Abstract
Objective
Methods
Results
Figures and Tables
Figure 2
Landmarks for skeletal measurements. Maxilla (Mx) canting is the angle between the line connecting the bi-jugale (J) and the Frankfort horizontal plane (FHP) projected on the frontal plane. The ramal inclination is the angle between the line connecting the condylion (Co), the gonion (Go), and the FHP projected on the frontal plane. The ramal length is the distance between the Go and the Co. The mandibular (Mn) body length is the distance between Go and menton (Me).

Figure 3
Landmarks for the dental measurements. A and C, The maxillary and mandibular canine inclinations indicate the angle between the line connecting the cusp tip and the apex and Frankfort horizontal plane (FHP) projected on the frontal plane. B and D, The maxillary and mandibular first molar inclinations indicate the angle between the line connecting the central groove and the furcation and FHP projected on the frontal plane. (For better readability, these images show the best fit of the longitudinal axis of the bilateral canines and molars.)

Table 1
Sample characteristics at initial examination (n = 29)
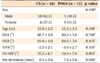
Values are presented as number (%) or mean ± standard deviation.
CS, Conventional orthognathic surgery; POGS, preorthodontic orthognathic surgery; SNA, angle of the lines connecting the sella, the nasion, and point A; SNB, angle of the lines connecting the sella, the nasion, and point B; ANB, angle of the lines connecting point A, the nasion, and point B; SN-MP, angle of the plane formed by the sella and the nasion to the mandibular plane formed by the gonion and the mention; Me, menton.
*Chi-square test, †Mann-Whitney U test, ‡independent t-test.
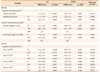
Table 2
Comparison of variables at T1

All measurements at T1 in both groups were tested with the independent t-test. Only 10 patients in the CS group had three-dimensional computed tomography scan at T0.
CS, Conventional orthognathic surgery; POGS, preorthodontic orthognathic surgery; SD, standard deviation; D, deviated; ND, nondeviated; diff., difference between deviated and nondeviated sides; Co, condylion; Go, gonion; Me, menton; Mx 3, maxillary canine; Mn 3, mandibular canine; FH, Frankfort horizontal plane; Mx 6, maxillary first molar; Mn 6, mandibular first molar.
*p < 0.05; †p < 0.01; ‡p < 0.001.
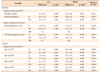
Table 3
Comparison of surgical changes between the two groups (T2 vs. T1)
CS, Conventional orthognathic surgery; POGS, preorthodontic orthognathic surgery; D, deviated; ND, nondeviated; diff., difference between deviated and nondeviated sides; Co, condylion; Go, gonion; Me, menton; FH, Frankfort horizontal plane; Mx 3, maxillary canine; Mn 3, mandibular canine; Mx 6, maxillary first molar; Mn 6, mandibular first molar.
Group comparisons were tested with the independent t-test; *p < 0.05; †p < 0.01; ‡p < 0.001.
§Positive and negative values indicate deterioration and improvement of maxilla canting, respectively.
∥Positive and negative values indicate lateral and mesial movement of ramus, respectively.
¶Positive and negative values indicate increase and decrease of measurements, respectively.
**Positive and negative values indicate buccally and lingually inclined, respectively.
††Positive and negative values indicate lingually and buccally inclined, respectively.
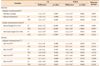
Table 4
Comparison of postsurgical changes between the two groups (T3 vs. T2)
CS, Conventional orthognathic surgery; POGS, preorthodontic orthognathic surgery; D, deviated; ND, nondeviated; diff., difference between deviated and nondeviated sides; Co, condylion; Go, gonion; Me, menton; FH, Frankfort horizontal plane; Mx 3, maxillary canine; Mn 3, mandibular canine; Mx 6, maxillary first molar; Mn 6, mandibular first molar.
Group comparisons were tested with the independent t-test; *p < 0.05; †p < 0.01.
‡Positive and negative values indicate deterioration and improvement of maxilla canting, respectively.
§Positive and negative values indicate lateral and mesial movement of ramus, respectively.
∥Positive and negative values indicate increase and decrease of measurements, respectively.
¶Positive and negative values indicate buccally and lingually inclined, respectively.
**Positive and negative values indicate lingually and buccally inclined, respectively.
Table 5
Comparison of total changes between the two groups (T3 vs. T0)
CS, Conventional orthognathic surgery; POGS, preorthodontic orthognathic surgery; D, deviated; ND, nondeviated; Co, condylion; Go, gonion; Me, menton; FH, Frankfort horizontal plane; Mx 3, maxillary canine; Mn 3, mandibular canine; Mx 6, maxillary first molar; Mn 6, mandibular first molar.
Group comparisons were tested with the independent t-test; *p < 0.05, †p < 0.01, §p < 0.001.
§Positive and negative values indicate deterioration and improvement of maxilla canting, respectively.
∥Positive and negative values indicate lateral and mesial movement of ramus, respectively.
¶Positive and negative values indicate increase and decrease of measurements, respectively.
**Positive and negative values indicate buccally and lingually inclined, respectively.
††Positive and negative values indicate lingually and buccally inclined, respectively.
Table 6
Comparison of variables at T3

CS, Conventional orthognathic surgery; POGS, preorthodontic orthognathic surgery; SD, standard deviation; D, deviated; ND, nondeviated; diff., difference between deviated and nondeviated sides; Co, condylion; Go, gonion; Me, menton; FH, Frankfort horizontal plane; Mx 3, maxillary canine; Mn 3, mandibular canine; Mx 6, maxillary first molar; Mn 6, mandibular first molar.
Group comparisons were tested by the independent t-test; *p < 0.05; †p < 0.01; ‡p < 0.001.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download