Abstract
Objective
The purpose of the present study was to evaluate the postoperative three-dimensional (3D) changes in the proximal segments after mandibular setback sagittal split ramus osteotomy and to compare the changes between the conventional mini-plate fixation and semi-rigid sliding plate fixation.
Methods
Cone-beam computed tomography (CBCT) images were used to evaluate the postoperative 3D changes in the proximal segments during the healing process. CBCT images were superimposed using the symphysis and the lower anterior mandible as references.
Results
There were no statistically significant differences between the conventional mini-plate and semi-rigid sliding plate groups (p > 0.05). With respect to the distribution of changes greater than 2 mm in the landmarks, the right condylion, right coronoid process, and left condylion showed ratios of 55.6%, 50.0%, and 44.4%, respectively, in the semi-rigid sliding plate group; however, none of the landmarks showed ratios greater than 30% in the conventional mini-plate group.
Conclusions
There were no statistically significant differences in postoperative changes in the segments between the conventional mini-plate and semi-rigid sliding plate groups. Nevertheless, while selecting the type of fixation technique, clinicians should consider that landmarks with greater than 2 mm changes were higher in the semi-rigid sliding plate group than in the conventional mini-plate group.
Postoperative skeletal relapse after mandibular setback surgery has already been reported by many investigators.1234567 In their study on various factors inducing postoperative skeletal relapse, Proffit et al.8 reported significant correlations between postoperative changes in the positions of the chin and gonion. In another study, Joss and Vassalli9 insisted that controlling the proximal segment is an important technique for achieving skeletal stability. Yet another study showed that the postoperative condylar position is affected by various factors such as the surgeon’s skill, surgical procedure, and neuromuscular environment.1011
Bilateral sagittal split ramus osteotomy (BSSRO) is a common surgical procedure for correcting jaw deformations. The use of rigid fixation in such procedures offers several advantages to patients undergoing orthognathic surgery, including minimal maxillomandibular fixation (immobilization), short hospitalization, early commencement of mouth-opening exercise, and the formation of a large bony contact area regardless of mandibular setback or advancement.12 Thus, rigid fixation can improve postoperative skeletal stability.
Even though a large bony contact area can be obtained after SSRO with rigid fixation, the rigid fixation process can induce postoperative positional changes of the condyle in the fossa.13 Moreover, transverse rotation of the proximal segment is known to occur after rigid fixation.8 Such postoperative changes can have an adverse effect on skeletal stability. In fact, Kim et al.14 have reported that after SSRO, the proximal segments show various changes according to the osteosynthesis method. Among the various modes of rigid fixation, the bicortical screw method affected the largest extent of segment change. All these changes are potential factors that lead to postoperative skeletal relapse.
In order to overcome these drawbacks of absolute rigid fixation, the semi-rigid fixation method was introduced to stabilize the osteotomized fragments with sufficient flexibility for enabling bone healing. For example, Mavili et al.15 applied two bicortical screws for mandibular semi-rigid fixation. Baek and Lee16 reported that a semi-rigid plate with two 2-mm-diameter, oval-shaped sliding holes was relatively stable while being convenient. These previous reports, however, focused almost exclusively on maxillary and mandibular skeletal stability. Few studies have investigated the postoperative three-dimensional (3D) changes in the proximal and distal segments, and there is a dearth of comparative studies on the conventional mini-plate and semi-rigid sliding plate fixation methods during the healing period.
Therefore, the purpose of the present study was to evaluate the 3D changes in the proximal segments during the healing process both immediately (T0) and 6 months after (T1) mandibular setback SSRO, and to compare the conventional mini-plate and semi-rigid sliding plate fixation methods on the basis of those changes.
This retrospective study included data from 38 patients with skeletal Class III malocclusion (16 men and 22 women) who underwent mandibular setback SSRO with/without Le Fort I osteotomy at Pusan National University Dental Hospital (Yangsan, Korea) between December 2013 and March 2015. The exclusion criteria were the presence of any syndrome, cleft lip and/or palate, a history of trauma and temporomandibular disorder, facial asymmetry, and genioplasty. All of the patients received presurgical orthodontic treatment. The study was reviewed and approved by the Institutional Review Board of Pusan National University Dental Hospital (PNUDH-2015-024).
