INTRODUCTION
Most patients seek orthodontic treatment for esthetic reasons,
1 although those with severe dentofacial deformities may also report functional problems.
2 Accordingly, malocclusions may have a significant impact on oral health-related quality of life (OHRQoL) and, particularly, on emotional and social wellbeing.
34 In addition to the nature and severity of malocclusions,
5 their type and location might play a part in this. For instance, significantly higher Child Perceptions Questionnaire (CPQ) scores have been reported for several dental anomalies located in the esthetic zone, including multiple missing teeth,
6 greater overjet, and anterior spacing.
7
Individuals with hyperdivergent facial types (or long faces) also have esthetically sensitive characteristics, with anterior open bite, gummy smile, and excessive lower facial height being common findings.
8 Specific features of the long face, such as anterior open bite, have been associated with greater impacts on OHRQoL.
9 However, few studies have investigated the relationship between OHRQoL and the hyperdivergent facial type as a distinct craniofacial anomaly. Individuals with hyperdivergent facial types are reported to have less attractive profiles,
1011 poorer masticatory performance, and a slower chewing rate than do normal or short-faced individuals.
12 These functional differences have been attributed to their lower bite force, which typically leads to greater muscular effort and associated rapid fatiguing.
12 Individuals with other facial morphologies may not necessarily experience this combination of esthetic and functional problems; therefore, we assume that these factors may have some additional impact on one's quality of life.
A large number of self-report instruments have been used in orthodontics to evaluate the impact of malocclusion on OHRQoL. Of these, the short-form Oral Health Impact Profile (OHIP-14)
13 is the most frequently used to assess the impact of orthodontic problems
9 and the effect of treatment on OHRQoL.
14 Despite its popularity, differentiation among the various dimensions of the OHIP-14 can often be difficult because of the limited number of items used to characterize each domain.
15 Functional limitations, in particular, may be more comprehensively assessed using condition-specific instruments such as the short-form Jaw Functional Limitation Scale (JFLS-8),
16 which has been reported to be a useful self-report instrument for individuals with functional problems.
17
The objective of the present study was to investigate the differences in OHRQoL and jaw function between individuals with hyperdivergent and normodivergent facial types by using the OHIP-14 and JFLS-8, respectively. We hypothesized that individuals with hyperdivergent facial types would have relatively poorer OHRQoL, especially in the functional and psychosocial domains, than do individuals with normodivergent facial types.
MATERIALS AND METHODS
The study included orthodontic patients with hyperdivergent and normodivergent facial types (n = 80 in each group), individually matched according to age, sex, ethnicity, and orthodontic treatment stage. Study participants were recruited by systematically screening the lateral cephalograms of previous and existing patients treated in the orthodontic clinic at the University of Otago (Dunedin, New Zealand). Since this study was part of a broader research project, the sample size was estimated using an outcome measure (minor allele frequency for single-nucleotide polymorphisms) not reported in this article. The study was approved by the University of Otago Ethics Committee (reference, 11/196).
The inclusion criteria were a willingness to participate, provision of informed consent, and a good-quality pretreatment cephalogram. Patients were excluded from the study if they had more than four extracted permanent teeth (excluding third molars), orofacial clefts, craniofacial syndromes, or a history of facial fractures.
Classification of vertical facial morphology
Facial morphology was evaluated by screening pretreatment lateral cephalograms for the mandibular plane angle (sella-nasion to mandibular plane). Participants with hyperdivergent facial types (cases) were selected on the basis of having an SN-MP angle greater than 2 standard deviations from the norm, or 42°. Individuals with normodivergent facial types (controls) were selected if the mandibular plane angle was within 1 standard deviation of the norm, or between 27° and 37°. The cut-off values used to define the study groups were independent of age or sex, and were those commonly used in Caucasian populations.
18
Evaluation of OHRQoL
Study participants were asked to complete the 14-item OHIP-14 questionnaire based on their experiences over the previous 4 weeks.
