1. Franchi L, Baccetti T. Transverse maxillary deficiency in Class II and Class III malocclusions: a cephalometric and morphometric study on postero-anterior films. Orthod Craniofac Res. 2005; 8:21–28. PMID:
15667642.

2. Proffit WR, Phillips C, Prewitt JW, Turvey TA. Stability after surgical-orthodontic correction of skeletal Class III malocclusion. 2. Maxillary advancement. Int J Adult Orthodon Orthognath Surg. 1991; 6:71–80. PMID:
1811032.
3. McNamara JA. Maxillary transverse deficiency. Am J Orthod Dentofacial Orthop. 2000; 117:567–570. PMID:
10799117.
4. Uysal T, Usumez S, Memili B, Sari Z. Dental and alveolar arch widths in normal occlusion and Class III malocclusion. Angle Orthod. 2005; 75:809–813. PMID:
16279827.
5. Ricketts RM. Perspectives in the clinical application of cephalometrics. The first fifty years. Angle Orthod. 1981; 51:115–150. PMID:
6942666.
6. Hesby RM, Marshall SD, Dawson DV, Southard KA, Casko JS, Franciscus RG, et al. Transverse skeletal and dentoalveolar changes during growth. Am J Orthod Dentofacial Orthop. 2006; 130:721–731. PMID:
17169734.

7. Leonardi R, Annunziata A, Caltabiano M. Landmark identification error in posteroanterior cephalometric radiography. A systematic review. Angle Orthod. 2008; 78:761–765. PMID:
18302479.
8. Jung PK, Lee GC, Moon CH. Comparison of cone-beam computed tomography cephalometric measurements using a midsagittal projection and conventional two-dimensional cephalometric measurements. Korean J Orthod. 2015; 45:282–288. PMID:
26629474.

9. Kusayama M, Motohashi N, Kuroda T. Relationship between transverse dental anomalies and skeletal asymmetry. Am J Orthod Dentofacial Orthop. 2003; 123:329–337. PMID:
12637905.

10. Tyan S, Park HS, Janchivdorj M, Han SH, Kim SJ, Ahn HW. Three-dimensional analysis of molar compensation in patients with facial asymmetry and mandibular prognathism. Angle Orthod. 2016; 86:421–430. PMID:
26192894.

11. Burstone CR. Deep overbite correction by intrusion. Am J Orthod. 1977; 72:1–22. PMID:
267433.

12. Melsen B, Agerbaek N, Markenstam G. Intrusion of incisors in adult patients with marginal bone loss. Am J Orthod Dentofacial Orthop. 1989; 96:232–241. PMID:
2773869.

13. Smith RJ, Burstone CJ. Mechanics of tooth movement. Am J Orthod. 1984; 85:294–307. PMID:
6585147.

14. Jo AR, Mo SS, Lee KJ, Sung SJ, Chun YS. Finite-element analysis of the center of resistance of the mandibular dentition. Korean J Orthod. 2017; 47:21–30. PMID:
28127536.

15. van Steenbergen E, Burstone CJ, Prahl-Andersen B, Aartman IH. Influence of buccal segment size on prevention of side effects from incisor intrusion. Am J Orthod Dentofacial Orthop. 2006; 129:658–665. PMID:
16679206.

16. Lee KJ, Joo E, Kim KD, Lee JS, Park YC, Yu HS. Computed tomographic analysis of tooth-bearing alveolar bone for orthodontic miniscrew placement. Am J Orthod Dentofacial Orthop. 2009; 135:486–494. PMID:
19361735.

17. Vanarsdall RL Jr. Transverse dimension and long-term stability. Semin Orthod. 1999; 5:171–180. PMID:
10860069.

18. Burstone CJ, Choy K. The biomechanical foundation of clinical orthodontics. Chicago: Quintessence Publishing Co, Inc.;2015.
19. Lim MY, Lim SH. Comparison of model analysis measurements among plaster model, laser scan digital model, and cone beam CT image. Korean J Orthod. 2009; 39:6–17.

20. Barrett JF, Keat N. Artifacts in CT: recognition and avoidance. Radiographics. 2004; 24:1679–1691. PMID:
15537976.

21. Kuntz TR, Staley RN, Bigelow HF, Kremenak CR, Kohout FJ, Jakobsen JR. Arch widths in adults with Class I crowded and Class III malocclusions compared with normal occlusions. Angle Orthod. 2008; 78:597–603. PMID:
18302456.

22. Lee HK, Son WS. A study on basal and dental arch width in skeletal class III malocclusion. Korean J Orthod. 2002; 32:117–127.
23. Masumoto T, Hayashi I, Kawamura A, Tanaka K, Kasai K. Relationships among facial type, buccolingual molar inclination, and cortical bone thickness of the mandible. Eur J Orthod. 2001; 23:15–23. PMID:
11296507.

24. Suk KE, Park JH, Bayome M, Nam YO, Sameshima GT, Kook YA. Comparison between dental and basal arch forms in normal occlusion and Class III malocclusions utilizing cone-beam computed tomography. Korean J Orthod. 2013; 43:15–22. PMID:
23504406.

25. Robert WE. Bone physiology, metabolism, biomechanics in orthodontic practice. In : Graber LE, Vanarsdall RL, Vig KW, editors. Orthodontics: current principles and techniques. 5th ed. Philadelphia, PA: Elsevier/Mosby;2012.
26. Proffit WR. Equilibrium theory revisited: factors influencing position of the teeth. Angle Orthod. 1978; 48:175–186. PMID:
280125.
27. Ovsenik M, Primožič J. How to push the limits in the transverse dimension? Facial asymmetry, palatal volume and tongue posture in children with unilateral posterior cross bite: a three-dimensional evaluation of early treatment. Orthod Fr. 2014; 85:139–149. PMID:
24923214.
28. Braun S, Hnat WP, Fender DE, Legan HL. The form of the human dental arch. Angle Orthod. 1998; 68:29–36. PMID:
9503132.
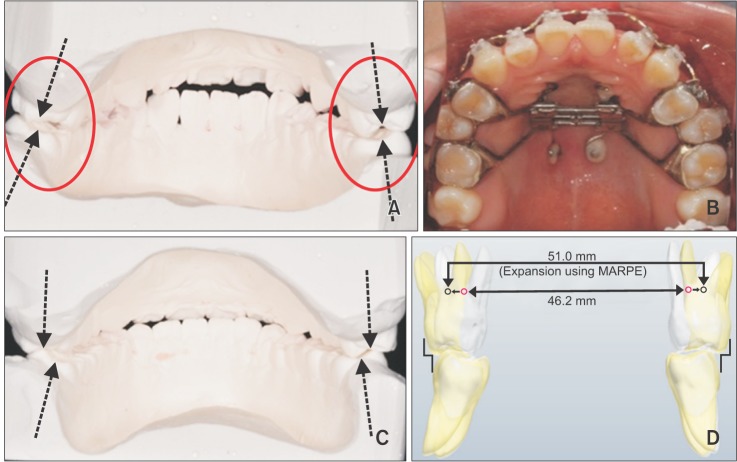
29. Choi SH, Shi KK, Cha JY, Park YC, Lee KJ. Nonsurgical miniscrew-assisted rapid maxillary expansion results in acceptable stability in young adults. Angle Orthod. 2016; 86:713–720. PMID:
26938955.

30. Lee KJ, Park YC, Park JY, Hwang WS. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop. 2010; 137:830–839. PMID:
20685540.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download