INTRODUCTION
In skeletal Class III patients with maxillary hypoplasia, facemasks have been widely used to stimulate the protraction of the maxilla during the growth period. Several intraoral tooth-borne devices have been used to transfer orthopedic force from the facemask to the maxilla.
123
However, since these appliances use the maxillary dentition for orthopedic anchorage, they cause some side effects beside maxillary protraction. Proclination of the upper incisors, mesialization and extrusion of the maxillary molars, camouflage of the skeletal effect, constriction of the maxillary arch and space closure of the canines, and posterior rotation of the mandible due to molar extrusion are the most commonly observed side effects of tooth-borne anchorage.
345
In order to avoid the side effects of tooth-borne appliances and to transfer the orthopedic force directly to the maxilla, intentionally ankylosed deciduous canines,
6 osseointegrated implants,
7 mini-implants,
8 onplants,
9 and miniplates
1011121314151617 have been used as skeletal anchorage units during protraction. However, ankylosed teeth could be loosened because of root resorption,
6 and implants and onplants would need osseointegration before force application.
79 Miniplates have been successfully used in maxillary protraction therapy as skeletal anchorage because they offer the following advantages: the force can be applied immediately after insertion, they can be properly contoured to match anatomical structures, and they are resistant to orthopedic forces.
10111213141516
In the literature, few clinical studies have evaluated miniplate-anchored facemask therapy.
1314151618 In those studies, miniplates were inserted to different anatomical locations, and only two of them preferred the zygomatic buttresses of the maxilla.
1516 However, neither of these studies compared their results with those of Class III control subjects. Therefore, the aim of this study was to evaluate the dentofacial effects of therapy using a facemask, which was anchored from the zygomatic buttresses of the maxilla by using two miniplates, in skeletal Class III patients with maxillary deficiency and to compare their results with those of a Class III control group.
MATERIALS AND METHODS
The study analyzed the lateral cephalograms of patients with skeletal Class III malocclusions who were referred to the Department of Orthodontics, Faculty of Dentistry, Gazi University for their orthodontic treatment. Ethical approval was obtained from the Ethical Committee of Faculty of Dentistry, Ankara University (09.01.2012-28/4).
The patients who fulfilled the following inclusion criteria were included in the study: (1) skeletal (ANB < 0°, Wits < −2 mm) and dental Class III malocclusion with maxillary retrusion (SNA < 82°), or maxillary retrusion and mandibular protrusion (SNB > 80°); (2) decreased or optimum mandibular plane angle (SN/GoGn ≤ 38°); (3) absence of functional shift of the mandible; (4) between developmental growth stages PP2= (i.e., the epiphysis of the proximal phalanx of the index finger has the same width as the diaphysis; this stage indicates the prepubertal growth period) and MP3cap (i.e., the diaphysis of the middle phalanx of the middle finger is covered by the cap-shaped epiphysis; this stage indicates the peak of the pubertal growth spurt), as evaluated using hand-wrist radiographs; and (5) no craniofacial anomalies or previous orthodontic treatment.
The study consisted of two groups: the treatment group (18 patients; 10 girls and 8 boys; mean pre-treatment age, 11.4 ± 1.28 years) that received miniplate-anchored facemasks, and an untreated control group (18 patients; 9 girls and 9 boys; mean pre-treatment age, 10.6 ± 1.12 years) that was formed from the archives of the department to distinguish the changes caused by the treatment and growth. The material comprised the records of patients with Class III malocclusions whose treatment could not be started because of poor hygiene and/or changes in dentition.
Surgical protocol
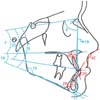
In the treatment group, two titanium miniplates were inserted at the zygomatic buttresses of the maxilla by the same maxillofacial surgeon. The I-shaped miniplates were designed with two holes in the body and a C hook at the head. The neck of the miniplate was a rounded bar 20 mm in length and 1.5 mm in diameter (Tasarımmed, Istanbul, Turkey) (
Figure 1). At the buccal vestibule side, a mucoperiosteal flap was elevated between the maxillary canine and the distal border of the first molar under local anesthesia to expose the maxillary zygomatic buttress. The miniplates were shaped to match the anatomic structure of the zygomatic buttresses and fixed using two self-drilling miniscrews 2 mm in diameter and 5 mm in length (Tasarımmed). The flap was closed and the C-shaped heads of the miniplates were exposed at the level of the soft tissue between the maxillary canine and first premolar (
Figure 2).
