive gingival display, but with a consonant smile arc) and transverse planes (large buccal corridors) in addition to the sagittal (lip protrusion and Class II relationship) plane. Therefore, three-dimensional (3D) tooth movement was planned to improve both the static and functional smile esthetics.
Simple biomechanics like TADs can be applied to achieve 3D movement of the whole dentition without concerns regarding anchorage or patient compliance. The CR of the whole maxillary dentition is suggested to be near the middle area of the premolar roots.23 From a biomechanical perspective, a line of distalization force applied from the TADs to the maxillary arch by using hooks between the canine and lateral incisor passes below the CR point, because the TADs are frequently inserted in the attached gingival zone between the maxillary first and second premolars. This may steepen the occlusal plane and clinically aggravate the gummy smile.10,24 Thus, we applied two additional miniscrews, one on each side between the premolars, and applied individual forces to the 2 hooks on each side to ensure that the line of action passes close to the CR (Figure 5).13 As a result, simultaneous total distalization and intrusion of the maxillary dentition was effectively achieved, thereby improving both the smile esthetics as well as the occlusion.
Traditionally, orthodontists have focused more heavily on the views of the face from the lateral aspect than do most other viewers. However, facial attractiveness correlates more highly to smiling photographs than to profile photographs.25 Considering the patient’s needs and esthetic concerns, the smile esthetics were monitored throughout the treatment period, and the treatment outcome was evaluated in the transverse, vertical, and sagittal planes.
In the transverse plane, the use of dual buccal interradicular miniscrews broadened the arch form, as has been suggested in previous reports.26 Thus, the buccal corridor ratio at smile improved from 25% to 15%, which was close to the ideal ratio of 10–15%.14 Initially, the patient had a narrow tapered arch form with excessive lingual crown torque in the maxillary canine and premolars. In such cases, buccal uprighting of the canines and premolars is recommended to widen the smile and reduce the buccal corridors.18 Buccal uprighting of the canine and premolars results in arch expansion. However, unlike the conventional arch expansion in adults, which is well known for its instability, buccal uprighting shows high long-term stability.27 From a biomechanical perspective, we utilized buccal miniscrews, which eventually result in buccal tipping throughout the treatment process. Accordingly, the excessive lingual crown torque was normalized, and the change in the arch form was beneficial. Posttreatment photographs revealed a full and natural smile. However, for patients with a broad arch form or narrow buccal corridors, careful monitoring is recommended to prevent unwanted changes in arch width as the treatment progresses.
In the vertical plane, excessive gingival display at smile and incisor show at rest were reduced to the ideal norms,2 whereas the ideal smile arc was maintained through total intrusion of the maxillary arch. However, following the large amounts of intrusion, the clinical crown height was also reduced by an average of 0.4 mm per tooth. This decrease in clinical crown height may have been due to the inability of the gingival complex to keep up with the speed of apical tooth movement.28 The response of the periodontal tissue following intrusion is highly related to the standard of oral hygiene.29 Experimental studies have shown that the clinical crown height may decrease because of gingival accumulation after intrusion without visual and histologic signs of inflammation.28 The patient maintained excellent oral hygiene; however, gingivoplasty was recommended after orthodontic treatment to improve the microesthetics of the maxillary incisors. The unevenness of the gingival margins became symmetric and the crown width and height ratio improved after gingivoplasty. From a biological perspective, large amounts of intrusion may also be associated with apical root resorption.3031 In this patient, relatively mild apical root resorption occurred after a 2-mm anterior and molar intrusion.
In the sagittal plane, the patient’s retrognathic mandible caused major concerns. Although the large skeletal discrepancies remained unchanged and resulted in limited outcome of the camouflage treatment, we tried to improve lip protrusion and the Class II relationship through full-arch distalization and intrusion. Since the patient had a third molar space available distal to the second molars and approximately 3 mm from the roots to the lingual cortical plate, which is considered an anatomic limit for mandibular distalization,2032 tooth movement per se was effectively achieved through the application of a distal force from the miniscrews. In our case, a total intrusion of 2 mm induced minor counterclockwise rotation of the mandible and advancement of the pogonion. Although the amount of counterclockwise rotation in response to the amount of maxillary intrusion is difficult to predict precisely, it is without doubt advantageous in terms of the profile esthetics and vertical control in cases of Class II high-angle malocclusions.1011 However, although the patient showed a significantly high mandibular plane angle in the sagittal view, she may well be categorized as having a brachyfacial type in the frontal view because of the relatively high facial width and interzygoma distance. In addition, the proportion of the lower 1/3 to the total facial height or to the midface was harmonious initially. Thus, an excessive decrease of lower facial height through counterclockwise rotation should always be monitored in the frontal plane because it may negatively affect the facial proportions.
CBCT superimposition to the cranial base was used to validate the treatment outcome in all 3 dimensions. Not only did it enable the observation of changes in the sagittal plane similar to the conventional superimposition, but it also enabled the measurement of the extent of individual tooth movement, as well as the changes in the transverse arch dimension and soft-tissue profile.32 Precise anatomical evaluation, such as that of the condylar position following counterclockwise rotation, the presence of root resorption, and the surrounding alveolar housing, as well as follow-up evaluation confirmed that the treatment results were satisfactory and stable.
To improve smile esthetics, smile was monitored in the transverse, vertical, and sagittal planes. The findings of this case study show that total intrusion and distalization of the maxillary dentition by using multiple TADs is a viable option for the treatment of skeletal Class II malocclusion associated with excessive gingival display and large buccal corridors.
Notes
References
1. Garber DA, Salama MA. The aesthetic smile: diagnosis and treatment. Periodontol 2000. 1996; 11:18–28. PMID: 9567953.

