Abstract
Fusion of teeth is a developmental anomaly. It occurs at the stage of tooth formation, which determines the shape and size of the tooth crown, when one or more teeth fuse at the dentin level during the morphodifferentiation of the dental germs. Such teeth show macrodontia and may cause crowding, as well as esthetic and endodontic problems. In this article, we report a rare case of a maxillary central incisor fused to a supernumerary tooth showing labial and palatal talon cusps, which was orthodontically moved across the midpalatal suture. A 13-year-old Caucasian boy sought treatment for the unesthetic appearance of his maxillary central incisor and anterior crowding. He was rehabilitated successfully via a multidisciplinary approach involving orthodontic, nonsurgical endodontic, periodontal, and prosthodontic treatments. After a 26-month treatment period, the patient's macroesthetics and microesthetics were improved. The overall improvement of this macrodontic tooth and its surrounding tissues through multidisciplinary treatment was documented using cone-beam computed tomography.
Dental developmental anomalies are rare conditions that make orthodontic treatment complicated and difficult. Since such anomalies ensue from the morpho-differentiation stage of tooth development, they can affect tooth size, shape, and structure.1
Fusion is a developmental anomaly defined as the union of two adjacent tooth germs at the dentin level. These teeth show macrodontia with or without talon cusps. Their root canals may be separated or shared. They may also affect the total number of teeth according to whether they fuse with a normal or supernumerary tooth.234 A talon cusp is a cusp-like structure usually projecting from the cingulum area; it is sometimes located on the labial surfaces of the maxillary or mandibular anterior teeth. It can be composed of enamel, dentin, and pulpal tissue. The talon cusp is called so because of its similarity in shape to an eagle's talon.56
The etiology of fused teeth remains unclear. A possible cause has been reported to be physical force or pressure compressing the developing tooth buds together. Trauma, genetic and environmental influences are considered cofactors affecting tooth fusion. Fused teeth could also be an accompanying symptom of some syndromes such as chondroectodermal dysplasia and achondrodysplasia.5
The prevalence of fusion anomalies varies in different societies. According to a study conducted in the Turkish population, the prevalence of fusion was found to be 0.23%, and the maxillary lateral incisors were the most commonly affected teeth.7
The maxillary anterior region is the most important region affecting a patient's smile and dental esthetics.8 Fused teeth usually have a wider mesiodistal dimension than do normal teeth, and they mostly appear in the anterior region of the maxilla.9 In some cases, these macrodontic teeth may need to be incorporated into the orthodontic treatment plan instead of removing them. In order to achieve esthetic success in these cases, a multidisciplinary treatment approach should be considered.10111213
Tooth movement through the midpalatal suture (MPS) may be needed during orthodontic treatment for obtaining an appropriate dental midline and thereby achieving a good esthetic goal. Animal studies and case reports have shown that moving the maxillary incisors across the MPS is biologically possible and can be performed using orthodontic treatment.14151617 However, to the best of our knowledge, no case report has documented this type of tooth movement performed on fused teeth.
Generally, fused teeth are asymptomatic. Moreover, they do not require root canal treatment unless a hemisection is planned, or unless they show pulp necrosis due to caries or pulpal anastomosis.181920
The aim of this case report was to present the management of a fused maxillary central incisor with labial and palatal talon cusps that was moved through the MPS to obtain an appropriate dental midline by using a multidisciplinary approach.
A 13-year-old Caucasian boy visited Department of Orthodontics of Faculty of Dentistry, the Ege University for orthodontic evaluation. His chief complaints were a large front tooth appearance when he smiled and crowding of the maxillary anterior teeth. He and his family did not report any medical problems. He was in good general health and had no history of major systemic disease.
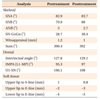
An initial extraoral examination showed that he had a symmetrical face on frontal view. He presented no gingival display when smiling. However, a lower dental midline deviated to the right in relation to the facial midline. On lateral view, he showed a straight profile (Figure 1).