Maxillary protraction protocol
One week after the placement of the miniplates, protraction forces were applied from the miniplates to the Petit-type facemask. Elastics were directed 30° downward from the occlusal plane and exerted a 400
g force per side (
Figure 3). A removable, acrylic bite raiser covering the mandibular dentition was used to avoid occlusal contacts. Patients wore the facemask all day except during meals.
The bite raiser was used until edge-to-edge incisor relation was achieved, and the facemasks were used until at least 2-mm overjet was achieved. The miniplates were not removed considering the different anchorage needs during the fixed orthodontic treatment.
Lateral cephalograms were acquired before miniplate insertion (T0) and after facemask therapy (T1) in the treatment group, and before (T0) and after (T1) the observation period in the control group. All cephalograms were traced and superimposed by the same operator. The tuberculum sella-wing (T-W) plane was constructed as the “horizontal reference plane (x)” to evaluate vertical changes. The “vertical reference plane (y)” was constructed perpendicular to the T-W plane at the T point to evaluate sagittal changes (
Figures 4 and
5). The lateral cephalograms acquired at T1 were superimposed on those acquired at T0 along the T-W plane at the T point, and the reference planes were transferred from the cephalograms acquired at T0 to those acquired at T1.
Maxillary and mandibular local superimpositions were performed to evaluate the dentoalveolar changes caused by treatment/observation. The “maxillary horizontal reference plane (x1)” was drawn along the ANS-PNS plane, and the “maxillary vertical reference plane (y1)” was drawn perpendicular to the ANS-PNS plane at the PNS point. The “mandibular horizontal reference plane (x2)” was drawn along the Go-Gn plane, and the “mandibular vertical reference plane (y2)” was drawn perpendicular to the Go-Gn plane at the Go point (
Figure 6). On each lateral cephalogram, 14 angular and 28 linear measurements were made (
Figures 4,
5,
6).
Statistical analysis
The power of the sample sizes of the groups was analyzed using G*Power Software (v3.1.3; Franz Faul, Universität Kiel, Germany). The data obtained from the subjects were evaluated using IBM SPSS Statistics for Windows, version 20.0 (IBM Corp., Armonk, NY, USA). The normality of the distribution of the variables was examined using the Shapiro-Wilk test. As the variables did not show a normal distribution, the Mann-Whitney U-test was used for intergroup comparisons and the Wilcoxon test was used for intragroup comparisons. p < 0.05, p < 0.01, and p < 0.001 were considered statistically significant.
RESULTS
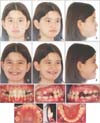
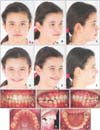
During protraction therapy, screw loosening was observed once in 3 miniplates and twice in 1 miniplate out of the 36 miniplates, and the success rate of miniplate stability was 86.11%. After mobility was observed, the miniplates were immediately replaced onto a substantial bone as close as possible to the previous insertion area of the zygomatic buttresses, and the patients continued wearing the facemasks. Pre- and posttreatment images of one of the patients in treatment group were given in
Figure 7 and
8, respectively.
In this study, the power of the sample size of both groups was found to be 95%. A comparison of the initial ages and dentofacial morphology of both groups is shown in
Table 1. The mean chronological age of the treatment group was statistically higher than that of the control group (
p < 0.01). ANB°, U1/NA°, and U1/ANSPNS°, as well as the ANS-PNS, Co-Gn, U1-NA, U1-y1, and U6-y1 dimensions showed statistically significant differences between the two groups at T0 (
Table 1).
