Abstract
The purpose of this article is to introduce a simple appliance that uses a setup model and a nickel-titanium (Ni-Ti) wire for correcting the mesial rotation and drift of the permanent maxillary first molar. The technique involves bonding a Ni-Ti wire to the proper position of the target tooth on a setup model, followed by the fabrication of the transfer cap for indirect bonding and its transfer to the patient's teeth. This appliance causes less discomfort and provides better oral hygiene for the patients than do conventional appliances such as the bracket, pendulum, and distal jet. The treatment time is also shorter with the new appliance than with full-fixed appliances. Moreover, the applicability of the new appliance can be expanded to many cases by using screws or splinting with adjacent teeth to improve anchorage.
Although conventional brackets have proven effective in the migration of teeth to desired positions, the use of these brackets causes oral discomfort and makes hygiene control difficult. Young patients with poor oral hygiene compliance have a high risk of developing labial white spot lesions. For such patients, partial treatment with a nickel-titanium (Ni-Ti) wire could be used to minimize the otherwise long treatment time when using conventional brackets. In patients with mixed dentition, the space required for premolar eruption is often lost because of the premature loss of the primary second molar followed by mesial drift along with mesial-in rotation of the permanent first molar. The transpalatal arch, distal jet, and pendulum could be used in patients with partially localized misalignment of teeth. However, such complicated devices often cause irritation and discomfort to patients while having detrimental effects on their oral hygiene.1234567 Furthermore, treatments with such removable appliances require patient compliance. This article introduces an alternative technique that uses a single Ni-Ti wire to improve and correct the position of the mesially drifted first molar.
The patient was a 9-year-old girl with the chief complaint of impacted maxillary left second premolar. The initial examination revealed she had a convex profile. Clinical and radiographic examinations showed mesial drift along with mesial-in rotation of the maxillary first molar with impacted second premolar due to insufficient space. As a result, she had class II molar relationship and class III canine key on the left side. Overbite was 2 mm, and overjet was 1.5 mm. The mandibular anterior teeth showed mild crowding. Lateral cephalometric analysis revealed skeletal class I malocclusion (ANB = 3.2°). The long axis of the maxillary and mandibular incisors was within the normal range.
Derotation of the maxillary left first premolar and maxillary left first molar was needed to gain sufficient space for the eruption of the maxillary left second premolar. A Ni-Ti molar derotation spring was fabricated on an ideal setup model to derotate the maxillary left first premolar and maxillary left first molar and to anticipate the eruption of the maxillary left second premolar. The appliance was delivered clinically for derotation of the rotated posterior teeth, and the natural eruption of the maxillary left second premolar was monitored.
Partial teeth alignment and space gaining by bracket appliance and wire has been conventionally used. Thus, one can use opencoil spring to gain space between brackets similary as this case. Also, distal jet or pendulum including opposite arch can be used to reinforce anchorage of the anterior semgment. However, in this case they were not considered as an option because such appliances are bulky and unfavorable for hygiene control and the anterior teeth should be protracted.
In the initial model, the target teeth were set up in an ideal position after considering the relationships with the opposing teeth (Figure 1). A 0.012-inch Ni-Ti sectioned wire (Ni-Ti®; Ormco™, Glendora, CA, USA) was passively bonded onto the setup model teeth by using a light-cured resin, which functioned as a customized base (Figure 2). The resin was also used to fabricate the transferring resin jig (Figures 3 and 4). Microetching was applied on the surface of the customized resin base after carefully removing the molar derotation and distalization spring from the setup model.
In order to regain the space for the maxillary second premolar, the Ni-Ti molar derotation and distalization spring fabricated on the setup model was transferred onto the patient's teeth. A safety ligature tie was then implemented to prevent accidental ingestion or aspiration of the appliance (Figure 5).
Initially, the maxillary first premolar and maxillary first molar were reciprocally derotated to gain space. After 6 weeks of treatment, the maxillary first premolar was derotated with complete closure of the space distal to the maxillary canine. Thereafter, the six maxillary anterior teeth and the maxillary first premolar were splinted using a Triple Flex wire (Triple Flex®; Ormco™). The eruption space for the maxillary second premolar was successively regained after 2.5 months without spring reactivation during the monthly check-ups. The total treatment period was 2.5 months.
Superimposition of the initial and final cast models by using the palatal rugae as the reference area on a three-dimensional reverse modeling software (Rapidform 2002; INUS Technology, Seoul, Korea) revealed that the buccal and palatal cusps of the maxillary first premolar moved mesially 4.0 mm and 1.6 mm, respectively, with an 18° mesial-in rotation in reference to the line drawn between the buccal and palatal cusps. As for the maxillary first molar, the mesiobuccal and mesiopalatal cusps moved distally 4.8 mm and 2.8 mm, respectively, with a 22° mesial-out rotation in reference to the line drawn between the mesiobuccal and mesiopalatal cusps. The clinical outcome is shown in Figures 5 and 6.