To reduce the pterygomasseteric sling extension for all of the patients, the proximal segments were stripped of the sling at the posterior and inferior parts. Bony segment fixation was achieved via the intra-oral approach. The patients were divided into two groups on the basis of the osteosynthesis method used (Table 1). For patients in group A (rigid fixation: mini-plate [Martin Medizintechnik, Tuttlingen, Germany]; 10 men and 10 women; mean age = 24.7 ± 5.3 years), four conventional 2.0 mm (diameter) × 6.0 mm (length) monocortical screws were installed in the middle of the mandibular body by using conventional 4-hole straight mini-plates. For patients in group B (semi-rigid fixation: sliding plate [Martin Medizintechnik]; 6 men and 12 women; mean age = 23.8 ± 5.2 years), three 2.0 mm × 6.0 mm monocortical screws were installed in the middle of the mandibular body by using 3-hole sliding plates (2 screws for the proximal segment and 1 for the distal segment). The two different fixation methods are shown in panoramic radiographs (Figure 1). For both groups, intermaxillary fixation was applied for 5-7 days by using a surgical splint, followed by physiotherapy involving muscle and mouth-opening exercises using elastic bands. One month after the surgery, orthodontic treatment was resumed, and 6 months after surgery, the mini-plates and sliding plates were removed.
Cone-beam computed tomography (CBCT) images (Pax-Zenith3D; Vatech Co., Seoul, Korea) were used to evaluate the postoperative 3D changes in the proximal segment during the healing process (T0–T1). For accurate measurement, the CBCT images were superimposed using the symphysis and the lower anterior mandible as references. On the superimposed CBCT volumes, the X, Y, and Z coordinates of the landmarks were identified (Figure 2) according to the following reference planes: the XY plane, centered on the B point (i.e., the origin: 0, 0, 0) and both mental foramina; the YZ plane, running perpendicular to the horizontal reference plane and passing through the B point and the mid-point of the mental foramina; and the XZ plane, running perpendicular to the horizontal and midsagittal reference planes and passing through the B point. On the superimposed 3D images, the positive directions for the X-, Y-, and Z-axes were the left, posterior, and superior, respectively.
The landmarks representing the postoperative 3D changes in the proximal segment were the following:
The 3D changes in the proximal segment were measured and calculated by referring to these landmarks. The percentage of samples with clinically significant (> 2 mm) and insignificant (< 2 mm) changes were also calculated.
The data were statistically analyzed using SPSS software ver. 12.0 (SPSS, Chicago, IL, USA). For determining the postoperative changes at all of the landmarks, paired t-testing was performed. The independent t-test was used to determine the intergroup differences (p < 0.05).
All of the variables were reassessed by the investigators at 2-week intervals. The systematic intra-examiner error between the two measurements was determined by means of a paired t-test. Additionally, the magnitude of that error was assessed by calculating the intraclass correlation coefficient (ICC). The intra- and inter-observer reliabilities of the 3D measurements were very good, with mean ICCs of 0.965 (95% confidence interval [CI], 0.800–0.999) and 0.892 (95% CI, 0.802–0.941), respectively. There were no statistically significant differences in the identification of the landmarks.
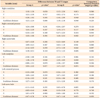
Patients in group B (3-hole sliding mini-plate) showed significant changes in the proximal segment. The condylion showed significant changes along the Z-axis on the right side and along the X-, Y-, and Z-axes on the left side (Table 2). The coronoid process showed significant changes along the Y-axis on the left side. The right screw hole showed significant changes along the Z-axis (p < 0.05). All of the right-side landmarks also showed significant changes in Euclidean distances (p < 0.05). However, patients in group A (4-hole mini-plate) showed no significant changes in any of the directions or Euclidean distances, except along the Y-axis for the left condylion. There were no statistically significant differences between groups A and B (p > 0.05, Table 2).
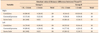
In group B, 10 of the 18 patients (55.6%) showed changes of 2 mm or more in Euclidean distances in right condylion (Table 3). Additionally, nine of the 18 patients (50.0%) and eight of the 18 patients (44.4%) showed changes of 2 mm or more in Euclidean distances in the right coronoid process and left condylion, respectively. As for all of the other landmarks, fewer than 40% of the patients showed changes of 2 mm or more in Euclidean distances.
Postoperative stability should be the main objective of orthognathic surgery, especially mandibular setback surgery. In order to enhance postoperative stability, rigid fixation is commonly employed, because it can reduce the intermaxillary fixation time, increase the surface area between the two segments, and hasten the commencement of mouth-opening exercises.12 However, rigid fixation can induce postoperative positional changes of the condyle in the fossa,13 as well as transverse rotation of the proximal segment.8 Such changes can have an adverse effect on skeletal stability. Moreover, the proximal segment exhibits various movements depending on the type of fixation method. The semi-rigid sliding plate has been suggested as a suitable option for fixation because it affords sufficient flexibility to the osteotomized bone fragments, thereby enabling faster bone healing.16 To date, however, semi-rigid fixation experiments have been limited to only exploring maxillary and mandibular skeletal stability. The present study, therefore, focused on comparing 3D changes in the proximal bone segments between semi-rigid sliding plate fixation and the conventional mini-plate fixation.