2. Chang CA, Fields HW Jr, Beck FM, Springer NC, Firestone AR, Rosenstiel S, et al. Smile esthetics from patients' perspectives for faces of varying attractiveness. Am J Orthod Dentofacial Orthop. 2011; 140:e171–e180. PMID: 21967955.

3. Hunt O, Johnston C, Hepper P, Burden D, Stevenson M. The influence of maxillary gingival exposure on dental attractiveness ratings. Eur J Orthod. 2002; 24:199–204. PMID: 12001557.

4. An SM, Choi SY, Chung YW, Jang TH, Kang KH. Comparing esthetic smile perceptions among laypersons with and without orthodontic treatment experience and dentists. Korean J Orthod. 2014; 44:294–303. PMID: 25473645.

5. Hwang WS, Hur MS, Hu KS, Song WC, Koh KS, Baik HS, et al. Surface anatomy of the lip elevator muscles for the treatment of gummy smile using botulinum toxin. Angle Orthod. 2009; 79:70–77. PMID: 19123705.

6. Kim SJ, Kim JW, Choi TH, Lee KJ. Combined use of miniscrews and continuous arch for intrusive root movement of incisors in Class II division 2 with gummy smile. Angle Orthod. 2014; 84:910–918. PMID: 24512532.

7. Proffit WR, Phillips C, Turvey TA. Stability following superior repositioning of the maxilla by LeFort I osteotomy. Am J Orthod Dentofacial Orthop. 1987; 92:151–161. PMID: 3475970.

8. Parekh SM, Fields HW, Beck M, Rosenstiel S. Attractiveness of variations in the smile arc and buccal corridor space as judged by orthodontists and laymen. Angle Orthod. 2006; 76:557–563. PMID: 16808559.
9. Baek MS, Choi YJ, Yu HS, Lee KJ, Kwak J, Park YC. Long-term stability of anterior open-bite treatment by intrusion of maxillary posterior teeth. Am J Orthod Dentofacial Orthop. 2010; 138:396.e1–396.e9. discussion 396-8. PMID: 20889043.

10. Kuroda S, Sakai Y, Tamamura N, Deguchi T, Takano-Yamamoto T. Treatment of severe anterior open bite with skeletal anchorage in adults: Comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop. 2007; 132:599–605. PMID: 18005833.