As seen in this case report, maxillary molar derotation is of utmost significance in space regaining. Insufficient space was observed for the eruption of the maxillary second premolar on the maxillary left quadrant because of what appeared to be mesial drift of the maxillary first molar. However, more accurately, it was mesialin rotation. The maxillary first molar is often rotated around the palatal root, which is its largest root. Such unwanted molar rotations have been corrected with massive, bulky appliances like the transpalatal arch, distal jet, pendulum, and fixed appliances, albeit with unwanted detrimental effects on oral hygiene. In addition, treatment using fixed appliances such as brackets also hinders oral hygiene control, thereby unintentionally leaving patients in poor oral health.89 The aim of this treatment was to achieve a similar treatment outcome rather than better results with a simpler appliance than the ones used in conventional treatment methods.
Moreover, the bent Ni-Ti spring used in the current approach exerts continuous elastic recovery force on the teeth, thereby allowing for a desirable amount of tooth movement with a single setup of the appliance. Both ends of the round wire are bent to prevent unwanted rotation in the resin base. Only a single Ni-Ti wire was used to regain the space for proper eruption of the maxillary second premolar. As such, this simple treatment was possible because of the customized appliance fabricated to move the target tooth in the desired direction based on the setup model.101112 If needed, the wire could be replaced with a new Ni-Ti spring fabricated using the overcorrected setup model or one fabricated using a thicker wire. However, the treatment could be successfully completed with a one-time setup appliance without additional reactivation. If the second molar had erupted, more time would have been required for distalization, and anchorage loss of the anterior segment could have occurred.10 In such cases, additional reactivation of the appliance or anchorage reinforcement of the anterior segment may become necessary.
Although such partial orthodontic treatment requires anchorage preparation, simple wire-bonding was used without miniscrew anchorage in this case. This resulted in mesial movement of its anterior anchorage teeth and deviation of the maxillary midline to the right (Figure 7). Such movement was not initially intended, but since it produced a positive effect, anterior movement was allowed under monitoring. Therefore, strict monitoring of unwanted tooth movement as well as anchorage reinforcement may be necessary depending on the case. Considering the age of the patient, anchorage reinforcement with microscrews had certain limitations. Thus, anchorage loss was an unintentional complication due to the selection of tooth-borne anchorage. The essence of this approach is to apply partial orthodontic treatment as an interim measure to induce the eruption of impacted teeth. Leveling and alignment of the full dentition could be considered subsequently.
The current appliance did not include a rigid main arch wire; hence, it was prone to cause unwanted tooth movement. For example, if one applied the molar derotation spring only on the buccal side, more space would be gained on the buccal side than on the palatal side. Thus, continuous monitoring and orthodontic approach from the palatal side may be necessary if excessive rotation occurs on the buccal side. Moreover, it would be safer to fabricate new appliances at many steps along the orthodontic movement rather than manufacturing just one appliance with overcorrection.
Disocclusion of the distobuccal cusp of the first molar was observed at the end of the treatment. To prevent excessive distal tipping of the first molar, a customized appliance was fabricated on the setup model of an upright first molar to create adequate movement. The maxillary left first molar was more distally tipped after treatment than in the setup model (Figure 8). Nonetheless, the tooth axis was appropriate in comparison with adjacent teeth during the 18-month retention period, as can be seen in Figures 5E and 6C. The improvement in the tooth axis may partly be due to the settling of the occlusion during the retention period.
Despite its benefits, the newly described appliance certainly has some drawbacks. As mentioned above, unwanted tooth movement can occur in the absence of sufficient anchorage preparation. Furthermore, a new appliance should be fabricated on a setup model if the original appliance partially falls off. However, this appliance has clear advantages over conventional brackets. The derotation spring causes less discomfort and may decrease the risk of white spot lesion development on tooth surfaces by improving oral hygiene. Treatment with a single Ni-Ti wire and a lingual fixed retainer makes the teeth less prone to plaque buildup and labial white spot lesions, and reduces the number of dental visits for supplemental reactivation.
This case illustrates the derotation and distalization of a mesially rotated and drifted first molar by using a single Ni-Ti wire spring fabricated on the setup model. This appliance causes less discomfort to the patient than does the bracket, pendulum, or distal jet. Compared to full-fixed appliances, the new appliance provides better oral hygiene during treatment and shortens the treatment time. To conclude, the derotation and distalization spring introduced in this article can be effectively used as a treatment option in cases in which derotation of adjacent teeth is required for space gaining. The treatment method would be more widely applicable if the anchorage is reinforced by using miniscrews or by splinting with adjacent teeth.
Figures and Tables
Figure 2
Fabrication of the nickel-titanium (Ni-Ti) spring with a customized resin base. Both ends of the Ni-Ti wire have been bent to prevent unwanted rotation in the resin base.