On CBCT images, the distal segments were superim-posed to compare the changes from T0 to T1 at three reference points: the condylion, coronoid process, and screw hole. The statistically significant results were the changes along the Y-axis in the left condylion and the Euclidean distances between the three reference points on the right side for the conventional mini-plate fixation and for sliding plate fixation, respectively. In particular, there were no statistically significant differences during T0–T1 between the conventional mini-plate fixation and sliding plate fixation. Because the average changes in each category were smaller than the standard deviation, the statistical differences within the two groups could be masked. As a limitation of this study, the small sample size could also affect this result.
Postoperative changes greater than 2 mm after mandibular setback SSRO are clinically important.17 In the present study, fewer than 30% of the patients showed changes greater than 2 mm for most of the landmarks in the conventional mini-plate fixation group. In the sliding plate fixation group, however, more than 40% of the patients showed changes greater than 2 mm in the left and right condylion and right coronoid process. Therefore, even though the two groups did not show any statistically significant relationships, many of the patients in the sliding plate fixation group showed clinically important changes. Moreover, while both the groups showed postero-inferior changes from the reference points, the most notable one was the postero-medio-inferior change of the condylion. In fact, in many patients in the sliding plate group, the condylion and coronoid process showed postoperative postero-medio-inferior movement. Although the screw hole also showed postero-inferior movement, the number of patients with such movement was lesser than that of patients with movement in the condylion and coronoid process. This finding could be attributed to the fact that the screw hole was closer to the fixation sites on the proximal and distal segments than was the condylion or coronoid process.
Numerous previous finite element analysis studies have examined the fixation of varyingly shaped mini-plates and different numbers of screws. These studies have shown that as the distance between the proximal and distal segments increases, so does the postoperative gap, which eventually leads to relapse.18 The mechanism underlying this result is the increasing torsional stress on segment-connecting plates incurred as the distance between them increases, which, in turn, results in increased plate bending. This explanation also correlates with the finding of a previous study that emphasized the importance of reducing torsional stress to increase stability between segments.19 In the present study, the use of three screws for the sliding plate resulted in an increased inter-screw distance between the distal and proximal segments. This increased distance induced torsional stress that caused plate bending, and, ultimately, antero-medio-inferior movement of the condylion, which was the reference point farthest from the plate. It should be emphasized that many reference points showed changes over 2 mm caused by sliding plates; this, however, was not due to the sliding plate allowing sliding, but rather to the increase in the inter-screw distance resulting from plate bending. Therefore, the distal hole of the sliding plate need not be oval-shaped. It should also be stressed that in order to prevent the sliding plate from bending during the postoperative healing period, intermaxillary elastics should be employed.
Despite the above-mentioned noteworthy findings, the current study has two limitations: 1) a small sample size and 2) patient enrollment from a single center. Furthermore, there might have been a selection bias while dividing the patients into the two groups. Considering these are all limitations of the retrospective study design, multi-center randomized controlled studies with large sample sizes should be conducted in the future to overcome these shortcomings.
There were no statistically significant differences between the conventional mini-plate and sliding plate with respect to changes in the proximal segment from T0 to T1. With the sliding plate, however, the inter-screw distance seemed to increase between the distal and proximal segments; this induced torsional stress causing plate torsion and bending. Moreover, compared to the conventional mini-plate group, the semi-rigid sliding plate group had more landmarks with changes greater than 2 mm. In order to prevent torsion and bending of the sliding plate, it is recommended that clinicians use intermaxillary elastics during the postoperative healing period.
Figures and Tables
Figure 1
Two different fixation methods. A, Rigid fixation with a mini-plate; B, semi-rigid fixation with a sliding mini-plate.