11. Deguchi T, Kurosaka H, Oikawa H, Kuroda S, Takahashi I, Yamashiro T, et al. Comparison of orthodontic treatment outcomes in adults with skeletal open bite between conventional edgewise treatment and implant-anchored orthodontics. Am J Orthod Dentofacial Orthop. 2011; 139(4 Suppl):S60–S68. PMID: 21435540.

12. Arai C, Choi JW, Nakaoka K, Hamada Y, Nakamura Y. Management of open bite that developed during treatment for internal derangement and osteoarthritis of the temporomandibular joint. Korean J Orthod. 2015; 45:136–145. PMID: 26023542.

13. Bechtold TE, Kim JW, Choi TH, Park YC, Lee KJ. Distalization pattern of the maxillary arch depending on the number of orthodontic miniscrews. Angle Orthod. 2013; 83:266–273. PMID: 22970751.

14. Sohn BW, Lee JG, Kim HS, Kim HS. Semi-longitudinal study of growth and development of children aged 6 to 17 Part I: Growth and development of arch form. Korean J Orthod. 1996; 26:225–239.
15. Burstone CJ, James RB, Legan H, Murphy GA, Norton LA. Cephalometrics for orthognathic surgery. J Oral Surg. 1978; 36:269–277. PMID: 273073.
16. Ioi H, Kang S, Shimomura T, Kim SS, Park SB, Son WS, et al. Effects of buccal corridors on smile esthetics in Japanese and Korean orthodontists and orthodontic patients. Am J Orthod Dentofacial Orthop. 2012; 142:459–465. PMID: 22999668.

17. Park YC. A morphologic study on straight wire bracket for Korean. Korean J Orthod. 1991; 21:481–493.
18. Zachrisson BU. Buccal uprighting of canines and premolars for improved smile esthetics and stability. World J Orthod. 2006; 7:406–412. PMID: 17190235.
19. Schendel SA, Carlotti AE Jr. Variations of total vertical maxillary excess. J Oral Maxillofac Surg. 1985; 43:590–596. PMID: 3859608.

20. Choi YJ, Lee JS, Cha JY, Park YC. Total distalization of the maxillary arch in a patient with skeletal Class II malocclusion. Am J Orthod Dentofacial Orthop. 2011; 139:823–833. PMID: 21640890.

21. Kim SJ, Choi TH, Baik HS, Park YC, Lee KJ. Mandibular posterior anatomic limit for molar distalization. Am J Orthod Dentofacial Orthop. 2014; 146:190–197. PMID: 25085302.

22. Lee KJ, Joo E, Kim KD, Lee JS, Park YC, Yu HS. Computed tomographic analysis of tooth-bearing alveolar bone for orthodontic miniscrew placement. Am J Orthod Dentofacial Orthop. 2009; 135:486–494. PMID: 19361735.

23. Jeong GM, Sung SJ, Lee KJ, Chun YS, Mo SS. Finite-element investigation of the center of resistance of the maxillary dentition. Korean J Orthod. 2009; 39:83–94.

24. Sung EH, Kim SJ, Chun YS, Park YC, Yu HS, Lee KJ. Distalization pattern of whole maxillary dentition according to force application points. Korean J Orthod. 2015; 45:20–28. PMID: 25667914.

25. Shafiee R, Korn EL, Pearson H, Boyd RL, Baumrind S. Evaluation of facial attractiveness from end-of-treatment facial photographs. Am J Orthod Dentofacial Orthop. 2008; 133:500–508. PMID: 18405813.

26. Yamada K, Kuroda S, Deguchi T, Takano-Yamamoto T, Yamashiro T. Distal movement of maxillary molars using miniscrew anchorage in the buccal interradicular region. Angle Orthod. 2009; 79:78–84. PMID: 19123698.

27. Proffit WR. The third stage of comprehensive treatment: finishing. In : Proffit WR, Fields HW, Sarver DV, editors. Contemporary orthodontics. 5th ed. St. Louis: Elsevier Health Sciences;2014. p. 596–597.
28. Murakami T, Yokota S, Takahama Y. Periodontal changes after experimentally induced intrusion of the upper incisors in Macaca fuscata monkeys. Am J Orthod Dentofacial Orthop. 1989; 95:115–126. PMID: 2916468.