The mean treatment period in the treatment group was 1.08 ± 0.35 years, and the mean observation period in the control group was 0.82 ± 0.28 years. The treatment time was statistically higher than the observation time (
p < 0.05).
Table 2 presents the changes during the treatment and observation periods, as well as the differences between the two groups. The cranial changes (S-N) in both groups were statistically significant (
p < 0.001); however, these changes were similar between the groups. The 2.2° increase in SNA° in the treatment group was statistically significant compared to that in the control group (
p < 0.001). In the treatment group, a significant forward movement of the maxilla was observed, i.e., 3.97 mm and 3.31 mm in Co-A and A-y, respectively (
p < 0.001). In the control group, the change in Co-A was statistically significant with a movement of 1.82 mm (
p < 0.001), while that in A-y was insignificant. The anterior replacement of the maxilla was significantly greater in the treatment group than in the control group. The significant (
p < 0.001) vertical movement of the A point (A-x) and the increase in maxillary length (ANS-PNS) were statistically greater in the treatment group than in the control group (
p < 0.05). The anterior rotation of the maxilla in the treatment group and the posterior rotation of the maxilla in the control group were insignificant in both intragroup and intergroup analyses.
The mandible showed both downward and backward movement with treatment. The 1.33° decrease of SNB° in the treatment group was significantly greater than the 0.08° decrease of SNB° in the control group (p < 0.01). Sagittal changes of the B point (B-y) were statistically different between the two groups (p < 0.05). This value decreased in the treatment group and increased in the control group insignificantly. The vertical position of the B point (B-x) increased significantly in both groups (p < 0.001), and the changes were significantly greater in the treatment group than in the control group (p < 0.05). The significant increase in total mandibular length (Co-Gn), corpus length (Go-Me), and ramus length (Ar-Go) was similar between the groups. The posterior rotation of the mandible was statistically significant in the treatment group (p < 0.01), whereas the mandible showed insignificant anterior rotation in the control group; both these changes were statistically different (p < 0.01).
The increase in ANB° and the improvement in Wits appraisal were higher in the treatment group than in the control group (p < 0.001). The maxillomandibular plane angle (ANSPNS/GoGn°) also increased significantly in the treatment group than in the control group (p < 0.01), and the results were significantly different between the groups (ANB° and Wits, p < 0.001; ANSPNS/GoGn°, p < 0.01).
The upper anterior face height (N-ANS), lower anterior face height (ANS-Me), and posterior face height (S-Go) increased significantly in both groups. However, only the increase in the lower anterior face height was significantly different between the groups (p < 0.001).
The changes in the upper incisor angles (U1/NA° and U1/ANSPNS°), upper incisor vertical position (U1-x1), and upper incisor to NA dimension (U1-NA) were insignificant in both groups. On the local superimpositions, the sagittal position of the upper incisors increased significantly in both groups (p < 0.05); however, this increase was similar and insignificant in both groups. The sagittal positions of the upper first molars remained stable in both groups; however, the vertical positions of these teeth increased significantly. The increase in the treatment group was significantly greater than that in the control group (p < 0.05). The lower incisors retruded (L1/NB, L1/GoMe, and L1-y2) more significantly in the treatment group than in the control group (L1/NB and L1-y2, p < 0.001; L1/GoMe, p < 0.01). The increase in overjet and the decrease in overbite in the treatment group were significantly greater than those in the control group (overjet, p < 0.001; overbite, p < 0.01). Moreover, the upper lip protruded and the lower lip retruded more significantly in the treatment group than in the control group (UL-S line, p < 0.001; LL-S line, p < 0.01).
DISCUSSION
The treatment of skeletal Class III malocclusions with facemasks is the most preferred method in the prepubertal/pubertal growth period.
19 However, several facemask studies using tooth-borne anchorage devices have reported undesired side effects.
45 Recently, skeletal anchorage systems, which transfer the orthopedic force directly to the bone, have become popular because they help overcome the side effects of tooth-borne devices and achieve more desirable orthopedic effects. To this end, clinicians have started using miniplates, which are biocompatible devices that allow immediate force application without having to wait after insertion.