13 The 14 items of the OHIP-14 represent the seven domains of function, pain, physical disability, psychological discomfort, psychological disability, social disability, and handicap. The participants reported the impact on each item by using a 5-point Likert-type response format (4 = very often, 3 = fairly often, 2 = occasionally, 1 = hardly ever, and 0 = never). An individual's overall score could range from 0 to 56, while the domain scores could range from 0 to 8. A higher OHIP-14 score indicated a greater impact on OHRQoL. The OHIP-14 scores were computed and reported as follows: (1) the prevalence or proportion of participants reporting more than one impact (defined as “very often” or “fairly often”, code 3 or 4); and (2) the severity or total OHIP-14 score (calculated by adding the scores of all 14 items).
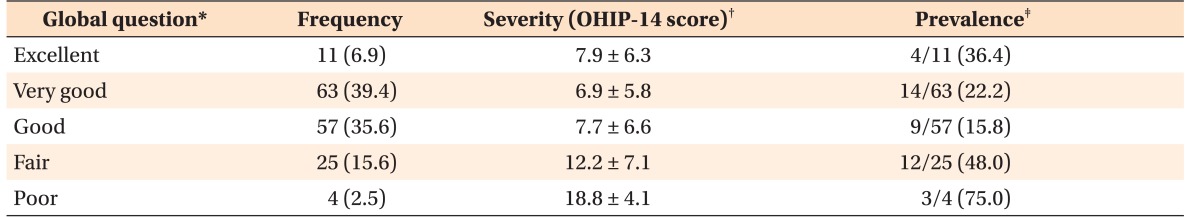
Concurrent validity of the OHIP-14 was investigated by observing the mean OHIP-14 scores across the ordinal response categories of a global question included in the study questionnaire (i.e., “How would you describe the health of your teeth or mouth?”).
19 Responses to the global question were recorded as either “excellent,” “very good,” “good,” “fair,” or “poor.”
Evaluation of jaw function
Study participants were also asked to complete the JFLS-8 based on their experiences over the previous 4 weeks.
16 The 8-item questionnaire sought information on the degree of limitation involved in carrying out normal daily tasks including chewing tough food, chewing chicken prepared in an oven, eating soft food not requiring chewing, opening the mouth wide enough to drink from a cup, swallowing, yawning, talking, and smiling. The participants