29. Melsen B. Tissue reaction following application of extrusive and intrusive forces to teeth in adult monkeys. Am J Orthod. 1986; 89:469–475. PMID: 3459360.

30. Han G, Huang S, Von den Hoff JW, Zeng X, Kuijpers-Jagtman AM. Root resorption after orthodontic intrusion and extrusion: an intraindividual study. Angle Orthod. 2005; 75:912–918. PMID: 16448231.
31. Choi YJ, Kim KH, Lee KJ, Chung CJ, Park YC. Radiographic evaluations of molar intrusion and changes with or without retention in rats. Angle Orthod. 2011; 81:389–396. PMID: 21261480.

32. Chung CJ, Choi YJ, Kim KH. Approximation and contact of the maxillary central incisor roots with the incisive canal after maximum retraction with temporary anchorage devices: Report of 2 patients. Am J Orthod Dentofacial Orthop. 2015; 148:493–502. PMID: 26321347.

Figure 4
Posterior anatomic limit for total distalization. A and B, The available space at the maxillary tuberosity distal to the second molars, and the available space between the mandibular second molar and the anterior border of the ramus in the sagittal plane; C and D, the available space between the second molar crown to the anterior border of the ramus and between the root to the inner lingual cortex of the mandible in the axial plane.
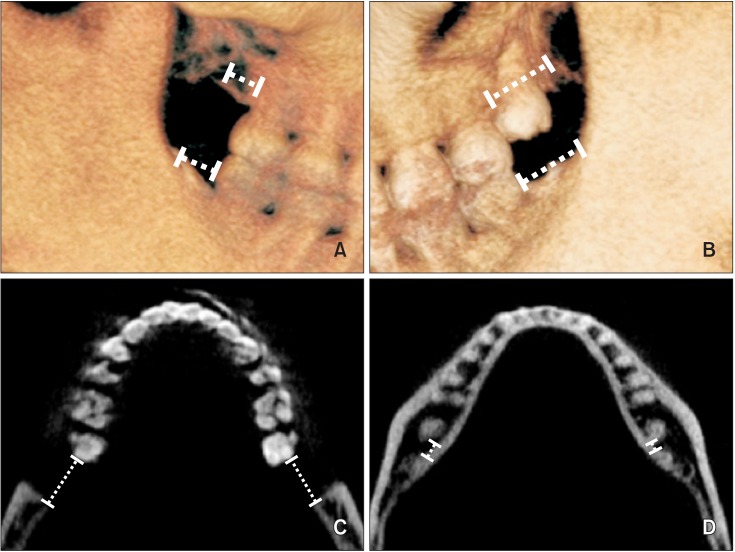
Figure 5
Biomechanical diagram and intraoral photographs. A, Line of force passing through the center of resistance (CR); B and C, dual miniscrews used for total intrusion and distalization of the maxillary arch; D and E, additional miniscrews inserted in the mandible for total distalization of the mandibular arch. F and G, Intraoral photographs before and after gingivoplasty.
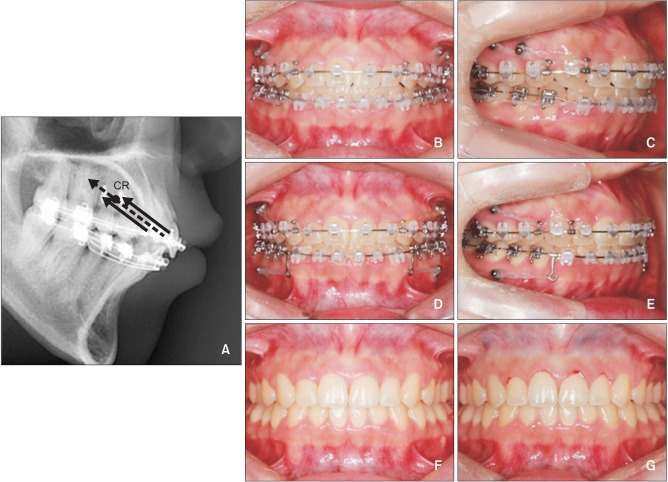
Figure 10
Three-dimensional cone-beam computed tomography superimposition to the cranial base. A, Sagittal cut near the midsagittal plane showing the mesial margins of the maxillary right central incisors. Incisal intrusion and distalization along with the changes in the lips are noted. Black, initial; white, final. B and C, Sagittal cut along the posterior arch form connecting the midroot portion of each tooth showing the