111820
Clinicians have reported different maxillary protraction mechanics with miniplate anchorage. Some authors have used only intraoral protraction mechanics. For example, De Clerck et al.
10 reported the use of intraoral Class III elastics between the maxillary and mandibular miniplates, while Sar et al.
13 and Coscia et al.
21 used intraoral elastics between a bonded tooth-borne appliance and the miniplates. In contrast, a group of authors preferred protraction of the maxilla with a facemask together with miniplate anchorage.
1112131415161718 However, none of these studies used a control group to eliminate the possible effects of growth. In the present study, maxillary protraction was performed using a facemask, which was anchored to two miniplates from the zygomatic buttresses of the maxilla, and the results were compared with those of a Class III control group.
Many of the previous miniplate-anchored facemask studies emphasized the use of the apertura piriformis as the miniplate insertion area.
11131418 However, only two clinical controlled trials have reported the insertion of miniplates to the zygomatic buttresses of the maxilla.
1516 The zygomatic buttress of the maxilla is close to the center of resistance of the nasomaxillary complex
22 and has enough bone thickness for miniplate insertion.
2324 The miniplates in this area have sufficient distance to the roots of the posterior teeth,
24 and therefore, they can be useful for further orthodontic treatments.
25
The tuberculum sella (T) and wing (W) points have been reported to maintain their stability in the pubertal developmental phases,
26 as the middle cranial base completed its growth in the earlier period.
27 Therefore, the T-W plane was used as a reliable reference plane in the present study.
Statistically significant differences were observed between the chronological ages of the two groups, whereas the differences between the groups in terms of skeletal ages were statistically insignificant. Previous studies have shown that skeletal age is more reliable than chronological age in determining the growth period; therefore, in this study, the patients in the two groups were matched according to their skeletal ages.
2829
The mean treatment period was 1.08 ± 0.35 years and the mean observation period was 0.82 ± 0.28 years. Skeletal Class III malocclusions should be treated at an early stage, and as early as possible in the growth period; therefore, in the present study, the duration of observation was statistically shorter than the duration of treatment (p < 0.05).
In the present study, the increase in SNA° was 2.2° and the forward movement of the A point was 3.31 mm with maxillary protraction. In the previous facemask studies utilizing miniplates, the increase in SNAo was reported to range between 1.7° and 3.7°, and the forward movement of the A point was reported to range between 2 mm and 4.8 mm.
1314151618
In the literature, a significant anterior rotation has been reported in the maxilla because of the force vector of the facemask passing below the center of resistance of the maxilla when using tooth-borne devices.
230 One of the main goals of the present study was the protraction of the maxilla without any rotation along the palatal plane by inserting the miniplates as close as possible to the center of resistance. The 0.31° anterior rotation of the palatal plane in the treatment group was insignificant compared to the 0.28° posterior rotation of the control group. Therefore, we can safely conclude that a miniplate-anchored facemask decreased, but not eliminated, the rotation of the palatal plane. Sar et al.
13 and Lee et al.
15 reported results in line with the present study findings, whereas Cha and Ngan
16 and Kaya et al.
14 found significant anterior rotation in the maxilla, which was different from our findings.
In the present study, the mandible showed downward and backward rotation with a significant decrease in the SNB° and B-y dimension, and a significant increase in the SN/GoGn° and B-x dimension. The significant increase in the vertical condyle position (Co-x) and lower face height (ANS-Me) in the treatment group supported the vertical changes in the mandible resulting from the treatment. Previous facemask studies have reported posterior rotation of the mandible due to the extrusion of the upper molars with tooth-borne devices, anterior rotation of the palatal plane, and the force directed with the facemask posteriorly to the chin.
2530 Previous studies that evaluated the effects of miniplate-anchored facemask therapy on the mandible have shown results similar to the results of the present study.