Intraoral and dental cast examinations showed an Angle Class II relationship on the right side and an Angle Class I relationship on the left side (Figure 2). Both the right and left canines showed an Angle Class II relationship. The right canine was in infraocclusion, and the lower dental midline was deviated 2 mm to the patient's right. The maxillary arch had a U-shaped form. The upper left central incisor was rotated and the upper right central incisor was fused to a supernumerary tooth representing a wide mesiodistal dimension. The mandibular arch was U-shaped with minimal crowding. The periodontal hygiene status was moderate.
Panoramic radiography revealed no root anomalies (Figure 3). Moreover, ongoing root formation of the upper and lower second molars and developing third molar buds were evident. Cone-beam computed tomography (CBCT) was used to evaluate the complex root canal morphology of the fused teeth and the anatomy of the surrounding tissues (Figure 4).21
The treatment objectives for this patient were to achieve a stable occlusion, to restore esthetics and function in the anterior region, and to correct the molar and canine Class II relationships. A multidisciplinary treatment approach was chosen for this patient because of the benefits offered by specialist medical care. The treatment was supported by an orthodontist, an endodontist, a periodontist, and a prosthodontist. The orthodontist had to collaborate with the other specialists to ensure treatment success. The orthodontist aimed to establish a harmonious facial profile and physiologic occlusion. Initially, the crowding would be addressed using fixed orthodontic appliances, followed by the extraction of the over-rotated left central incisor, which had a small mesiodistal width, to obtain enough space for two central incisors readily existing in the form of a single macrodontic (fused) tooth. The coincidence of upper and lower dental midlines would be achieved by the movement of the macrodontic incisor through the MPS. The endodontist aimed to eliminate the complication of pulpal reactions during the prosthodontic preparation of the tooth, whereas the periodontist aimed to maintain periodontal health during the treatment and to reshape the gingival contour around the macrodontic central incisor to form two individual gingival margins. Finally, the prosthodontist aimed to provide esthetics in the anterior region and guide the anterior movement of the mandible by providing a double-crown restoration.
The first option consisted of extracting the macrodontic maxillary right central incisor, aligning the teeth via orthodontic treatment, implant placement for the maxillary right central incisor, and a cosmetic restorative preparation for the small left central incisor. This option was not preferred because of the patient's young age, since the patient would have to wait a long time until implant placement.22
The second option consisted of extracting the fused maxillary right central incisor, aligning the teeth orthodontically, and preparing a crown and bridge work for the maxillary right central incisor. This option was also not desirable because of the risk of bone resorption in the alveolar crest due to extraction and the ongoing dental development in the young patient.23
The third option was first to perform hemisection of the fused incisor, with root canal treatment because of the manifestation of pulpal anastomosis, and start orthodontic treatment. This option was not chosen because the macrodontic tooth was vital and asymptomatic, and because root canal treatment was not essential at the beginning of treatment.
The fourth alternative was to extract the left rotated central incisor because of its small anatomic size and a tendency to relapse,24 to perform orthodontic treatment including the movement of the fused teeth through the MPS, and to build a prosthetic double-crown restoration. This was the option chosen for the young patient in order to avoid a dental implant or a fixed crown and bridge restoration in the maxillary anterior region. The patient and his family granted approval for the treatment plan and publication of the treatment records.
After full eruption of the second molars, when the patient was 14 years old, we decided to start the treatment. Initially, the patient was sent to a periodontist to undergo oral hygiene control and education. After achieving a good hygiene level, the patient was referred back to the orthodontic department. Before the fixed orthodontic appliances were bonded, the labial talon cusp was gradually ground to have a flat labial surface.