reported the extent of functional limitation for each item by using an unmarked 10-cm visual analogue scale (VAS). They were asked to place a vertical mark on the scale that was anchored by “no limitation” at one end and “severe limitation” at the other end. They were also instructed not to respond to an item if they avoided that specific activity for reasons other than a physical limitation (such as a vegetarian who does not normally eat chicken—item 2). The VAS score for each item was recorded as a continuous variable.
Statistical analysis
Data were analyzed using conventional descriptive methods. Bivariate analysis was performed using the chi-square test, Fisher's exact test, and one-way analysis of variance as appropriate. Non-parametric tests (such as the Kruskal-Wallis and Mann-Whitney U tests) were used whenever a continuous dependent variable was not normally distributed. Data were analyzed using IBM SPSS Statistics for Macintosh (version 22.0; IBM Co., Armonk, NY, USA).
RESULTS
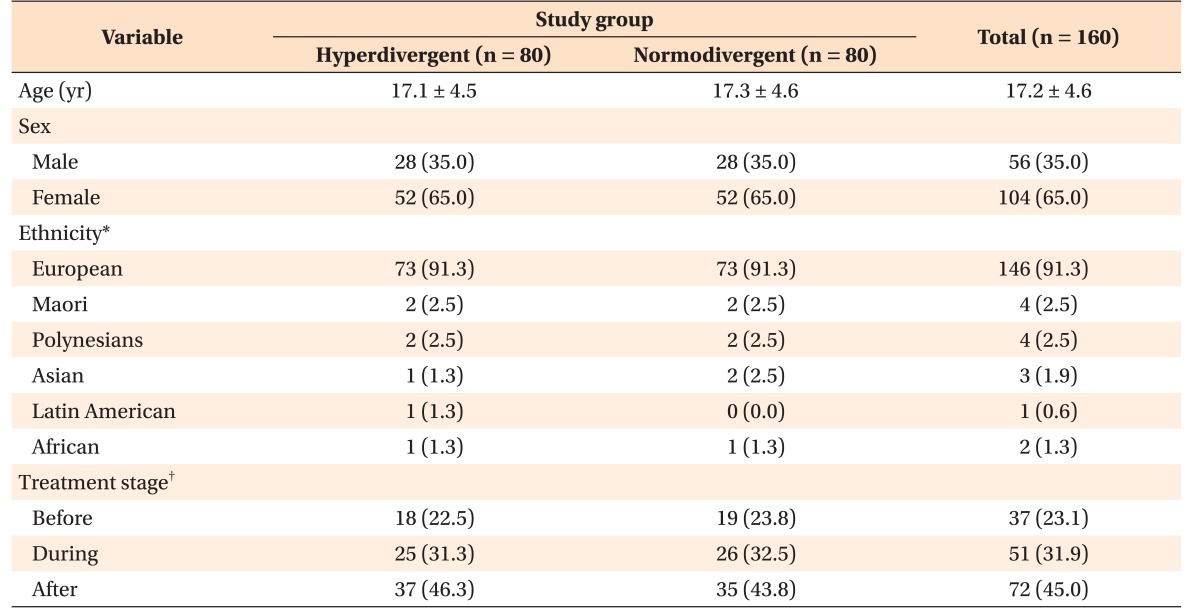
The mean age of the participants was 17.2 ± 4.6 years (range, 12–49 years), with most participants being female (65.0%) and of New Zealand European origin (91.3%;
Table 1). Approximately 25% of the participants had not received any orthodontic care, while 45% had completed treatment. The two groups differed primarily in hyperdivergence, but not in sagittal characteristics. For instance, the A point-nasion-B point angle in the cases (3.8° ± 2.7°) was similar to that in the controls (3.1° ± 3.1°;
p > 0.05).
The majority of the participants rated the overall health of their teeth and mouth as either “very good” (39.4%) or “good” (35.6%), with very few rating it as “poor” (2.5%). In general, a gradient was observed in the OHIP-14 scores across the five categories of the self-rated oral health global question (