Notes
References
1. Dolce C, Van Sickels JE, Bays RA, Rugh JD. Skeletal stability after mandibular advancement with rigid versus wire fixation. J Oral Maxillofac Surg. 2000; 58:1219–1227.

2. Mobarak KA, Krogstad O, Espeland L, Lyberg T. Long-term stability of mandibular setback surgery: a follow-up of 80 bilateral sagittal split osteotomy patients. Int J Adult Orthodon Orthognath Surg. 2000; 15:83–95.
3. Costa F, Robiony M, Sembronio S, Polini F, Politi M. Stability of skeletal Class III malocclusion after combined maxillary and mandibular procedures. Int J Adult Orthodon Orthognath Surg. 2001; 16:179–192.
4. Kim MJ, Kim SG, Park YW. Positional stability following intentional posterior ostectomy of the distal segment in bilateral sagittal split ramus osteotomy for correction of mandibular prognathism. J Craniomaxillofac Surg. 2002; 30:35–40.

5. Borstlap WA, Stoelinga PJ, Hoppenreijs TJ, van't Hof MA. Stabilisation of sagittal split advancement osteotomies with miniplates: a prospective, multicentre study with two-year follow-up. Part III--condylar remodelling and resorption. Int J Oral Maxillofac Surg. 2004; 33:649–655.

6. Politi M, Costa F, Cian R, Polini F, Robiony M. Stability of skeletal class III malocclusion after combined maxillary and mandibular procedures: rigid internal fixation versus wire osteosynthesis of the mandible. J Oral Maxillofac Surg. 2004; 62:169–181.

7. Rhee CH, Choi YK, Kim YI, Kim SS, Park SB, Son WS. Correlation between skeletal and dental changes after mandibular setback surgery-first orthodontic treatment: Cone-beam computed tomography-generated half-cephalograms. Korean J Orthod. 2015; 45:59–65.

8. Proffit WR, Phillips C, Dann C 4th, Turvey TA. Stability after surgical-orthodontic correction of skeletal Class III malocclusion. I. Mandibular setback. Int J Adult Orthodon Orthognath Surg. 1991; 6:7–18.
9. Joss CU, Vassalli IM. Stability after bilateral sagittal split osteotomy setback surgery with rigid internal fixation: a systematic review. J Oral Maxillofac Surg. 2008; 66:1634–1643.

10. Wolford LM. Concomitant temporomandibular joint and orthognathic surgery. J Oral Maxillofac Surg. 2003; 61:1198–1204.

11. Son S, Kim SS, Son WS, Kim YI, Kim YD, Shin SH. Miniscrews versus surgical archwires for intermaxillary fixation in adults after orthognathic surgery. Korean J Orthod. 2015; 45:3–12.

12. Law JH, Rotskoff KS, Smith RJ. Stability following combined maxillary and mandibular osteotomies treated with rigid internal fixation. J Oral Maxillofac Surg. 1989; 47:128–136.

13. Stroster TG, Pangrazio-Kulbersh V. Assessment of condylar position following bilateral sagittal split ramus osteotomy with wire fixation or rigid fixation. Int J Adult Orthodon Orthognath Surg. 1994; 9:55–63.
14. Kim YI, Park SB, Jung YH, Hwang DS, Lee JY. Evaluation of intersegmental displacement according to osteosynthesis method for mandibular setback sagittal split ramus osteotomy using cone-beam computed tomographic superimposition. J Oral Maxillofac Surg. 2012; 70:2893–2898.

15. Mavili ME, Canter HI, Saglam-Aydinatay B. Semirigid fixation of mandible and maxilla in orthognathic surgery: stability and advantages. Ann Plast Surg. 2009; 63:396–403.
16. Baek RM, Lee SW. A new condyle repositionable plate for sagittal split ramus osteotomy. J Craniofac Surg. 2010; 21:489–490.

17. Proffit WR, Phillips C, Turvey TA. Stability after mandibular setback: mandible-only versus 2-jaw surgery. J Oral Maxillofac Surg. 2012; 70:e408–e414.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download