Damon Q 0.022-inch (Ormco Corp., Orange, CA, USA) passive self-ligating brackets were used for this patient. The brackets were first placed on the maxillary teeth. Two central incisor brackets were used for the fused right central incisor. A 0.014-inch preformed Damon Copper NiTi archwire (Ormco Corp.) was inserted to initiate tooth movement, leveling, and transverse arch form development (Figure 6A). Two months after the first appointment, the brackets for the mandibular arch were placed and posterior bite turbos were added to the molars to raise the bite and ease crowding relief. A preformed 0.014-inch Damon Copper NiTi archwire (Ormco Corp.) was likewise used as the first arch to align the mandibular teeth.
After 3 months of treatment, a 0.016-inch Damon Copper NiTi wire (Ormco Corp) was used as a second archwire in both the upper and lower jaws for ongoing alignment. In accordance with the treatment plan, the left central incisor was extracted. Two months later, a 0.014 × 0.025-inch preformed Damon Copper NiTi wire (Ormco Corp.) was inserted in both the jaws to initiate work on torque, root angulations, and rotation control, as well as to continue transverse arch form development. After another 3 months, a 0.018 × 0.025-inch preformed Damon Copper NiTi archwire (Ormco Corp.) was used in the upper and lower arches to prepare for the insertion of the working stainless steel (SS) wire. At this stage, a light-force open NiTi coil spring was used for moving the fused central incisors through the MPS.
After 15 months of treatment, a 0.019 × 0.025-inch SS wire (Ormco Corp.) was inserted inthe maxillary arch. The movement of the fused teeth through the MPS was completed by continuing the use of the open coil springs and low forces (Figure 6B). After positioning the fused teeth in the correct position (center of the midline), crimpable hooks were inserted to the same archwire for enabling the use of Class II elastics. A 0.019 × 0.025-inch SS wire (Ormco Corp) was inserted to the mandibular arch to maintain the integrity of the arch during anteroposterior Class II correction. Class II intermaxillary elastics (5/16-inch, 6 oz) were used for correcting the dental Class II relationship. The patient used the elastics for 4 months (Figure 6C).
The objectives related to orthodontics, which included solving the crowding, correction of the Class II relationship, moving the fused teeth through the MPS, and obtaining enough space for two incisors, had been achieved after 20 months of treatment. Electrical testing was performed to ensure the fused central macrodontic incisor was still vital after the movement through the MPS. After removing the upper appliance, the patient was sent to the periodontist for gingivoplasty of the upper incisor. The periodontist reshaped the gingival tissue to form an interdental papilla and performed an upper frenectomy. An immediate temporary composite laminate veneer restoration was performed on the labial surface to support the reshaped gingival tissues. We first tried applying the temporary composite laminate, but the outcome was assessed by the patient as “very unesthetic” because the built crown was triangular and gingivectomy could not be performed esthetically. This was the reason we preferred a prosthetic restoration, despite the risk of passive eruption. After the gingiva had healed, the patient was sent to the prosthodontist for the preparation of the permanent prosthetic restoration.
During the preparation of the atypical macrodontic tooth, a complication occurred. The pulp chamber was perforated. Hence, the patient was sent to an endodontist who performed root canal treatment of the two fused teeth that shared the pulp tissue.
After the completion of the root canal treatments, the permanent prosthetic restoration was applied (Figure 6D). For retaining the maxillary teeth, a vacuum-formed retainer (VFR) was used. During the same appointment, the lower orthodontic appliances were removed and a fixed lingual retainer was placed. A VFR was also used to support the retention in the mandible.
The post-treatment facial photographs showed an improvement of facial esthetics. The patient achieved macroesthetics and microesthetics (Figure 7). A normal overjet and overbite relationship were evident. The dental Class II relationship was corrected and a stable occlusion was obtained (Figure 8). The macrodontic fused central incisor became “two” central incisors with normal size and shape. The midline discrepancy was corrected. Normal incisal and canine guidance was also achieved. The gingival tissue around the fused teeth was healthy, and the patient was advised on maintaining oral hygiene. Post-treatment panoramic radiography showed excellent root parallelism (Figure 9). Post-treatment CBCT imaging showed that a successful movement of the fused teeth towards the midline was achieved by a “slippage phenomenon” of the MPS in the lateral direction (Figure 10). No sign of root resorption was evident. Maxillary retention was provided by a VFR, and mandibular retention was achieved with a canine-to-canine bonded fixed retainer in combination with a VFR. Although not included in the treatment plan, the root canal treatment was successful. Facial and dental esthetics of the young adult was maintained during the 1-year retention period (Figure 11). The patient remained symptom-free during the post-treatment period.