Table 2). Participants who rated their overall oral health as either “fair” or “poor” had the highest mean OHIP-14 scores and greatest prevalence of OHIP-14 impacts.
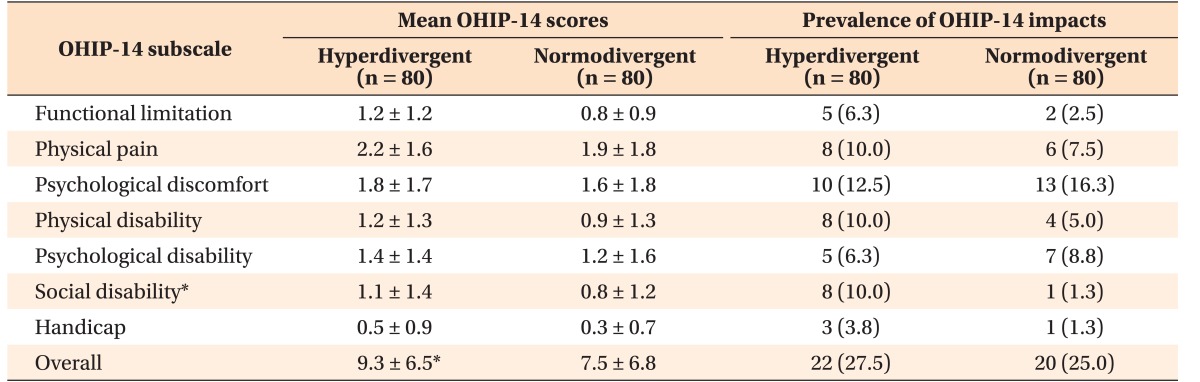
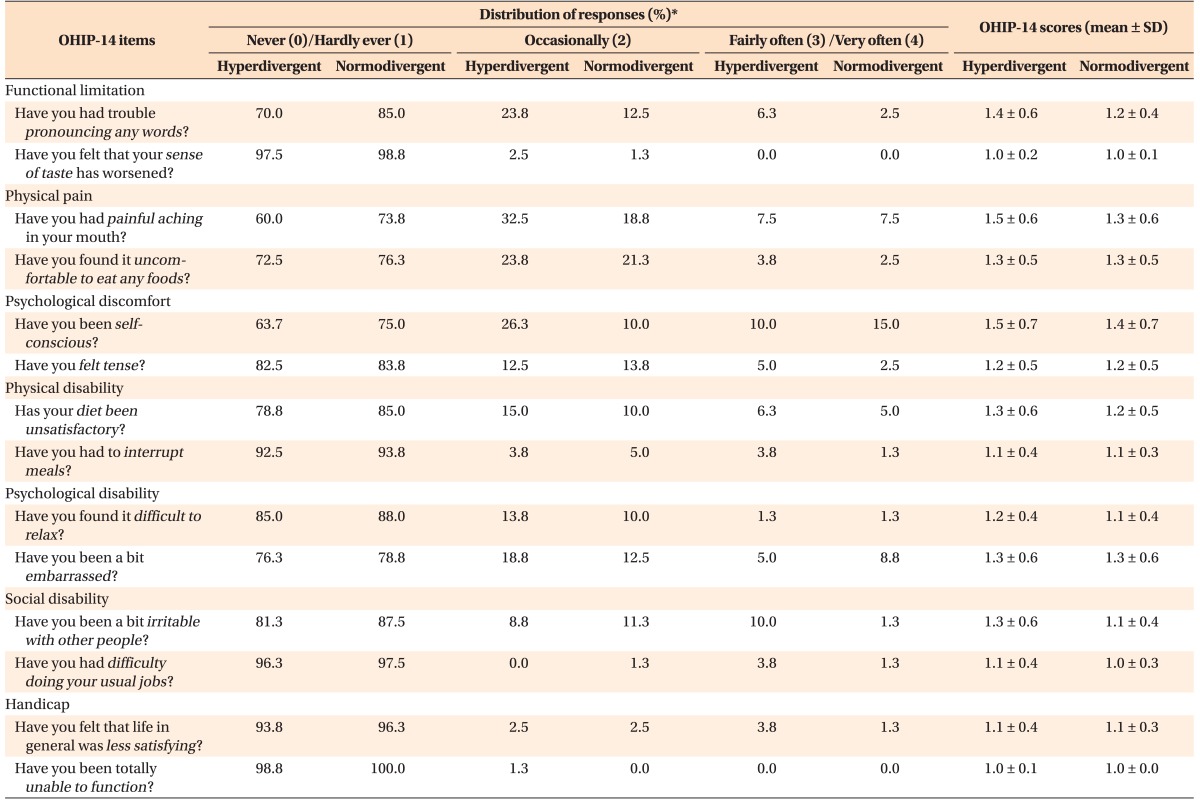
The prevalence of impacts and the mean score for each of the seven domains are presented in
Table 3. No statistically significant differences were observed in the prevalence of OHIP-14 impacts or in the mean item score for any of the 14 items between the two study groups (
Table 4). Approximately 10% of the participants with hyperdivergent facial types reported experiencing at least one impact related to social disability (
p < 0.05). These participants also had consistently higher mean OHIP-14 scores in all seven domains, even though these did not differ significantly from those of the controls. The overall OHIP-14 score was higher in the hyperdivergent group than in the normodivergent group (
p < 0.05).
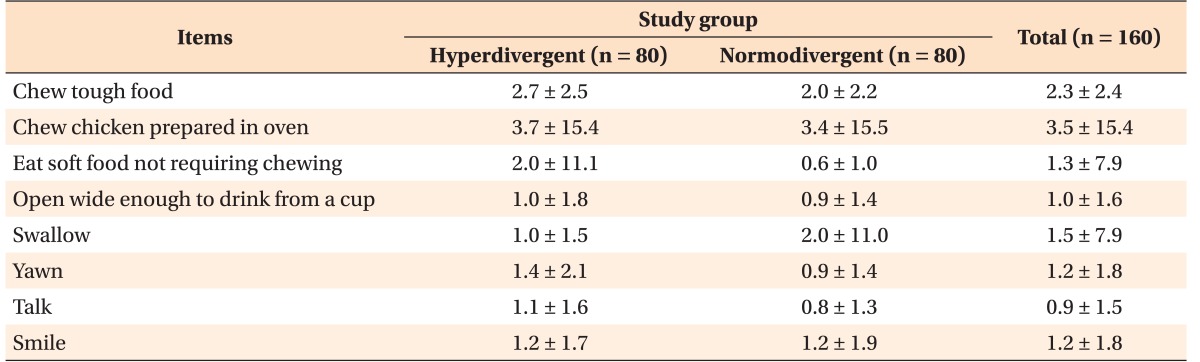
The participants with hyperdivergent facial types had a slightly higher mean score than did the controls for most of the JFLS-8 items, but these differences were not statistically significant (
Table 5). The greatest limitation in the hyperdivergent group was reported for “chewing chicken prepared in an oven” and “chewing tough food,” while the least discomfort occurred while “talking.” Moreover, the mean score for “eating soft food not requiring chewing” in the hyperdivergent group was identical to that for “chewing tough food” in the normodivergent group.