movement of the maxillary and mandibular posterior teeth. Translation of the maxillary molars and the distal tip of the mandibular molars are noted. Black solid line, initial; white dotted line, final.
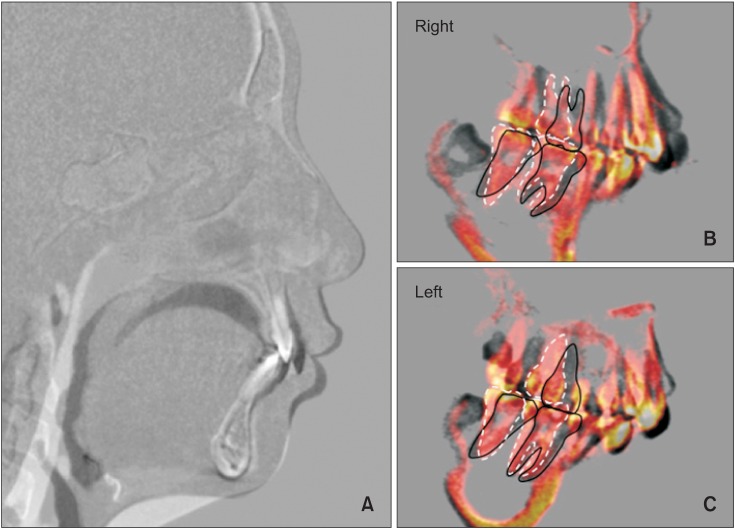
Figure 11
Changes in the arch form and tooth position following treatment. Axial cuts were made at the mid-crown level and midroot level before and after treatment. Black, initial; white, final.
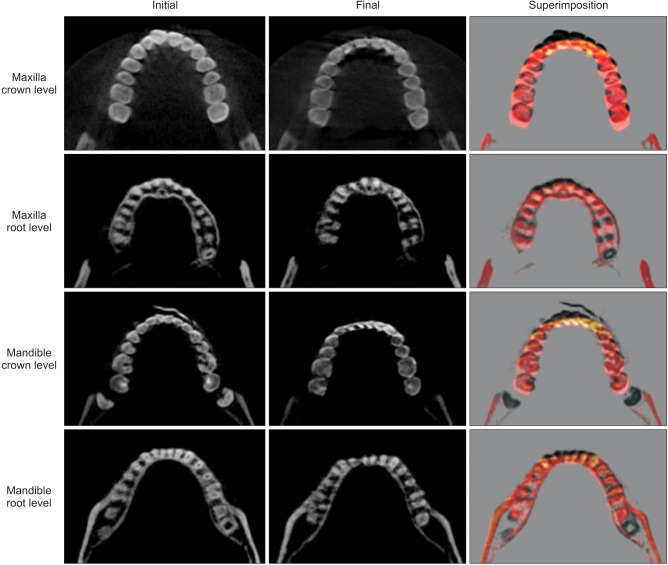
Figure 12
Three-dimensional cone-beam computed tomography superimposition of the temporomandibular joint. No distinct changes in condylar position are noted.
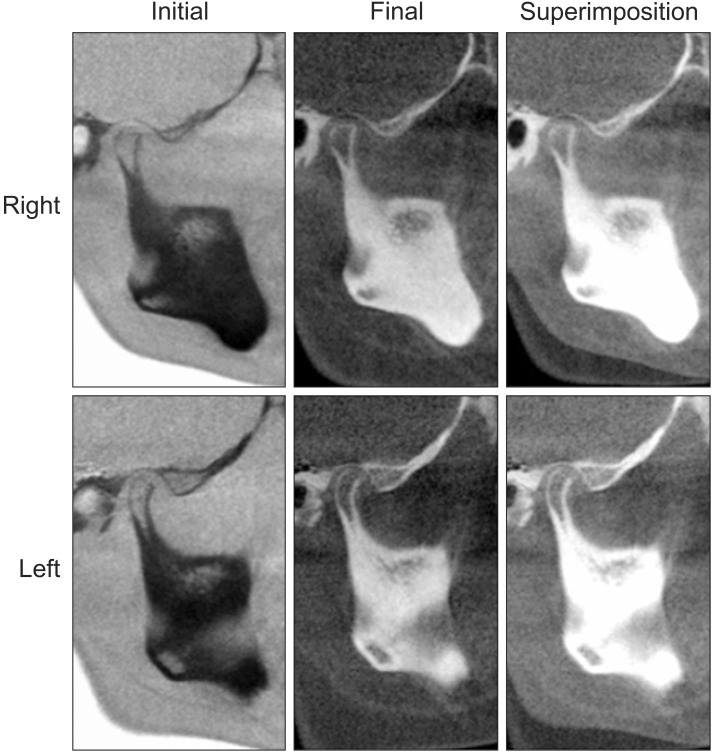
Figure 13
Changes in the central incisors and the surrounding alveolar housing. Mild root blunting is noted, but the incisors are within their biological boundaries after treatment.
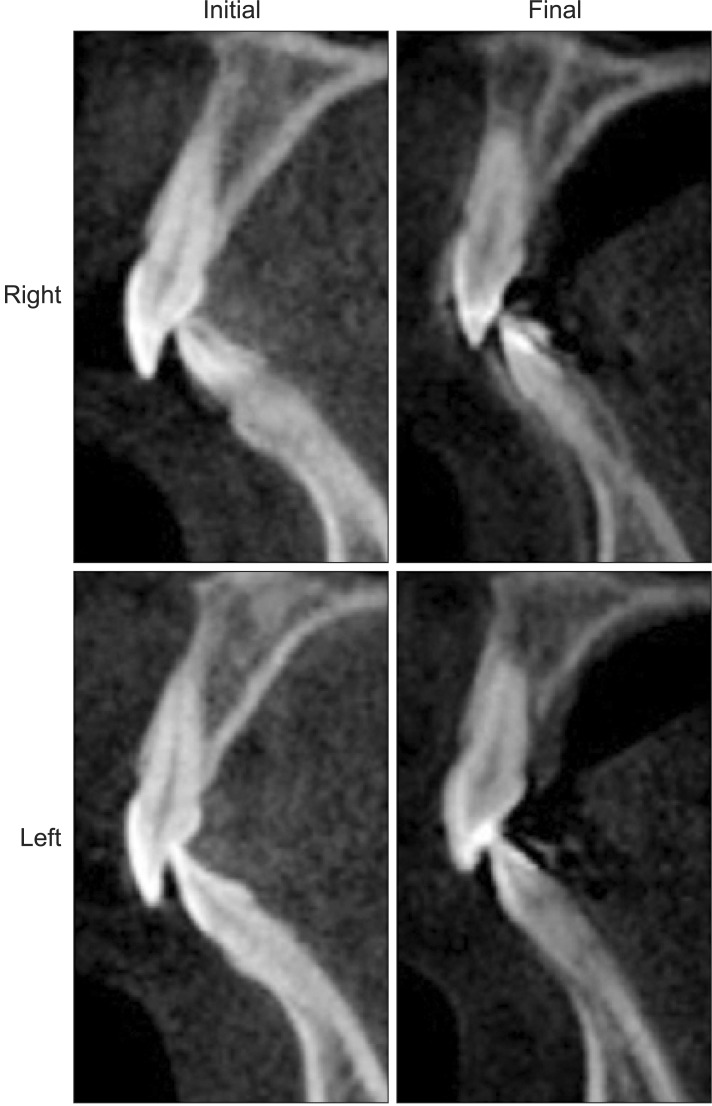
Figure 15
Cephalometric superimposition at debonding and after 15 months of follow-up. Black, final; red, retention.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download