13141516
The maxillomandibular relationship showed significant improvements with increases of 3.81° and 5.44 mm in ANB° and Wits appraisal, respectively, in the treatment group. A significant increase in ANB° has been previously reported by Lee et al.
15 (3.81°), Cha and Ngan
16 (4.36°), Sar et al.
13 (4.46°), and Kaya et al.
14 (2.8°). Moreover, a significant increase in the Wits appraisal has been reported by Sar et al.
13 (5.43 mm) and Kaya et al.
14 (4.2 mm). Because of the insignificant decrease along the palatal plane and the significant increase along the mandibular plane angles, the maxillomandibular plane angle (ANSPNS/GoGn°) showed a significant increase in the treatment group.
One of the main advantages of skeletally anchored maxillary protraction is that it helps achieve maximum skeletal effect and minimum dental side effects while eliminating the proclination of the upper incisors and mesialization of the maxillary molars, which have been reported in most of the studies using conventional methods.
15 In this study, the proclination of the upper incisors and the mesialization of the maxillary molars were controlled successfully by using miniplate anchorage. In their studies comparing miniplate-anchored facemasks with tooth-borne anchored facemasks, Cha and Ngan
16 and Sar et al.
13 found insignificant changes in the upper incisors with miniplates while they significantly protruded the teeth with RME anchorage. In the same study, Cha and Ngan
16 reported insignificant maxillary molar changes with miniplate anchorage and significant mesialization with RME anchorage. In contrast, Lee et al.
15 reported significant upper incisor protrusion with miniplate and RME anchorage; however, protrusion was greater in the RME group than in the miniplate group.
In facemask therapy, the pressure on the lower incisors causes lower incisor retroclination, as previously reported in several studies.
51314 In our study, the lower incisors showed similar results.
In the present study, overjet increased significantly (5.72 mm) with the treatment. While 57.9% of this improvement was due to maxillary protraction, 19.2% was due to mandibular posterior rotation and 22.7% due to lower incisor retroclination. Miniplate-anchored facemask studies have reported that a great amount of overjet improved after maxillary anterior replacement.
131415
The overbite decreased significantly after maxillary protraction and this change was more statistically significant in the treatment group than in the control group (
p < 0.01). The decrease in overbite could be due to insignificant anterior rotation of the palatal plane and significant posterior rotation of the mandibular plane. Contrary to this result, previous miniplate-anchored facemask studies have reported insignificant changes in overbite.
131415
The soft-tissue profile improved with significant protrusion of the upper lip (
p < 0.001) and significant retrusion of the lower lip (
p < 0.01) after maxillary protraction treatment. The upper lip protrusion was caused by maxillary forward replacement and the lower lip retrusion was caused by the retroclination of the lower incisors. Lee et al.
15 reported greater upper lip protrusion with tooth-borne anchorage than with miniplate anchorage; however, the lower lip showed insignificant changes in the same study. Cha and Ngan
16 and Kaya et al.
14 also reported insignificant lower lip changes, while Sar et al.
13 reported retrusion in the lower lips, which agrees with the findings of the present study. While comparing our results with those of similar studies in the literature, the differences in patient selection and study design should be taken into account. The mean age of our study group was similar to that of other miniplate-anchored facemask studies,
141618 implying that age may not be the reason for the differences observed in the results. When the treatment protocol is considered, the position (i.e., the zygomatic buttresses of the maxilla) and differences in the design of the miniplates, as well as the total duration of applied force (all day except meal times) could also possibly have altered the outcomes.
This study also has some limitations. The insertion and removal of miniplates are invasive surgical procedures, and these caused some discomfort to our patients. In addition, the use of a facemask needs patient cooperation, and might cause undesired effects in the mandible (posterior rotation) and lower incisors (retroclination), which all limit the advantages of using miniplates in Class III malocclusion therapy.
Nevertheless, the use of miniplates in combination with a facemask could be an alternative treatment when more skeletal effects are desired and tooth-borne anchorage is not possible. Although our study provides promising results, further studies are needed to evaluate the long-term stability and success of this treatment.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download