Developmental anomalies most frequently occur in the maxillary incisor region and cause esthetic and dental problems.1925 Labeling them as anomalies may be difficult. Fused teeth are generally referred to as macrodontia, megadontia, or double teeth.3
These dental abnormalities occur at different rates in different populations. In the Turkish society, the prevalence of fusion was found to be 0.23%, and maxillary lateral incisors were the most commonly affected teeth.7 In Jordanian adult patients, fusion was found to have a prevalence of 0.19%, and maxillary central incisors were the most commonly affected teeth.26
To our knowledge, this case report is the first on a permanent maxillary “double-tooth” with labial and palatal talon cusps that has been moved through the MPS. Double teeth usually are asymptomatic but are potentially problematic because their mesiodistal dimension is wider than that of normal incisors. Because of the complex structures of fused teeth, a multidisciplinary approach is mostly required for their rehabilitation.
The 13-year-old patient had fused teeth in the maxillary anterior region, upper and lower crowding, and a dental Class II relationship. The over-rotated, mesiodistally narrow tooth in the anterior region also had a tendency to relapse.24 To avoid cosmetic restoration, long-term retention, or an invasive surgery such as supracrestalfiberotomy, the small left central incisor was extracted. If the fused teeth had been extracted, a dental implant insertion or prosthodontic treatment (fixed bridge or removable partial denture) for replacing the space would have been essential. Considering the esthetic importance of the anterior region, the patient's age as well as hard- and soft-tissue conditions around the space must be considered before deciding on any treatment option.2227
Careful clinical and radiographic examinations should be performed for optimal treatment planning. Normal dental radiographs may not be sufficient for proper diagnosis and treatment planning. In a specific case like the current one, CBCT data could provide more details about the location of the moved incisors; root canals; root resorption of the teeth involved; surrounding tissues; and anatomic structures like the incisive foramen, nasopalatine canal, and, specifically, the MPS.21 The incisive foramen is the palatal orifice of the nasopalatine canal located at the MPS. The nasopalatine nerve and the end branches of the nasopalatine artery are located in the nasopalatine canal.28 The incisive papilla and labial frenulum are related soft tissues of the MPS. Moving a tooth through the suture could affect the course of the canal and its content. Therefore, pretreatment and post-treatment CBCT images were used to observe the relative position of the macrodontic incisor and the MPS.
Case reports and studies have shown that if the suture is mineralized, the tooth moves normally. If the suture is not mineralized, however, the MPS undergoes distortion in the same direction as that of tooth movement; moreover, the connective tissue of the suture is incorporated into the periodontal ligament.151617 We termed the current condition as a “slippage phenomenon” of the suture in order to rationalize the terminology. CBCT imaging revealed that the tooth movement had little or no effect on the position of the incisive foramen. Tooth movement affected the soft tissues, such as the buccal mucosa and periodontal tissues, but not the hard palate.
Dental abnormalities such as fusion can cause functional and esthetic problems. A multidisciplinary approach, including orthodontics, periodontics, endodontics, and prosthodontics, could be used to achieve successful and satisfying treatment results. In this case, the intraoral rehabilitation in conjunction with the improvement of facial esthetics contributed enormously to the self-confidence of the young, adolescent patient.
Figures and Tables
Figure 6
Treatment progress. A, Leveling and aligning phase of treatment with 0.014-inch preformed Damon Copper NiTi archwire. B, Movement of the fused teeth through the midpalatal suture by using a 0.019 × 0.025-inch stainless steel wire and open coil springs. C, Class II intermaxillary elastics (5/16-inch, 6 oz) are used for correcting the dental Class II relationship. D, Prosthetic restoration application after bracket removal.