DISCUSSION
Few studies have investigated the impact of vertical facial form on OHRQoL. The purpose of this study was to investigate the impact of the hyperdivergent facial type on OHRQoL. Our findings suggest that some minor differences in OHRQoL exist between individuals with hyperdivergent and normodivergent facial types.
The study used two self-report instruments to assess the quality of life and functional limitations in individuals with different facial morphologies. Although the impact of malocclusions has traditionally been measured using clinical indices, there is a growing trend of combining these indices with OHRQoL measures in order to better evaluate a patient's self-perception of his/her facial appearance.
14 The OHIP-14 is a generic OHRQoL instrument with a number of important properties, including good discriminative abilities in normal orthodontic patient samples,
20 as well as in those with severe dentofacial deformities.
21 Moreover, it has been validated for use in young patients.
22 These features made the OHIP-14 ideal for evaluating OHRQoL in the present study sample with varied facial deformities and demographic characteristics.
The assessment of jaw function is somewhat more difficult because a large proportion of individuals are often not aware of their oral behaviors and habits.
23 Several instruments have been purposefully designed to evaluate jaw function, including the Research Diagnostic Criteria for Temporomandibular Disorders, the Functional Limitation Checklist,
24 and the Mandibular Function Impairment Questionnaire. These instruments were originally developed for assessing patients with temporomandibular disorders (TMDs), and they have not been validated for assessing other conditions.
16 Moreover, some have been found to have inadequate definitions of specific behaviors, along with overlapping content across domains.
16
The JFLS is another condition-specific instrument that has recently been developed for patients with TMDs.
16 Unlike previous scales, however, the JFLS has been validated for a range of oral conditions, including primary Sjogren syndrome, burning mouth syndrome, skeletal malocclusion, and healthy dentitions.
1725 More specifically, the JFLS has been validated for severe malocclusions such as anterior open bite and mandibular prognathism.
25 Although the JFLS-20 was originally validated for assessing three distinct constructs (mastication, vertical jaw mobility, and emotional and verbal expression), the short-form version (JFLS-8) has also been shown to be a useful measure of global functional limitation of the jaws.
25 The combined use of a generic OHRQoL measure and a condition-specific functional scale was useful in this study because some of the participants were expected to have both psychological and functional problems.
Individuals with hyperdivergent facial patterns did not differ from the controls in either the functional limitation subscale of the OHIP-14 or any of the JFLS-8 items. Interestingly, the mean score for “eating soft food not requiring chewing” in the hyperdivergent group was identical to that for “chewing tough food” in the control group. A similar preference for soft and pasty food (over solid food) has also been reported in young children with enlarged adenotonsillar tissue and who often present with similar skeletal patterns.
26 These findings indicate that participants with hyperdivergent facial types may experience minor problems with mastication and deglutition, probably owing to the biomechanical properties of their masticatory system. Indeed, individuals with hyperdivergent facial types are reported to have poor masticatory muscle efficiency, which results in a slower rate of chewing during eating, than do individuals with normodivergent facial types.
12
The lack of incisor contact due to an anterior open bite has also been associated with discomfort while eating.
9 Although anterior open bite occurs in a large proportion of patients with hyperdivergent facial types,
27 neither our sample size nor the study design allowed us to investigate the impact of anterior occlusion on jaw function. Future studies, however, should focus on investigating jaw function in different subphenotypes of the hyperdivergent facial type, especially those without incisor contact.