Figure 3
Fabrication of the transferring resin jig for the nickel-titanium spring with a customized resin base.

Figure 4
Precise application of the nickel-titanium spring with a customized resin base by transferring the resin jig.

Figure 5
Adequate space is gained through the derotation of the maxillary first premolar and maxillary first molar. A, Pretreatment; B, after 6 weeks; C, after 4 months; D, post-treatment (after 5 months); E, 18 months after treatment. The occlusal button seen in C is bonded for later use during orthodontic traction. However, traction was not applied because the tooth erupted spontaneously.

Figure 6
Comparison of the radiographs at A, pretreatment; B, post-treatment; and C, 18 months after treatment.

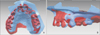
Figure 7
Three-dimensional superimposition of the pre-treatment (blue) and post-treatment (red) models. The models were scanned using the intraoral scanner (iTero™; Align Technology Inc., Santa Clara, CA, USA), and the models were superimposed using a three-dimensional reverse modeling software (Rapidform 2002; INUS Technology, Seoul, Korea). A, Occlusal view of the maxillary dentition; B, occlusal view of the left maxillary dentition; C, palatal view of the left maxillary dentition; D, buccal view of the left maxillary dentition.

References
1. Dahlquist A, Gebauer U, Ingervall B. The effect of a transpalatal arch for the correction of first molar rotation. Eur J Orthod. 1996; 18:257–267.

2. Bondemark L, Kurol J. Distalization of maxillary first and second molars simultaneously with repelling magnets. Eur J Orthod. 1992; 14:264–272.

3. Fontana M, Cozzani M, Caprioglio A. Non-compliance maxillary molar distalizing appliances: an overview of the last decade. Prog Orthod. 2012; 13:173–184.

4. Gurgel Jde A, Pinzan-Vercelino CR, Bramante FS, Rivera AP. Distalization of maxillary molars using a lever arm and mini-implant. Orthodontics (Chic.). 2013; 14:e140–e149.
5. Hourfar J, Ludwig B, Kanavakis G. An active, skeletally anchored transpalatal appliance for derotation, distalization and vertical control of maxillary first molars. J Orthod. 2014; 41:Suppl 1. S24–S32.

6. Chiu PP, McNamara JA Jr, Franchi L. A comparison of two intraoral molar distalization appliances: distal jet versus pendulum. Am J Orthod Dentofacial Orthop. 2005; 128:353–365.

7. Caprioglio A, Cafagna A, Fontana M, Cozzani M. Comparative evaluation of molar distalization therapy using pendulum and distal screw appliances. Korean J Orthod. 2015; 45:171–179.

8. Klukowska M, Bader A, Erbe C, Bellamy P, White DJ, Anastasia MK, et al. Plaque levels of patients with fixed orthodontic appliances measured by digital plaque image analysis. Am J Orthod Dentofacial Orthop. 2011; 139:e463–e470.

9. Wiechmann D, Gerss J, Stamm T, Hohoff A. Prediction of oral discomfort and dysfunction in lingual orthodontics: a preliminary report. Am J Orthod Dentofacial Orthop. 2008; 133:359–364.

10. Locatelli R, Bednar J, Dietz VS, Gianelly AA. Molar distalization with superelastic NiTi wire. J Clin Orthod. 1992; 26:277–279.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download