ACKNOWLEDGEMENTS
The authors thank Dr. Mehmet Emin Kaval, Dr. Nejat Nizam, and Dr. Muharrem Erhan Comlekoğlu for their priceless help with the endodontic, periodontal, and prosthetic approaches in this case.
References
1. Brook AH, Winter GB. Double teeth. A retrospective study of ‘geminated’ and ‘fused’ teeth in children. Br Dent J. 1970; 129:123–130.

2. Levitas TC. Gemination, fusion, twinning, and concrescence. J Dent Child (Chic). 1965; 32:93–100.
3. Foster TD. Fusion and duplication: orthodontic treatment of a developmental anomaly. Eur J Orthod. 1987; 9:240–242.

4. Sivolella S, Bressan E, Mirabal V, Stellini E, Berengo M. Extraoral endodontic treatment, odontotomy and intentional replantation of a double maxillary lateral permanent incisor: case report and 6-year follow-up. Int Endod J. 2008; 41:538–546.

5. Ekambaram M, Yiu CK, King NM. An unusual case of double teeth with facial and lingual talon cusps. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 105:e63–e67.

6. Mitchell WH. Letter to the editor. Dent Cosmos. 1892; 34:1036.
7. Altug-Atac AT, Erdem D. Prevalence and distribution of dental anomalies in orthodontic patients. Am J Orthod Dentofacial Orthop. 2007; 131:510–514.

8. Zachrisson BU. Esthetics in tooth display and smile design. In : Nanda R, editor. Biomechanics and esthetics strategies in clinical orthodontics. Philedelphia: Elsevier Saunders;2005. p. 110–130.
9. Primosch RE. Anterior supernumerary teeth--assessment and surgical intervention in children. Pediatr Dent. 1981; 3:204–215.
10. Demircioglu Guler D, Sen Tunc E, Arici N, Ozkan N. Multidisciplinary management of a fused tooth: a case report. Case Rep Dent. 2013; 2013:634052.

11. Sammartino G, Cerone V, Gasparro R, Riccitiello F, Trosino O. Multidisciplinary approach to fused maxillary central incisors: a case report. J Med Case Rep. 2014; 8:398.

12. Ozden B, Gunduz K, Ozer S, Oz A, Otan Ozden F. The multidisciplinary management of a fused maxillary central incisor with a talon cusp. Aust Dent J. 2012; 57:98–102.

13. Garattini G, Crozzoli P, Brenna F. Bilateral dental fusion of the upper central incisors: a multi-disciplinary approach. J Esthet Dent. 1999; 11:149–154.

14. Follin M, Ericsson I, Thilander B. Orthodontic movement of maxillary incisors through the midpalatal suture area--an experimental study in dogs. Eur J Orthod. 1984; 6:237–246.

15. Bosio JA, Bradley TG, Hefti AF. Moving an incisor across the midline: a treatment alternative in an adolescent patient. Am J Orthod Dentofacial Orthop. 2011; 139:533–543.

16. Pair J. Movement of a maxillary central incisor across the midline. Angle Orthod. 2011; 81:341–349.

17. Garib DG, Janson G, dos Santos PB, de Oliveira Baldo T, de Oliveira GU, Ishikiriama SK. Orthodontic movement of a maxillary incisor through the midpalatal suture: a case report. Angle Orthod. 2012; 82:370–379.

18. Indra R, Srinivasan MR, Farzana H, Karthikeyan K. Endodontic management of a fused maxillary lateral incisor with a supernumerary tooth: a case report. J Endod. 2006; 32:1217–1219.

19. Yanikoğlu F, Kartal N. Endodontic treatment of a fused maxillary lateral incisor. J Endod. 1998; 24:57–59.
20. Tsurumachi T, Kuno T. Endodontic and orthodontic treatment of a cross-bite fused maxillary lateral incisor. Int Endod J. 2003; 36:135–142.

21. Kato H, Kamio T. Diagnosis and endodontic management of fused mandibular second molar and paramolar with concrescent supernumerary tooth using cone-beam CT and 3-D printing technology: a case report. Bull Tokyo Dent Coll. 2015; 56:177–184.

22. Thilander B, Odman J, Lekholm U. Orthodontic aspects of the use of oral implants in adolescents: a 10-year follow-up study. Eur J Orthod. 2001; 23:715–731.

23. Misawa M, Lindhe J, Araújo MG. The alveolar process following single-tooth extraction: a study of maxillary incisor and premolar sites in man. Clin Oral Implants Res. 2016; 27:884–889.

24. Naraghi S, Andrén A, Kjellberg H, Mohlin BO. Relapse tendency after orthodontic correction of upper front teeth retained with a bonded retainer. Angle Orthod. 2006; 76:570–576.
25. Brook AH. A unifying aetiological explanation for anomalies of human tooth number and size. Arch Oral Biol. 1984; 29:373–378.

26. Hamasha AA, Al-Khateeb T. Prevalence of fused and geminated teeth in Jordanian adults. Quintessence Int. 2004; 35:556–559.
27. Cardoso JA, Almeida PJ, Fischer A, Phaxay SL. Clinical decisions for anterior restorations: the concept of restorative volume. J Esthet Restor Dent. 2012; 24:367–383.

28. Netter FH. Atlas of human anatomy. 6th ed. Philadelphia: Saunders/Elsevier Inc.;2014.




 PDF
PDF ePub
ePub Citation
Citation Print
Print











 XML Download
XML Download