Study participants with hyperdivergent facial types in this study had greater mean scores and prevalence of OHIP-14 impacts for the overall scale and social disability subscale than did the ones with normodivergent facial types. Previous studies using orthodontic samples have also found greater impacts in the emotional and social domains of the CPQ
11-14.
34 The impact of malocclusions on social interactions and interpersonal relationships is likely to reflect a desire for better esthetics. Individuals with particularly long faces are known to present with a wide range of dental and facial esthetic concerns, including gummy smile, greater lower facial height, and anterior open bite.
8 Although orthodontic treatment may help address some of these esthetic concerns, it is unlikely that other issues (particularly skeletal ones) would be corrected without surgical intervention.
With the exception of the social domain, we found no statistically significant differences in the other six domains of the OHIP-14 between the two study groups. In fact, the prevalence of impacts for the two psychological domains was somewhat higher in the normodivergent group than in the hyperdivergent group. This was somewhat unexpected, because patients with hyperdivergent facial types are reported to have less attractive profiles than do those with normodivergent facial types,
1011 and this could have some adverse impact on the former group's social development and functioning.
28 Of course, the exact definition of facial attractiveness is not universal, with opinions differing substantially between clinicians and lay people.
29 Nonetheless, the mediating role of facial attractiveness should still be considered in future studies designed to investigate the impact of dentofacial anomalies on OHRQoL.
Several other reasons may account for the lack of differences between the two study groups. For instance, the selection criterion (i.e., mandibular plane angle) used to classify facial type may not reflect the important esthetic or functional differences between the groups. Lower anterior facial height has been reported to be an important predictor of facial attractiveness—even more so than sagittal features.
10 Profiles with greater lower anterior facial height have been rated as the least attractive and the most in need of orthodontic treatment.
11 The participants in this study differed primarily on the basis of skeletal divergence and not necessarily on the basis of their lower anterior facial height. Future studies should, therefore, consider the use of additional cephalometric measurements to characterize the hyperdivergent facial phenotype.
Another important confounding factor is the impact of other malocclusion features on an individual's OHRQoL. Although this study investigated only the impact of vertical morphology, it is important to note that other occlusal features (such as lateral cross bite and anterior spacing) may adversely affect an individual's quality of life.
79 Indeed, the effect of orthodontic treatment on OHRQoL has been shown to differ among patients with different malocclusions.
30 It is noteworthy, however, that previous studies have also encountered similar difficulties while investigating the relationship between specific features of a malocclusion (e.g., vertical dysplasia) and OHRQoL.
9
This study had a number of limitations, which may have masked important differences in OHRQoL and jaw function between the groups. First, the study may not have been adequately powered to detect particularly small effect sizes. Second, most of the study participants were either undergoing orthodontic treatment or had completed treatment at the time of participation. Patients undergoing orthodontic treatment often experience a significant worsening of OHRQoL,
19 and this may have confounded the relationship between malocclusion and quality of life in our study. In other words, the impact of treatment status on OHRQoL may have been greater than that of the underlying malocclusion. Although treatment duration may have some impact on OHRQoL, we could not evaluate this because of the mixed design and cross-sectional nature of the study (i.e., some participants had still not started or finished treatment at the time of the study). Third, the study did not utilize clinical or epidemiological indices (such as the Dental Aesthetic Index
31) to adjust for differences in malocclusion severity between the study groups. Other clinical factors such as periodontal health and level of dental decay were also not considered in this study; however, most of the participants were generally young adolescents who were expected to have good oral health. Finally, detailed screening for TMDs was not carried out; however, the prevalence of these conditions was expected to be low given the young age of the participants. Future studies should address limitations of the current study design.
Despite these limitations, the study had a number of strengths including the use of a global question to validate the OHIP-14.
19 We found that participants who reported their overall oral health as “poor” or “fair” did in fact have the highest OHIP-14 score (or worse OHRQoL). Accordingly, the OHIP-14 was considered a valid measure of how participants in this study viewed their general oral health. In addition, the effects of some potential confounders were reduced by individually matching the groups according to age, sex, ethnicity, and treatment stage. From a clinical perspective, these findings may be useful for understanding the impact of facial divergence and treatment on a patient's everyday life. Future work should focus on determining the minimally important difference in the OHIP-14 score required for triggering a clinically important change in oral health.
32




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download